Brain Diseases
neurocognitive disorder (NCD)
Any of a number of brain diseases that affects a person’s ability to remember, analyze, plan, or interact with other people.
Most older people are less sharp than they were, but they still think and remember quite well. Others experience serious decline. They have a neurocognitive disorder (NCD).
The Ageism of Words
The rate of neurocognitive disorders increases with every decade after age 60. But ageism distorts and exaggerates that fact. To understand and prevent NCDs, we need to begin by using words carefully.

Download the DSM-5 Appendix to learn more about the terminology and classification of brain diseases in late adulthood.
Senile simply means “old.” If the word senility is used to mean severe mental impairment, that implies that old age always brings intellectual failure—
The DSM-
Memory problems occur in every cognitive disorder, although some people with NCDs have other notable symptoms, such as in judgment (they do foolish things) and moods (they are suddenly rageful or tearful). The line between normal age-
The former word—
to ignore the subjectivity and quality of life of those who are suffering dementia, and to stigmatize, devalue, disempower, banish, objectify, and invalidate them on account of their neuropathological condition.
[George & Whitehouse, 2010, p. 351]
In Japanese, the traditional word for neurocognitive disorder was chihou, translated as “foolish” or “stupid.” As more Japanese reached old age, a new word, ninchihou, which means “cognitive syndrome,” was chosen (George & Whitehouse, 2010). That is far better, for, as you remember with Down syndrome, a syndrome is a cluster of characteristics, with each person somewhat different.
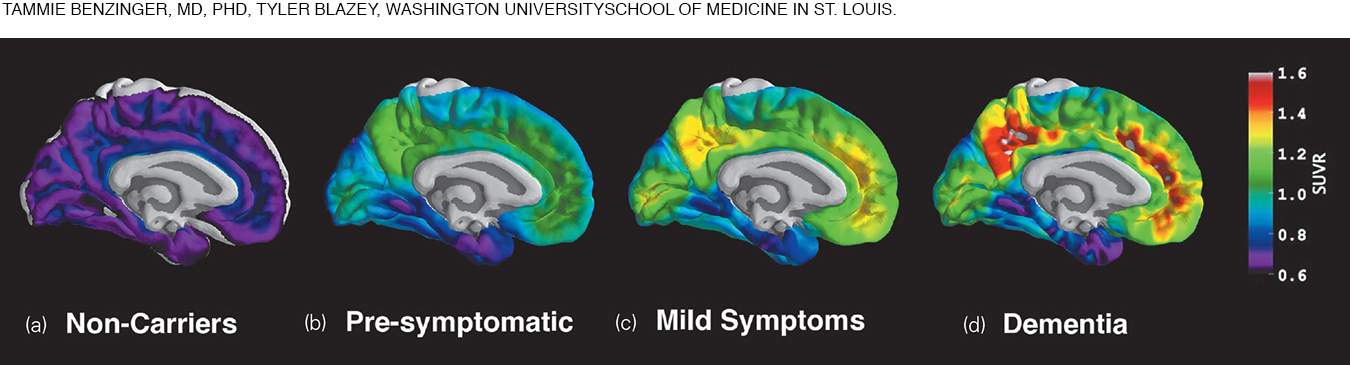
Many scientists seek biological indicators (called biomarkers, such as in the blood or cerebrospinal fluid) or brain indicators (as on brain scans) that predict major memory loss. However, although abnormal scores on many tests (biological, neurological, or psychological) indicate possible problems, an examination of 24 such measures found that no single test, or combination of tests, is 100-
One new and promising test, a PET scan that reveals amyloid plaques which indicate Alzheimer’s disease, is not reimbursed by Medicaid because the link between presence of amyloid and effective treatment is “insufficient.” More research is needed (Centers for Medicare and Medicaid Services, 2014).
Prevalence of NCDs
How many people suffer from neurocognitive disorders in their older years? To answer this question, researchers selected a representative sample of people over age 69 from every part of the United States. Each was interviewed and tested. Then the researchers interviewed someone who knew the elder well (usually an immediate relative). This information was combined with medical records and clinical judgment.
major neurocognitive disorder (major NCD)
Irreversible loss of intellectual functioning caused by organic brain damage or disease. Formerly called dementia, major NCD becomes more common with age, but it is abnormal and pathological even in the very old.
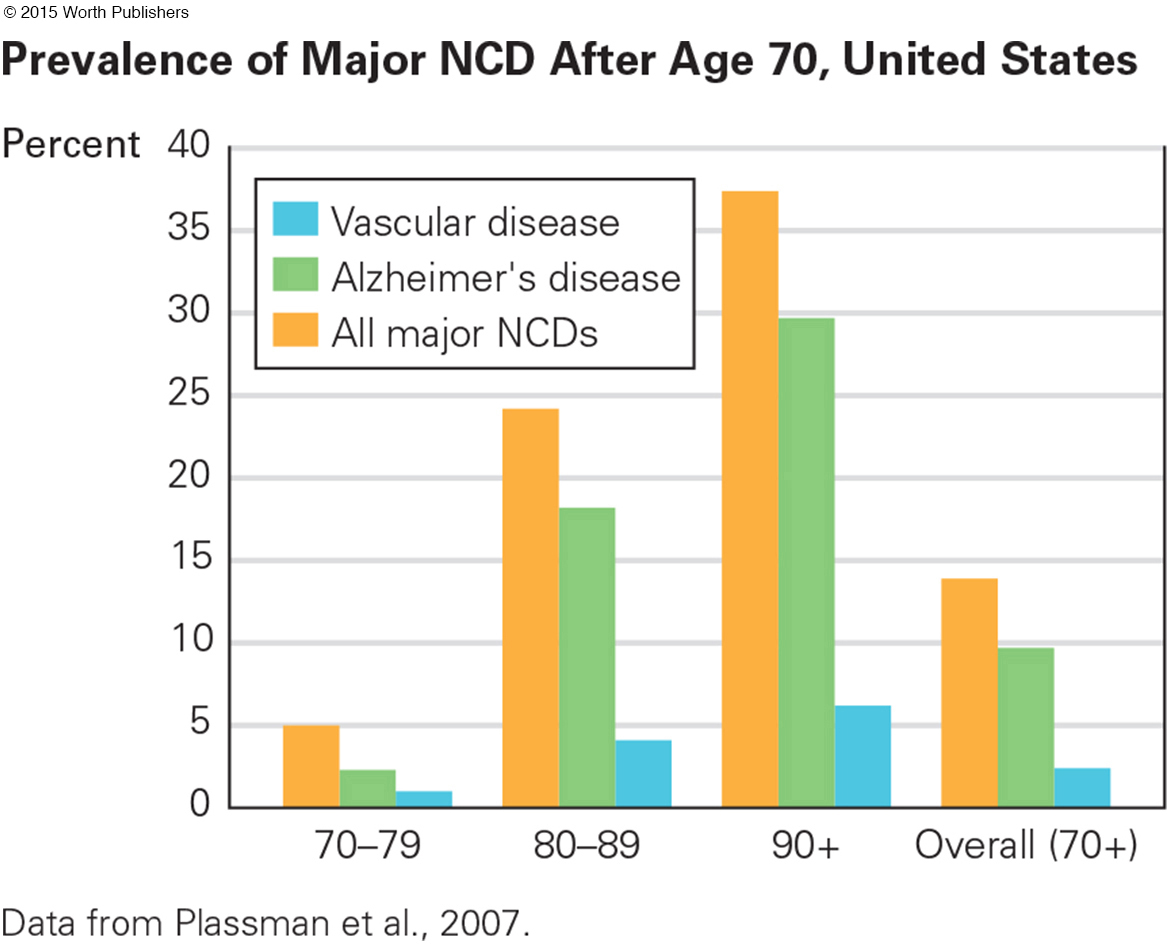
The conclusion was that 14 percent of the elders had some form of neurocognitive disorder (Plassman et al., 2007) (see Figure 14.6). Extrapolated to the overall population, that means that about 4 million U.S. residents have a serious neurocognitive disorder. Another study, this one of people already diagnosed with major neurocognitive disorder, found much lower rates, about 8 percent of the aged population (Koller & Bynum, 2014). The discrepancy may be that many people are not diagnosed, or that the rate has decreased.
An estimated 47 million people (again, estimates vary from 35 million to 60 million) are affected worldwide, 60 percent of them in low-
Eventually, better education and public health will reduce the rate (if not the n-
The Many Neurocognitive Disorders
As more is learned, it has become apparent that there are many types of brain disease, with each beginning in a distinct part of the brain and having particular symptoms. Once it was thought that if a person seemed to have a good memory, he or she could not be suffering from a neurocognitive disorder. That mistaken idea prevented diagnosis and treatment. Accordingly, we describe some of the many disorders now.
Alzheimer’s disease (AD)
The most common cause of major NCD, characterized by gradual deterioration of memory and personality and marked by the formation of plaques of beta-

In Video Activity: Alzheimer’s Disease, experts and family members discuss the progression of the disease.
ALZHEIMER’S DISEASE In the past century, millions of people in every large nation have been diagnosed with Alzheimer’s disease (AD), (now formally referred to as major NCD due to Alzheimer’s disease). Severe and worsening memory loss is the main symptom, but the diagnosis is not definitive until an autopsy finds extensive plaques and tangles in the cerebral cortex.
plaques
Clumps of a protein called beta-
tangles
Twisted masses of threads made of a protein called tau within the neurons of the brain.
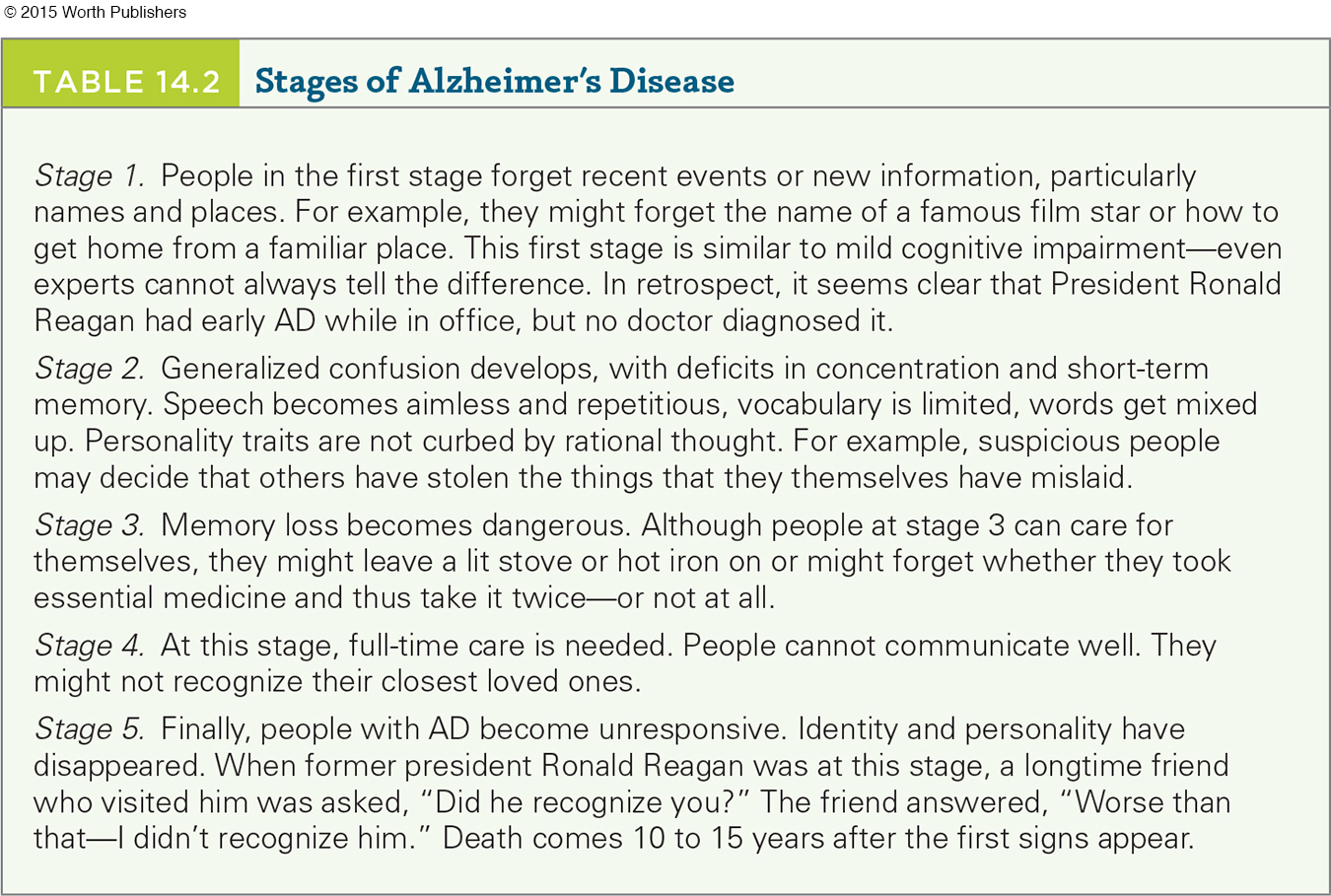
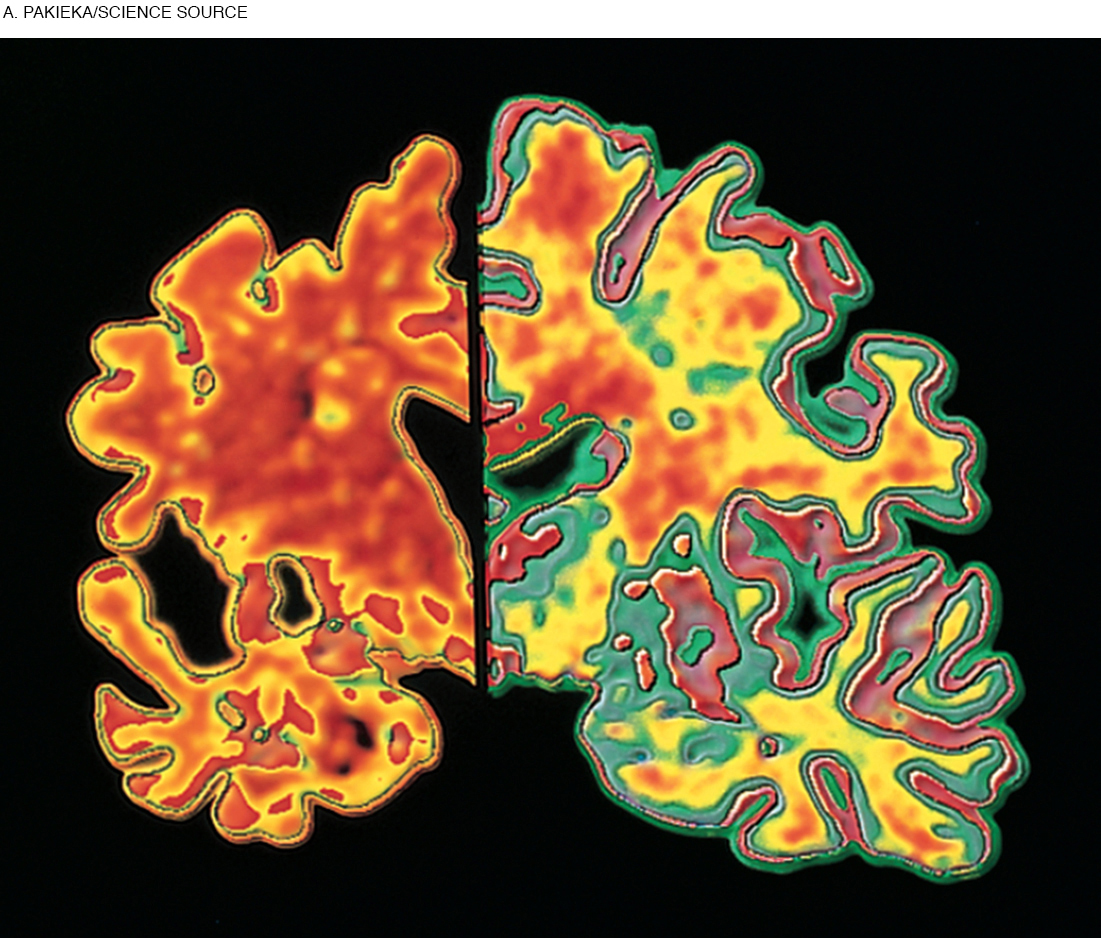
Plaques are clumps of a protein called beta-
An autopsy that finds massive plaques and tangles proves that a person had Alzheimer’s disease. However, between 20 and 30 percent of cognitively normal elders have, at autopsy, extensive plaques in their brains (Jack et al., 2009). One explanation is that cognitive reserve enables some people to bypass the disconnections caused by plaques. Education does seem to prevent, or modify, AD (Langa, 2015).
Alzheimer’s disease is partly genetic. If it develops in middle age, the affected person either has trisomy-
Most cases begin much later, at age 75 or so. Many genes have some impact, including SORL1 and ApoE4 (allele 4 of the ApoE gene). People who inherit one copy of ApoE4 (as about one-
VASCULAR DISEASE The second most common cause of neurocognitive disorder is a stroke (a temporary obstruction of a blood vessel in the brain) or a series of strokes, called transient ischemic attacks (TIAs, or ministrokes). The interruption in blood flow reduces oxygen, destroying part of the brain. Symptoms (blurred vision, weak or paralyzed limbs, slurred speech, and mental confusion) suddenly appear.
vascular disease
Formerly called vascular or multi-
In a TIA, symptoms may vanish quickly, unnoticed. However, unless recognized and prevented, another TIA is likely, eventually causing vascular disease, commonly referred to as vascular or multi-
Vascular disease also correlates with the ApoE4 allele (Cramer & Procaccio, 2012). For some of the elderly, it is caused by surgery that requires general anesthesia. They suffer a ministroke, which, added to reduced cognitive reserve, damages their brains (Stern, 2013).
frontotemporal NCDs
Brain disorders that occur with serious impairment of the frontal lobes. (Also called frontotemporal lobar degeneration.)
FRONTOTEMPORAL NCDS Several types of neurocognitive disorders affect the frontal lobes and thus are called frontotemporal NCDs, or frontotemporal lobar degeneration (Pick disease is the most common form). These disorders cause perhaps 15 percent of all cases of NCDs in the United States. Frontotemporal NCDs tend to occur under age 70, unlike Alzheimer’s or vascular disease (Seelaar et al., 2011).
In frontotemporal NCDs, parts of the brain that regulate emotions and social behavior (especially the amygdala and prefrontal cortex) deteriorate. Emotional and personality changes are the main symptoms (Seelaar et al., 2011). A loving mother with a frontotemporal NCD might reject her children, or a formerly astute businessman might invest in a hare-
Frontal lobe problems may be worse than more obvious types of neurocognitive disorders, in that compassion, self-
threw away tax documents, got a ticket for trying to pass an ambulance and bought stock in companies that were obviously in trouble. Once a good cook, he burned every pot in the house. He became withdrawn and silent, and no longer spoke to his wife over dinner. That same failure to communicate got him fired from his job.
[Grady, 2012, p. A1]
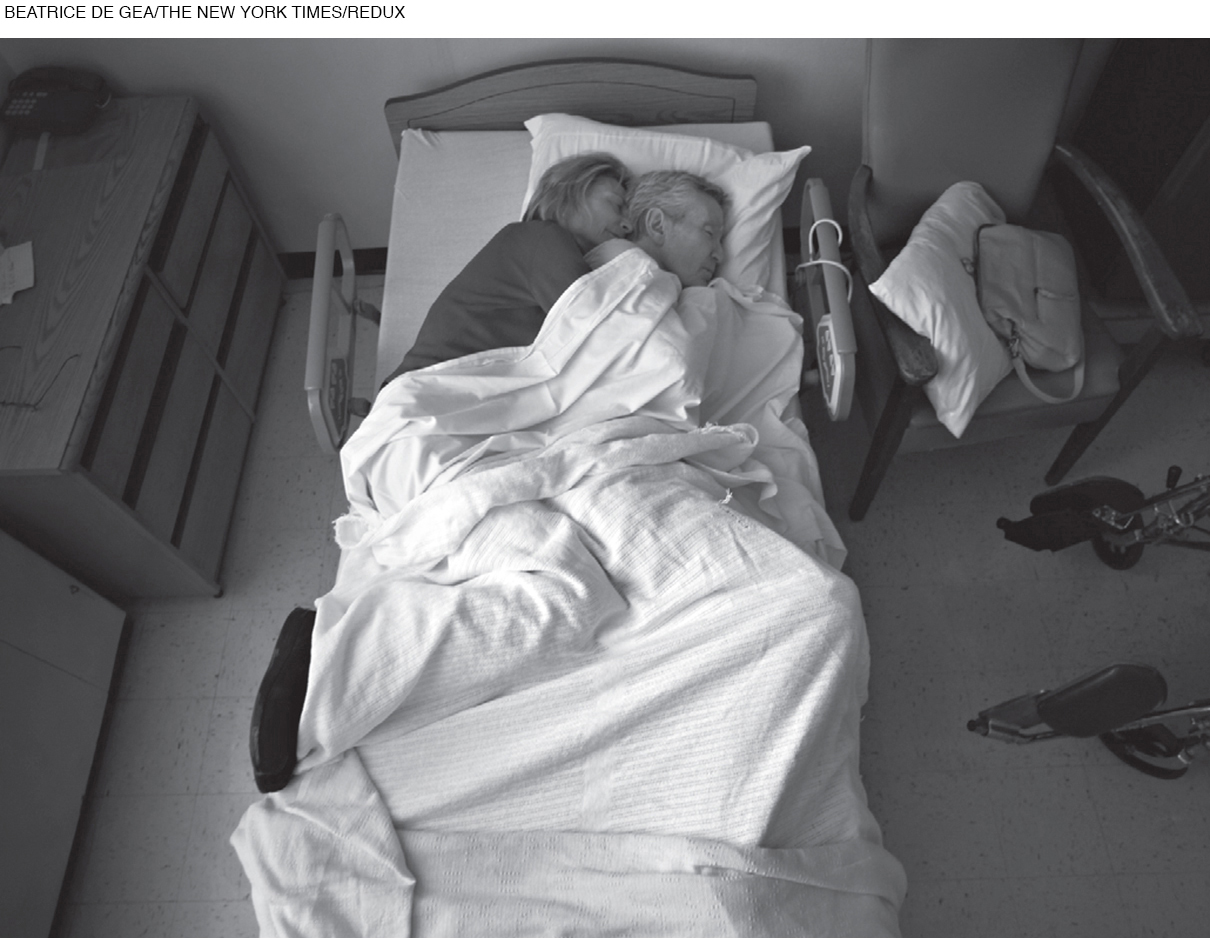
Finally, he was diagnosed with a frontotemporal NCD. Ruth asked him to forgive her fury. It is not clear that he understood either her anger or her apology. (See photo.)
Parkinson’s disease
A chronic, progressive disease that is characterized by muscle tremor and rigidity and sometimes major NCD; caused by reduced dopamine production in the brain.
Although there are many forms and causes of frontotemporal NCDs—
OTHER DISORDERS Many other brain diseases begin with impaired motor control (shaking when picking up a coffee cup, falling when trying to walk), not with impaired thinking. The most common of these is Parkinson’s disease, the cause of about 3 percent of all cases of NCDs.
Parkinson’s disease starts with rigidity or tremor of the muscles as dopamine-
Older people with Parkinson’s develop cognitive problems sooner (Pfeiffer & Bodis-
Lewy body disease
A form of major NCD characterized by an increase in particular abnormal cells in the brain. Symptoms include visual hallucinations, momentary loss of attention, falling, and fainting.
Another 3 percent of people with NCD in the United States suffer from Lewy body disease: excessive deposits of a particular kind of protein in their brains. Lewy bodies are also present in Parkinson’s disease, but in Lewy body disease they are more numerous and dispersed throughout the brain, interfering with communication between neurons. The main symptom is loss of inhibition: A person might gamble or become hypersexual.

Comorbidity is common with all these disorders. For instance, most people with Alzheimer’s disease also show signs of vascular impairment (Doraiswamy, 2012). Parkinson’s, Alzheimer’s, and Lewy body diseases can occur together: People who have all three experience more rapid and severe cognitive loss (Compta et al., 2011).
Some other types of NCDs begin in middle age or even earlier, caused by Huntington’s disease, multiple sclerosis, a severe head injury, or the last stages of syphilis, AIDS, or bovine spongiform encephalopathy (BSE, or mad cow disease). Repeated blows to the head, even without concussions, can cause chronic traumatic encephalopathy (CTE), which first causes memory loss and emotional changes (Voosen, 2013).
Although the rate of systemic brain disease increases dramatically with every decade after age 60, brain disease can occur at any age, as revealed by the autopsies of a number of young professional athletes. For them, prevention includes better helmets and fewer body blows. Already, tackling is avoided in football practice.
These changes in athletic practices have come too late for thousands of adults, including Derek Boogaard, a National Hockey League enforcer who died of a drug overdose in 2011 at age 28. His autopsied brain showed traumatic brain injury, now called CTE.
For Boogaard, chronic traumatic encephalopathy may have been a cause of drug addiction and would have become major NCD if he lived longer. The brain disorder probably already occurred, undiagnosed. Another hockey player said of him, “His demeanor, his personality, it just left him . . . He didn’t have a personality anymore” (John Scott, quoted in Branch, 2011, p. B13). Obviously, senility is not a synonym for neurocognitive disorder.
Preventing Impairment
Severe brain damage cannot be reversed, although the rate of decline and some of the symptoms can be treated. However, education, exercise, and good health not only ameliorate mild losses, they may prevent worse ones. That may be happening: “A growing number of studies, at least nine over the past 10 years, have shown a declining risk for dementia incidence or prevalence in high-
Because brain plasticity is lifelong, exercise that improves blood circulation not only prevents cognitive loss but also builds capacity and repairs damage. The benefits of exercise have been repeatedly cited in this text. Now we simply reiterate that physical exercise—
Question 14.26
OBSERVATION QUIZ
What three things do you see that promote cognitive health?
Social interaction, appreciation of nature, and, of course, exercise. Doing leg lifts alone at home is good too, but this is much better.

Medication to prevent stroke also protects against neurocognitive disorders. In a Finnish study, half of a large group of older Finns were given drugs to reduce lipids in their system (primarily cholesterol). Years later, fewer of them had developed NCDs than did a comparable group who were not given the drug (Solomon et al., 2010).
Avoiding specific pathogens is critical. For example, beef can be tested to ensure that it does not have BSE, condoms can protect against HIV/AIDS, and syphilis can be cured with antibiotics.
For most neurocognitive disorders, however, despite the efforts of thousands of scientists and millions of older people, no foolproof prevention or cure has been found. Avoiding toxins (lead, aluminum, copper, and pesticides) or adding supplements (hormones, aspirin, coffee, insulin, antioxidants, red wine, blueberries, and statins) have been tried as preventatives but have not proven effective in controlled, scientific research.
Thousands of scientists have sought to halt the production of beta-
Early, accurate diagnosis years before obvious symptoms appear leads to more effective treatment. Drugs do not cure NCDs, but some slow progression. Sometimes surgery or stem cell therapy is beneficial. The U.S. Pentagon estimates that more than 200,000 U.S. soldiers who were in Iraq or Afghanistan suffered traumatic brain injury, predisposing them to major NCD before age 60 (G. Miller, 2012). Measures to remedy their brain damage may help the civilian aged as well.
Among professionals, hope is replacing despair. Earlier diagnosis seems possible; many drug and lifestyle treatments are under review. “Measured optimism” (Moye, 2015, p. 331) comes from contemplating the success that has been achieved in combating other diseases. Heart attacks, for instance, were once the leading cause of death for middle-

Reversible Neurocognitive Disorder?
Care improves when everyone knows that a disease is undermining intellectual capacity. Accurate diagnosis is even more crucial when memory problems do not arise from a neurocognitive disorder. Brain diseases destroy parts of the brain, but some people are thought to be permanently “losing their minds” when a reversible condition is really at fault.
DEPRESSION The most common reversible condition that is mistaken for major NCD is depression. Normally, older people tend to be quite happy; frequent sadness or anxiety is not normal. Ongoing, untreated depression increases the risk of major NCD (Y. Gao et al., 2013).
Ironically, people with untreated anxiety or depression may exaggerate minor memory losses or refuse to talk. Quite the opposite reaction occurs with early Alzheimer’s disease, when victims are often surprised when they cannot answer questions, or with Lewy body disease or frontotemporal NCDs, when people talk too much without thinking.
Specifics provide other clues. People with neurocognitive loss might forget what they just said, heard, or did because current brain activity is impaired, but they might repeatedly describe details of something that happened long ago. The opposite may be true for emotional disorders, when memory of the past is impaired but short-
NUTRITION Malnutrition and dehydration can also cause symptoms that may seem like brain disease. The aging digestive system is less efficient but needs more nutrients and fewer calories. This requires new habits, less fast food, and more grocery money (which many do not have).
Some elderly people deliberately drink less because they want to avoid frequent urination, yet adequate liquid in the body is needed for cell health. Since homeostasis slows with age, older people are less likely to recognize and remedy their hunger and thirst, and thus they may inadvertently impair their cognition.
Beyond the need to drink water and eat vegetables, several specific vitamins have been suggested as decreasing the rate of major NCD. Among the suggested foods to add are those containing antioxidants (C, A, E) and vitamin B-
Obviously, any food that increases the risk of heart disease and stroke also increases the risk of vascular disease. In addition, some prescribed drugs destroy certain nutrients, although specifics require more research (Jyrkkä et al., 2012).
Indeed, well-
polypharmacy
Refers to a situation in which people take many medications. The various side effects and interactions of those medications can result in NCD symptoms.
POLYPHARMACY At home as well as in the hospital, most elderly people take numerous drugs—
The rate of polypharmacy is increasing in the United States. For instance, in 1988 the number of people over age 65 who took five drugs or more was 13 percent; by 2010 that number had tripled to 39 percent (Charlesworth et al., 2015).
Unfortunately, recommended doses of many drugs are determined primarily by clinical trials with younger adults, for whom homeostasis usually eliminates excess medication (Herrera et al., 2010). When homeostasis slows down, excess may linger. In a-
The average elderly person in the United States sees a physician eight times a year (National Center for Health Statistics, 2014). Typically, each doctor follows “clinical practice guidelines,” which are recommendations for one specific condition. A “-prescribing cascade” (when many interacting drugs are prescribed) may occur.
In one disturbing case, a doctor prescribed medication to raise his patient’s blood pressure, and another doctor, noting the raised blood pressure, prescribed a drug to lower it (McLendon & Shelton, 2011–
A related problem is that people of every age forget when to take which drugs (before, during, or after meals? after dinner or at bedtime?) (Bosworth & Ayotte, 2009). Short-
Even when medications are taken as prescribed and the right dose reaches the bloodstream, drug interactions can cause confusion and memory loss. Cognitive side effects can occur with almost any drug, but especially with drugs intended to reduce anxiety and depression.
Finally, following recommendations from the radio, friends, and television ads, many of the elderly try supplements, compounds, and herbal preparations that contain mind-
The solution seems simple: Discontinue drugs. However, that may increase both disease and cognitive decline. One expert warns of polypharmacy but adds that “-underuse of medications in older adults can have comparable adverse effects on quality of life” (Miller, 2011–
For instance, untreated diabetes and hypertension cause cognitive loss. Lack of drug treatment for those conditions may be one reason why low-
THINK CRITICALLY: Who should decide what drugs a person should take—
Obviously, money complicates the issue: Prescription drugs are expensive, which increases profits for drug companies, but they can also reduce surgery and hospitalization, thus saving money. As one observer notes, the discussion about spending for prescription drugs is highly polarized, emotionally loaded, with little useful debate. A war is waged over the cost of prescriptions for older people, and it is a “gloves-
WHAT HAVE YOU LEARNED?
Question 14.27
1. What brain diseases or conditions correlate with loss of cognition?
Neurocognitive disorders (NCDs) impair intellectual functioning caused by organic brain damage or disease. NCDs may be diagnosed as major or mild, depending on the severity of symptoms. Specific NCDs include Alzheimer’s disease, vascular disease, and frontotemporal NCDs. Loss of cognition can also be associated with disorders such as Parkinson’s disease.
Question 14.28
2. How does changing terminology reflect changing attitudes?
Ageism is revealed in the older terminology surrounding neurocognitive disorders. Senile simply means “old,” but senility suggests severe mental impairment, which implies that old age always brings intellectual failure—
Question 14.29
3. How does exercise affect the brain?
Exercise that improves blood circulation not only prevents cognitive loss but also builds capacity and repairs damage.
Question 14.30
4. What changes in the prevalence of neurocognitive disorders have occurred in recent years?
While the poorest nations have the lowest rates of major NCD, rates rise as public health, better education, and prosperity lead to increases in longevity. This has already occurred in China, where 9 million people had a major NCD in 2010, compared to only 4 million in 1990. Eventually, better education and public health will reduce the rate (if not the number) of cognitive impairments everywhere. In England and Wales the rate of major NCD for people over age 65 was 8.3 percent in 1991 but only 6.5 percent in 2011. Sweden had a similar decline.
Question 14.31
5. What indicates that Alzheimer’s disease is partly genetic?
Alzheimer’s disease is partly genetic. If it develops in middle age, the affected person either has trisomy-
Question 14.32
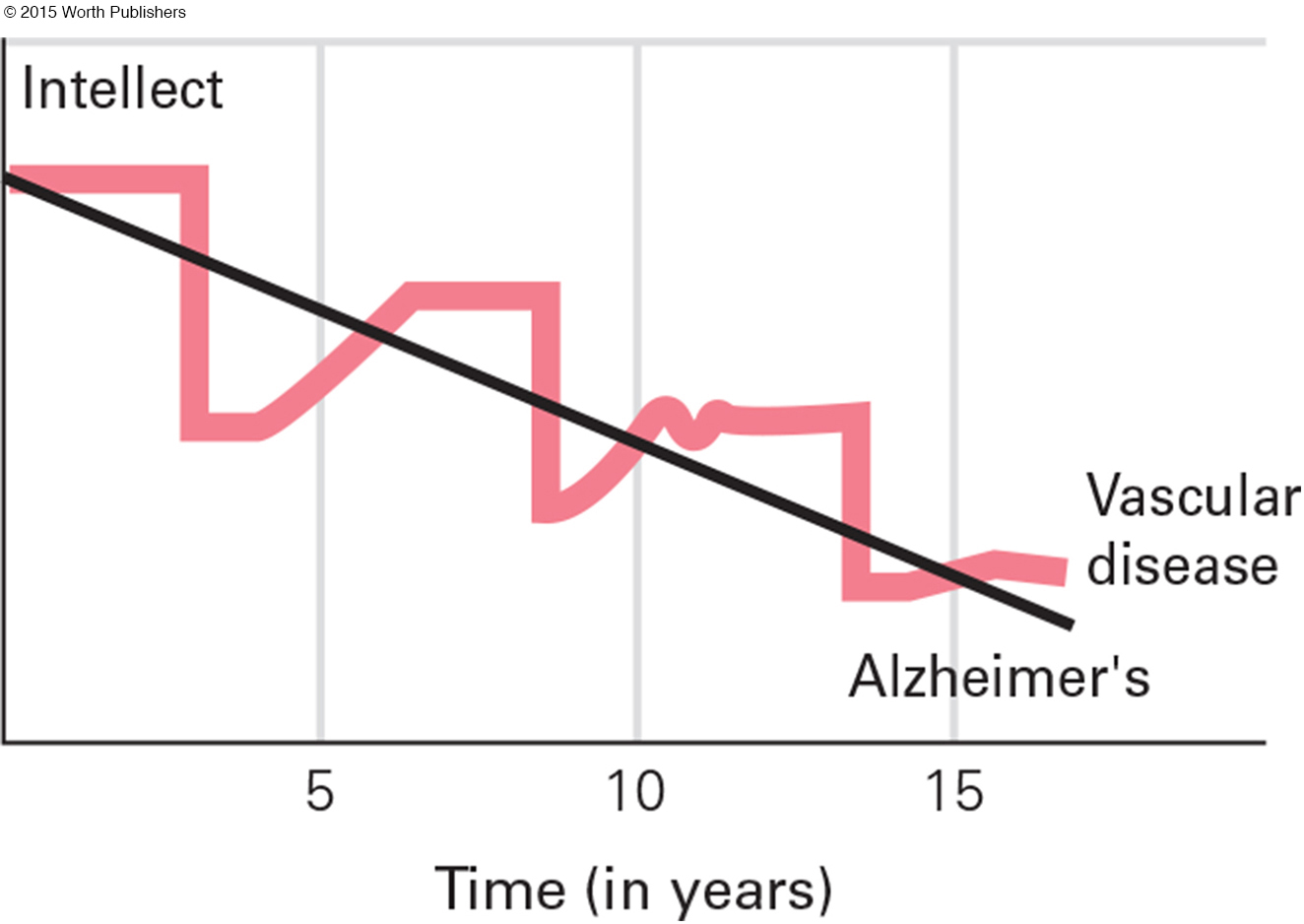
6. How does the progression of Alzheimer’s differ from vascular disease?
People may be unaware of the early stages of vascular disease because symptoms may vanish quickly and thus go unnoticed. The progression of Alzheimer’s disease is gradual, whereas the symptoms of vascular disease suddenly appear.
Question 14.33
7. In what ways are frontotemporal NCDs worse than Alzheimer’s disease?
In addition to the fact that they tend to affect people who are under age 70, frontotemporal NCDs may be worse than other types of NCDs because compassion, self-
Question 14.34
8. Why is Lewy body disease sometimes mistaken for Parkinson’s disease?
Lewy bodies are also present in Parkinson’s disease, but in Lewy body disease they are more numerous and dispersed throughout the brain, interfering with communication between neurons.
Question 14.35
9. How successful are scientists at preventing major NCD?
Among professionals, hope is replacing despair. Earlier diagnosis seems possible; many drug and lifestyle treatments are under review. Early, accurate diagnosis, years before obvious symptoms appear, leads to more effective treatment.
Question 14.36
10. What is the relationship between depression, anxiety, and neurocognitive disorders?
Ongoing, untreated depression increases the risk of major NCD, but the symptoms of both depression and anxiety are often opposite the symptoms of neurocognitive disorders. While people with untreated anxiety or depression may exaggerate minor memory losses or refuse to talk, those with early Alzheimer’s disease are often surprised when they cannot answer questions, and those with Lewy body disease or frontotemporal NCDs may talk too much without thinking.
Question 14.37
11. Why is polypharmacy particularly common among the elderly?
Because the average elderly person in the United States sees a physician more frequently than younger adults, a prescribing cascade (when many interacting drugs are prescribed) may occur. A related problem is that people of every age forget when to take which drugs. Finally, following recommendations from the radio, friends, and television ads, many of the elderly try supplements, compounds, and herbal preparations that contain mind-