 Aging and Disease
Aging and Disease
As you know from Chapters 17 and 20, with each passing decade homeostasis takes longer and allostatic load builds. Skin, hair, and body shape show unmistakable signs of senescence, while every internal organ ages. A stress to which younger bodies quickly adjust, such as a string of hot days or extra effort shoveling snow, could be lethal for the old.
Primary and Secondary Aging
primary aging The universal and irreversible physical changes that occur to all living creatures as they grow older.
secondary aging The specific physical illnesses or conditions that become more common with aging but are caused by health habits, genes, and other influences that vary from person to person.
Gerontologists distinguish between primary aging, which involves universal changes that occur with the passage of time, and secondary aging, which are the consequences of particular inherited weaknesses, chosen health habits, and environmental conditions. One researcher explains:
Primary aging is defined as the universal changes occurring with age that are not caused by diseases or environmental influences. Secondary aging is defined as changes involving interactions of primary aging processes with environmental influences and disease processes.
[Masoro, 2006, p. 46]
Primary aging does not directly cause illness, but it makes almost every disease more likely. The combination of primary and secondary aging causes morbidity and mortality.
For example, with age the heart pumps more slowly and the vascular network is less flexible, increasing the risk of stroke and heart attack. The lungs take in and expel less air with each breath, so that blood oxygen is reduced and chronic obstructive pulmonary disease is more common. Digestion slows. The kidneys become less efficient, increasing problems if people become dehydrated because they drink less—
Furthermore, because of age, healing takes longer when an illness or an accident occurs. That is why young adults who contract pneumonia usually recover completely in a few weeks, but in the very old pneumonia can overwhelm a weakened body. Indeed, pneumonia often is listed as the cause of death for the oldest-
The same is true for accidents of all kinds, from falls, crashes, fires, and poisons. Younger people are much more likely to recover from such insults, but 41 million people in the United States over age 65 died accidentally in 2010, making the accidental death rate for the elderly higher than for people of any other age (National Center for Health Statistics, 2012).
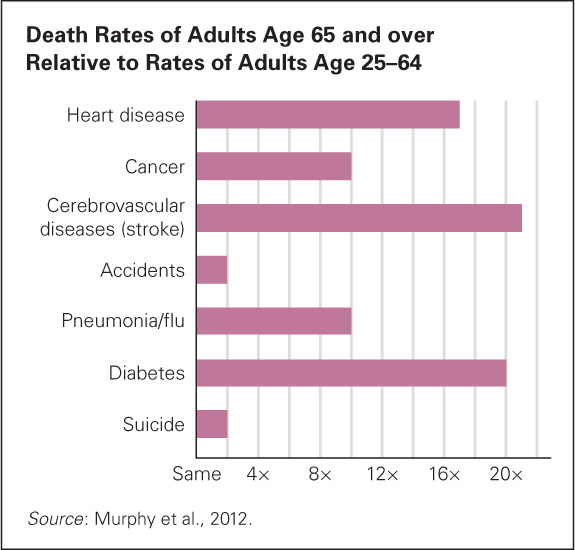
FIGURE 23.5
More Years to Live Even compared with a decade ago, fewer people die before age 65, which means that, for many causes, death is far more likely in old age. Most of the underlying conditions for these diseases were present in middle age.The data in the previous paragraph may bewilder you, since you learned in earlier chapters that more children, adolescents, and emerging adults die of accidents than of any other cause. The explanation centers on other causes of death. Because heart disease, cancers, strokes, and so on are rare earlier in life but common in late adulthood, accidents are the first cause of death from age 1 to 44 but only the eighth after age 65. Older people are more cautious than younger ones, but when injury occurs, death is more likely after age 65.
A developmental view of the relationship between primary and secondary aging harkens back to the lifelong toll of stress, as explained in Chapters 17 and 21. Allostatic load is measured by 10, or sometimes 16, biomarkers—
Thus, measurement of allostatic load assesses the combined, long-
Treatment of the Elderly: Examples—Flu and Hypertension
Because of primary aging, medical intervention affects the old differently than the young. For this reason, drugs, surgeries, and so on that have been validated on young adults may be less effective on the elderly. Two examples are treatments for flu and hypertension, or high blood pressure.
The specific strains of flu that circulate are slightly different each year, so the vaccine is redesigned annually to fight whatever strains are predicted. That’s why people need flu shots every fall for the following winter. Annual immunization is particularly recommended for those over age 65, because their other infirmities make flu sometimes fatal.
The 2012–
The importance of considering age when designing disease prevention is also apparent with medication to reduce hypertension. If systolic blood pressure in a middle-
Surprisingly, for some of the elderly, hypertension is protective; drugs may increase the risk of death, not decrease it. When physicians decide whether to prescribe pressure-
Variation in hypertension may be one reason that anesthesia may damage an older person’s brain or cause the heart to stop. Drugs to reduce pain may also affect the elderly differently from the young. That may explain why temporary hallucinations and delirium after surgery are far more common for the old than for the young.
Chronic and Acute Disease: Example—The Heart
acute illness An illness that is sudden and severe.
chronic illness An illness that begins gradually and is ongoing.
It is important to understand the distinction between acute and chronic illness. An acute illness is sudden and severe. A chronic illness is gradual and ongoing. Consider the leading cause of death in the United States, coronary heart disease.
A heart attack is acute. A person feels fine, and then suddenly breath becomes shallow; or an arm, jaw, or shoulder hurts; or the person feels nauseous or heaviness around the heart (like an elephant standing on your chest). All these symptoms are signs of a heart attack—
By contrast, heart disease is chronic. The arteries are clogged, so blood pressure is high, or the heartbeat becomes unsteady. Exercise leads to exhaustion or shortness of breath. The heart gradually weakens. Many adults are unaware of any disability but have high blood pressure or high LDL cholesterol—
Heart problems are the most common cause of death for both men and women. However, in general, women are more likely to have chronic diseases and men to have acute ones. More men die of heart attacks, more women die of heart disease.
The same gender difference is apparent for many other conditions: Women have far more arthritis, lupus, type 2 diabetes, depression, and osteoporosis, for instance. Men are not exempt from these conditions and women also die of acute illnesses, but gender rates differ worldwide.
Women live for years with chronic illness; men are more likely to die quickly when they become seriously ill. That is one reason the sex ratio in U.S. nursing homes is about 3 women for every man, even though the overall population of those over age 65 is only about 1.3 women for every man (Figure 23.6).
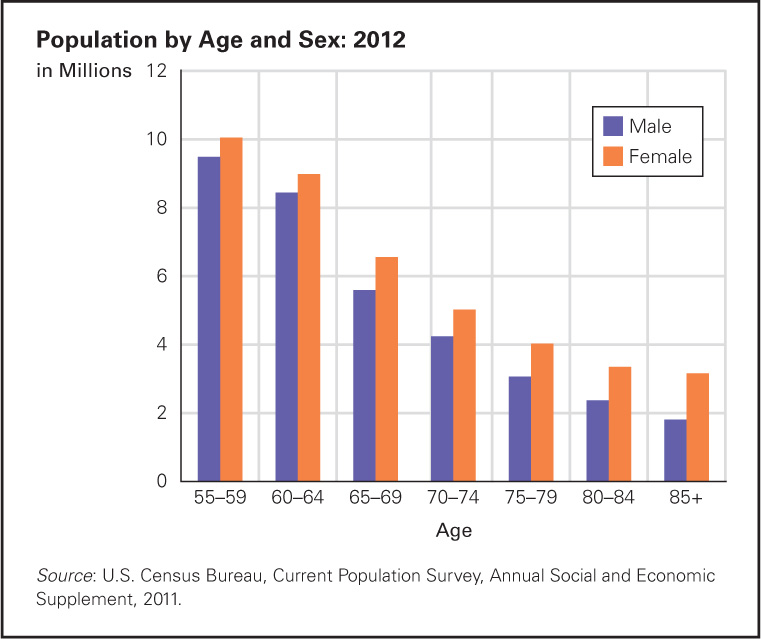
FIGURE 23.6
Lonely Old Men When younger people notice the sex ratio in late adulthood, they often pity the old women, many of whom are widows living alone and unable to find (or not interested in finding) a mate. That is not true of older men: Most are married, and if their wives die they remarry far more often than women do. But the data suggests that older women are closer to their friends, their relatives, and especially to their children than older men are. Indeed, their social network may be the reason they are far less likely to commit suicide or die of a heart attack than men their age.This distinction is problematic because hospitals, many doctors, and research funding target acute illnesses—
Quite apart from sexism, there are historical reasons for the neglect of chronic conditions. For most of human history, when people died at much younger ages, most died of acute illness. Saving heart attack victims, preventing blood poisoning, vaccinating against typhoid—
Compression of Morbidity
Ideally, prevention of disease begins in childhood and continues lifelong, so “the target of public health and aging efforts is not just the older adults of today but the children and adults who are the future elders” (Albert & Freedman, 2010, pp. 31–
compression of morbidity A shortening of the time a person spends ill or infirm, accomplished by postponing illness.
The name for this extension of vitality into old age is compression of morbidity, which is the reduction (compression) of sickness before death. Ideally, a person is in good health for decades after age 65, and then, within a few days or months, experiences serious illnesses that lead to death. Years of frailty are avoided.
Morbidity has been compressed even as mortality is postponed. For instance, unlike 30 years ago, most people diagnosed today with cancer, diabetes, or a heart condition continue to be vital for decades. The World Health Organization and many experts recognize that disability is the result of person–
osteoporosis A disease whose symptoms are low bone mass and deterioration of bone tissue, which lead to increasingly fragile bones and greater risk of fracture.
The need for compression of morbidity is apparent with osteoporosis (fragile bones). Primary aging makes bones more porous as cells that build bone (osteo-
The result of this chronic condition can be deadly, not just disabling. A fall that would have merely bruised a young person may result in a broken hip or a spine fracture, neither of which is lethal in itself but may potentially start a cascade of medical problems. Such a fall leads to death for 10 percent of osteoporosis sufferers within a year. According to The Center for Disease Control, a broken hip was “a leading cause of excess mortality among older adults” (MMWR, March 31, 2000). The problem was that half the people who broke their hips never walked again, and immobility causes many body systems to deteriorate.
Now let’s return to compression of morbidity. Note the 2000 date above. Now a more recent report: “In the 21st century, osteoporosis, a disease once considered an inevitable consequence of aging, is both diagnosable and treatable” (Black et al., 2012, p. 2051).
How was this compression of morbidity achieved? Early diagnosis via a bone density test (not available a few decades ago) can detect bone weakening long before the first fracture. Prevention can begin in middle age, or even earlier, with weight-
Because a focus on chronic conditions is relatively new and treatment of osteoporosis is newer yet, scientists do not know the consequences of ingesting preventive drugs over many years. The data suggest caution (Brown et al., 2012). As you know, drugs that prevent one problem may eventually cause another. [Lifespan Link: HRT (hormone replacement therapy) is discussed in Chapter 20.] Nonetheless, the 44 million people over age 50 in the United States who have weak bones need not experience the disabling breaks that those with osteoporosis once did. That is compression of morbidity.
Hearts and bones are only two examples. For almost every condition, morbidity can be compressed, although many people do not realize it. For instance, half the elderly population has arthritis, but few know that their stiffness and immobility can be reduced (Hootman et al., 2012). The same is true for diabetes, which often goes undiagnosed until it leads to other chronic problems of the heart, kidney, feet, eyes, and more (Caspersen et al., 2012).
Consider also breast cancer. That kills African American women at one and a half times the rate of European Americans, primarily because it is diagnosed too late, causing months of morbidity and then death rather than shorter morbidity and then recovery.
Gerontologists now agree that the goal is not simply to live a long life, but to live a long, healthy life; not to add years to life but to add life to years, via health habits, early treatment, and so on (Gremeaux et al., 2012). Demographers now calculate the number of healthy years. This has been done for each state of the United States (MMWR, July 19, 2013) (see Figure 23.7).
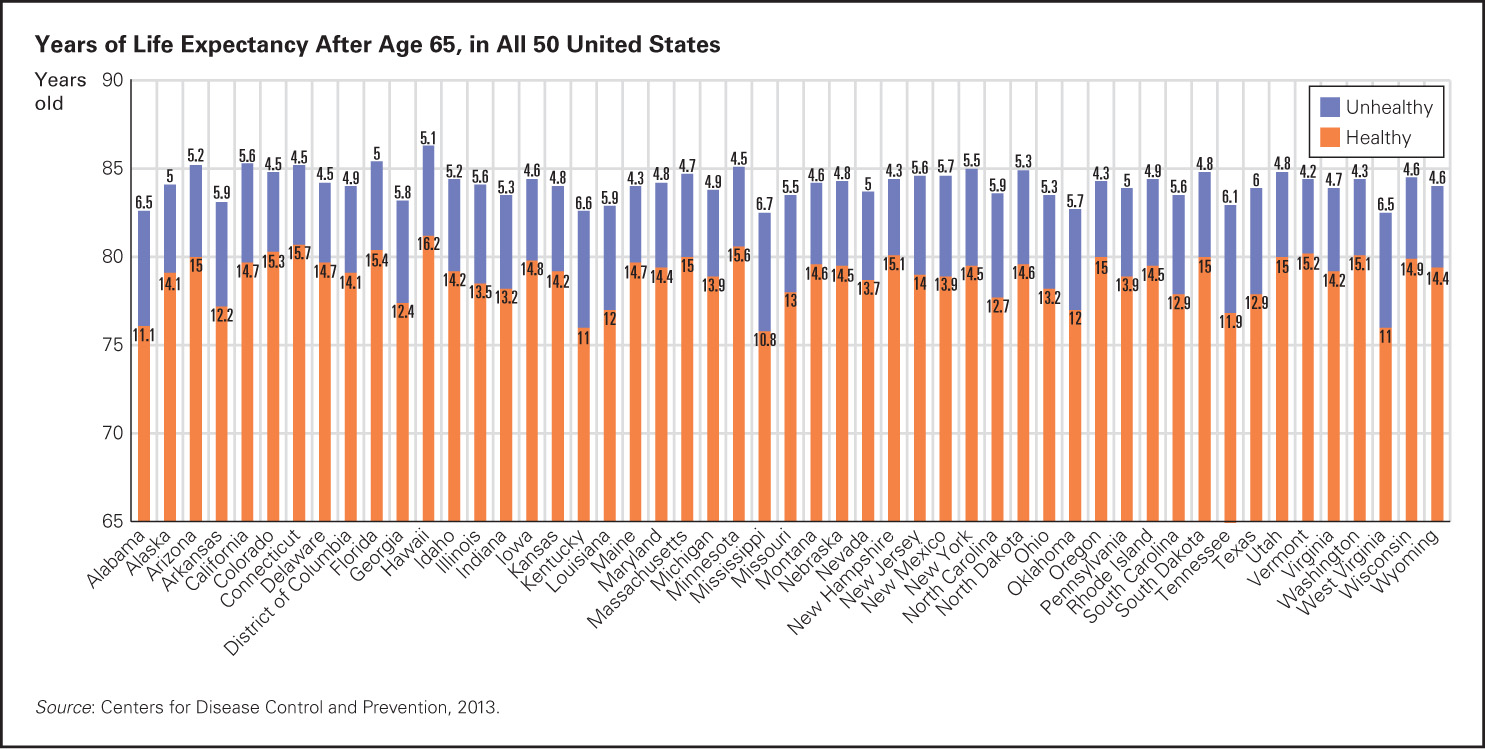
FIGURE 23.7
Life Expectancy after Age 65 Another Reason to Live in Hawaii After age 65, people in Hawaii have 18 more healthy years compared to only 11 in Mississippi, or maybe go to Oregon, with only 4 unhealthy years before death, on average, at age 84.The U.S. data as well as the data from other nations show that there is no set age when people become frail. The correlation between sheer longevity and healthy longevity is positive; further compression of morbidity seems a realistic goal.
SUMMING UP
Primary aging is inevitable and universal, the direct result of years gone by. Secondary aging involves diseases that result from poor health habits, genetic vulnerability, infections, and environmental toxins that often exacerbate the losses associated with primary aging. Some of the most troubling morbidities relate to the senses, particularly vision and hearing, because sensory impairment leads to depression and social isolation. Acute illnesses are sudden, and medical measures have reduced them markedly. The next goal is to reduce debilitation caused by chronic diseases, a goal called compression of morbidity. As illustrated with osteoporosis, aging need not be accompanied by years of debilitating disease.