12.4 What Causes Substance Use Disorders?
Clinical theorists have developed sociocultural, psychological, and biological explanations for why people develop substance use disorders. No single explanation, however, has gained broad support. Like so many other disorders, excessive and chronic drug use is increasingly viewed as the result of a combination of these factors.
Sociocultural Views

What factors might explain the finding that different ethnic, religious, and national groups have different rates of alcohol use disorder?
A number of sociocultural theorists propose that people are most likely to develop substance use disorders when they live under stressful socioeconomic conditions (Gardner et al., 2010). Studies have found that regions with higher unemployment levels have higher alcoholism rates. Similarly, people in lower socioeconomic classes have rates of substance use disorder that are higher than those of the other classes (Marsiglia & Smith, 2010; Franklin & Markarian, 2005). In a related vein, 18 percent of unemployed adults currently use an illegal drug, compared with 9 percent of full-
Sociocultural theorists hold that people confronted regularly by other kinds of stress also have a heightened risk of developing substance use disorders. A range of studies conducted with Hispanic and African American people, for example, find higher rates of substance use disorders among those participants who live or work in environments of particularly intense discrimination (Clark, 2014; Hurd et al., 2014; Unger et al., 2014).
Still other sociocultural theorists propose that people are more likely to develop substance use disorders if they are part of a family or social environment in which substance use is valued or at least accepted (Chung et al., 2014; Washburn et al., 2014). Researchers have learned that problem drinking is more common among teenagers whose parents and peers drink, as well as among teenagers whose family environments are stressful and unsupportive (Wilens et al., 2014; Andrews & Hops, 2011; Kliewer, 2010). Moreover, lower rates of alcoholism are found among Jews and Protestants, groups in which drinking is typically acceptable only as long as it remains within clear limits, whereas alcoholism rates are higher among the Irish and Eastern Europeans, who do not, in general, draw as clear a line (Hart & Ksir, 2014; Ledoux et al., 2002).
Psychodynamic Views
Psychodynamic theorists believe that people with substance use disorders have powerful dependency needs that can be traced to their early years (Iglesias et al., 2014; Dodes & Khantzian, 2011, 2005). They suggest that when parents fail to satisfy a young child’s need for nurturance, the child is likely to grow up depending excessively on others for help and comfort, trying to find the nurturance that was lacking during the early years. If this search for outside support includes experimentation with a drug, the person may well develop a dependent relationship with the substance.
Some psychodynamic theorists also believe that certain people respond to their early deprivations by developing a substance abuse personality that leaves them particularly prone to drug abuse. Personality inventories, patient interviews, and even animal studies have in fact indicated that individuals who abuse drugs tend to be more dependent, antisocial, impulsive, novelty-
BETWEEN THE LINES
Nonmedical Use of Pain Relievers
In the United States, the largest increase in illicit drug use during the past few years has been the nonmedical use of medications, mostly pain relievers (NSDUH, 2013).
In an effort to establish clearer causation, one pioneering longitudinal study measured the personality traits of a large group of nonalcoholic young men and then kept track of each man’s development (Jones, 1971, 1968). Years later, the traits of the men who developed alcohol problems in middle age were compared with the traits of those who did not. The men who developed alcohol problems had been more impulsive as teenagers and continued to be so in middle age, a finding suggesting that impulsive men are indeed more prone to develop alcohol problems. Similarly, in various laboratory investigations, “impulsive” rats—
A major weakness of this line of argument is the wide range of personality traits that have been tied to substance use disorders. Different studies point to different “key” traits (Wills & Ainette, 2010). Inasmuch as some people with these disorders appear to be dependent, others impulsive, and still others antisocial, researchers cannot presently conclude that any one personality trait or group of traits stands out in the development of the disorders (Chassin et al., 2001).
Cognitive-Behavioral Views
According to behaviorists, operant conditioning may play a key role in substance use disorders. They argue that the temporary reduction of tension or raising of spirits produced by a drug has a rewarding effect, thus increasing the likelihood that the user will seek this reaction again (Clark, 2014; Urošević et al., 2014). Similarly, the rewarding effects may eventually lead users to try higher dosages or more powerful methods of ingestion (see Table 12-4). Cognitive theorists further argue that such rewards eventually produce an expectancy that substances will be rewarding, and this expectation helps motivate people to increase drug use at times of tension (Sussman, 2010).
|
Method |
Route |
Time to reach Brain |
|
Inhaling |
Drug in vapor form is inhaled through mouth and lungs into circulatory system. |
7 seconds |
|
Snorting |
Drug in powdered form is snorted into the nose. Some of the drug lands on the nasal mucous membranes, is absorbed by blood vessels, and enters the bloodstream. |
4 minutes |
|
Injection |
Drug in liquid form directly enters the body through a needle. Injection may be intravenous or intramuscular (subcutaneous). Intravenous Intramuscular |
20 seconds 4 minutes |
|
Oral ingestion |
Drug in solid or liquid form passes through esophagus and stomach and finally to the small intestines. It is absorbed by blood vessels in the intestines. |
30 minutes |
|
Other routes |
Drugs can be absorbed through areas that contain mucous membranes. Drugs can be placed under the tongue, inserted anally and vaginally, and administered as eyedrops. |
Variable |
|
Information from: Hart & Ksir, 2014; Landry, 1994. |
||
In support of these behavioral and cognitive views, studies have found that many people do drink more alcohol or seek heroin when they feel tense (Kassel et al., 2010; McCarthy et al., 2010). In one study, as participants worked on a difficult anagram task, a confederate planted by the researchers unfairly criticized and belittled them (Marlatt, Kosturn, & Lang, 1975). The participants were then asked to participate in an “alcohol taste task,” supposedly to compare and rate alcoholic beverages. Those who had been harassed drank more alcohol during the taste task than did the control participants who had not been criticized.

In a manner of speaking, the cognitive-
A number of behaviorists have proposed that classical conditioning may also play a role in these disorders (O’Brien, 2013; Cunningham et al., 2011). As you’ll remember from Chapters 3 and 5, classical conditioning occurs when two stimuli that appear close together in time become connected in a person’s mind, so that eventually, the person responds similarly to each stimulus. Cues or objects present in the environment at the time a person takes a drug may act as classically conditioned stimuli and come to produce some of the same pleasure brought on by the drugs themselves. Just the sight of a hypodermic needle, drug buddy, or regular supplier, for example, has been known to comfort people who are addicted to heroin or amphetamines and to relieve their withdrawal symptoms. In a similar manner, cues or objects that are present during withdrawal distress may produce withdrawal-
Biological Views
In recent years, researchers have come to suspect that drug misuse may have biological causes. Studies on genetic predisposition and specific biochemical processes have provided some support for these suspicions.
Genetic PredispositionFor years, breeding experiments have been conducted to see whether certain animals are genetically predisposed to become addicted to drugs (Carroll & Meisch, 2011; Weiss, 2011). In several studies, for example, investigators have first identified animals that prefer alcohol to other beverages and then mated them to one another. Generally, the offspring of these animals have been found also to display an unusual preference for alcohol.
Similarly, some research with human twins has suggested that people may inherit a predisposition to misuse substances (Ystrom et al., 2014). One classic study found an alcoholism concordance rate of 54 percent in a group of identical twins; that is, if one identical twin displayed alcoholism, the other twin also did in 54 percent of the cases. In contrast, a group of fraternal twins had a concordance rate of only 28 percent (Kaij, 1960). Other studies have found similar twin patterns (Koskinen et al., 2011; Legrand et al., 2005; Tsuang et al., 2001). As you have read, however, such findings do not rule out other interpretations. For one thing, the parenting received by two identical twins may be more similar than that received by two fraternal twins.
A clearer indication that genetics may play a role in substance use disorders comes from studies of alcoholism rates in people adopted shortly after birth (Samek et al., 2014; Walters, 2002; Cadoret et al., 1995; Goldstein, 1994). These studies have compared adoptees whose biological parents abuse alcohol with adoptees whose biological parents do not. By adulthood, the individuals whose biological parents abuse alcohol typically show higher rates of alcoholism than those with nonalcoholic biological parents.

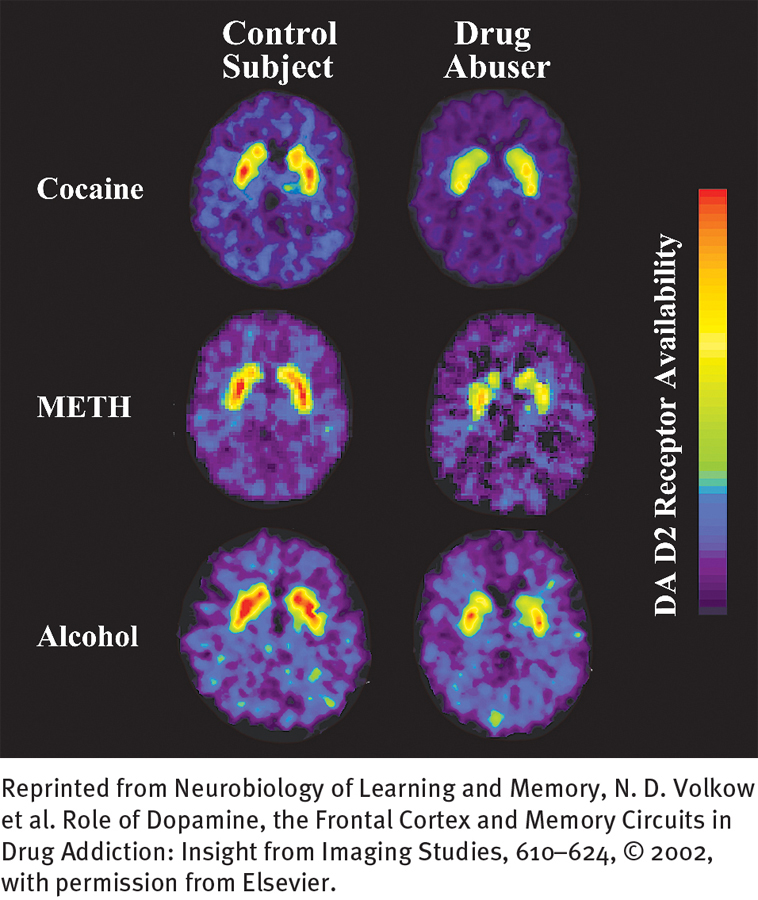
Genetic linkage strategies and molecular biology techniques provide more direct evidence in support of a genetic explanation (Pieters et al., 2012; Gelernter & Kranzler, 2008). One line of investigation has found an abnormal form of the so-
Biochemical FactorsOver the past few decades, researchers have pieced together several biological explanations of drug tolerance and withdrawal symptoms (Chung et al., 2012; Kosten, George, & Kleber, 2011, 2005; Schmidt et al., 2011). According to one of the leading explanations, when a particular drug is ingested, it increases the activity of certain neurotransmitters whose normal purpose is to calm, reduce pain, lift mood, or increase alertness. When a person keeps on taking the drug, the brain apparently makes an adjustment and reduces its own production of the neurotransmitters. Because the drug is increasing neurotransmitter activity or efficiency, the brain’s release of the neurotransmitter is less necessary. As drug intake increases, the body’s production of the neurotransmitters continues to decrease, leaving the person in need of progressively more of the drug to achieve its effects. In this way, drug takers build tolerance for a drug, becoming more and more reliant on it rather than on their own biological processes to feel comfortable, happy, or alert. If they suddenly stop taking the drug, their natural supply of neurotransmitters will be low for a time, producing the symptoms of withdrawal. Withdrawal continues until the brain resumes its normal production of the neurotransmitters.

Which neurotransmitters are affected depends on the drug used. Repeated and excessive use of alcohol or benzodiazepines may lower the brain’s production of the neurotransmitter GABA, regular use of opioids may reduce the brain’s production of endorphins, and regular use of cocaine or amphetamines may lower the brain’s production of dopamine (Kosten et al., 2011, 2005). In addition, researchers have identified a neurotransmitter called anandamide that operates much like THC; excessive use of marijuana may reduce the production of anandamide (Budney et al., 2011; Hitti, 2004).
This theory helps explain why people who regularly take substances have tolerance and withdrawal reactions. But why are drugs so rewarding, and why do certain people turn to them in the first place? A number of brain-
 reward center A dopamine-
reward center A dopamine-
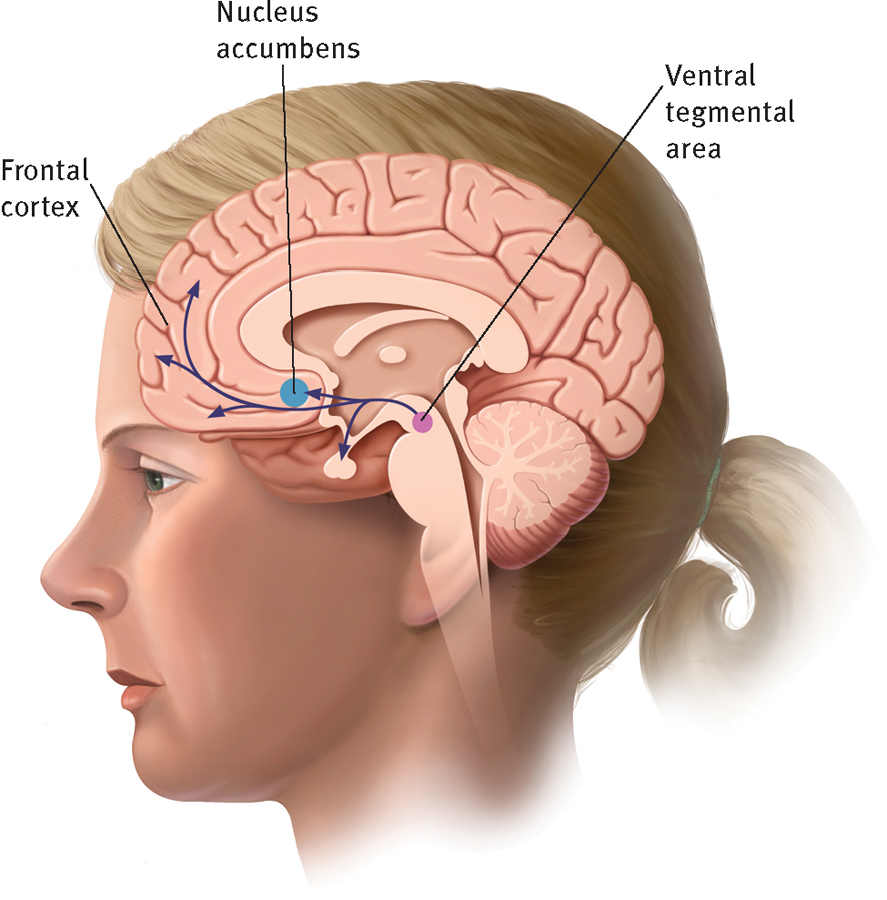
Pleasure centers in the brain
One of the reasons drugs produce feelings of pleasure is because they increase levels of the neurotransmitter dopamine along a “pleasure pathway” in the brain that extends from the ventral tegmental area to the nucleus accumbens and then to the frontal cortex. This activation of pleasure centers plays a role in addiction.
Certain drugs apparently stimulate the reward center directly. Remember that cocaine, amphetamines, and caffeine directly increase dopamine activity. Other drugs seem to stimulate it in roundabout ways. The biochemical reactions triggered by alcohol, opioids, and marijuana probably set in motion a series of chemical events that eventually lead to increased dopamine activity in the reward center.
A number of theorists further believe that when substances repeatedly stimulate this reward center, the center develops a hypersensitivity to the substances. Neurons in the center fire more readily when stimulated by the substances, contributing to future desires for them. This theory, called the incentive-
Still other theorists suspect that people who chronically use drugs may suffer from a reward-