15.5 The Community Approach

The broadest approach for the treatment of schizophrenia and other severe mental disorders is the community approach. In 1963, partly in response to the terrible conditions in public mental institutions and partly because of the emergence of antipsychotic drugs, the U.S. government ordered that patients be released and treated in the community. Congress passed the Community Mental Health Act, which stipulated that patients with psychological disorders were to receive a range of mental health services—
Thus began several decades of deinstitutionalization, an exodus of hundreds of thousands of patients with schizophrenia and other long-
How might the “revolving door” pattern itself worsen the symptoms and outlook of people with schizophrenia?
 deinstitutionalization The discharge of large numbers of patients from long-
deinstitutionalization The discharge of large numbers of patients from long-
What Are the Features of Effective Community Care?
People recovering from schizophrenia and other severe disorders need medication, psychotherapy, help in handling daily pressures and responsibilities, guidance in making decisions, social skills training, residential supervision, and vocational counseling—
Coordinated ServicesWhen the Community Mental Health Act was first passed, it was expected that community care would be provided by community mental health centers, treatment facilities that would supply medication, psychotherapy, and inpatient emergency care to people with severe disturbances, as well as coordinate the services offered by other community agencies. When community mental health centers are available and do provide these services, patients with schizophrenia and other severe disorders often make significant progress (Burns & Drake, 2011; Rapp & Goscha, 2008). Coordination of services is particularly important for so-
 community mental health center A treatment facility that provides medication, psychotherapy, and emergency care for psychological problems and coordinates treatment in the community.
community mental health center A treatment facility that provides medication, psychotherapy, and emergency care for psychological problems and coordinates treatment in the community.

Short-
 aftercare A program of posthospitalization care and treatment in the community.
aftercare A program of posthospitalization care and treatment in the community.
Partial HospitalizationPeople’s needs may fall between full hospitalization and outpatient therapy, and so some communities offer day centers, or day hospitals, all-
 day center A program that offers hospital-
day center A program that offers hospital-
Another kind of institution that has become a popular setting for the treatment of people with schizophrenia and other severe disorders is the semihospital, or residential crisis center. Semihospitals are houses or other structures in the community that provide 24-

Supervised ResidencesMany people do not require hospitalization but are unable to live alone or with their families. Halfway houses, also known as crisis houses or group homes, often serve individuals well (Lindenmayer & Khan, 2012; Levy et al., 2005). Such residences may shelter between one and two dozen people. The live-
 halfway house A residence for people with schizophrenia or other severe problems, often staffed by paraprofessionals. Also known as a group home or crisis house.
halfway house A residence for people with schizophrenia or other severe problems, often staffed by paraprofessionals. Also known as a group home or crisis house.
The halfway house changed my life. First of all, I discovered that some of the staff members had once been clients in the program! That one single fact offered me hope. For the first time, I saw proof that a program could help someone, that it was possible to regain control over one’s life and become independent. The house was democratically run; all residents had one vote and the staff members, outnumbered 5 to 22, could not make rules or even discharge a client from the program without majority sentiment. There was a house bill of rights that was strictly observed by all. We helped one another and gave support. When residents were in a crisis, no staff member hustled them off or increased their medication to calm them down. Residents could cry, be comforted and hugged until a solution could be found, or until they accepted that it was okay to feel bad. Even anger was an acceptable feeling that did not have to be feared, but could be expressed and turned into constructive energy. If you disliked some aspect of the program or the behavior of a staff member, you could change things rather than passively accept what was happening. Choices were real, and failure and success were accepted equally…. Bit by bit, my distrust faltered and the fears lessened. I slept better and made friends…. Other residents and staff members who had hallucinated for years and now were able to control their hallucinations shared with me some of the techniques that had worked for them. Things like diet … and interpersonal relationships became a few of my tools.
(Lovejoy, 1982, pp. 605–
Occupational Training and SupportPaid employment provides income, independence, self-
Many people recovering from such disorders receive occupational training in a sheltered workshop—a supervised workplace for employees who are not ready for competitive or complicated jobs. The workshop replicates a typical work environment: products such as toys or simple appliances are manufactured and sold, workers are paid according to performance and are expected to be at work regularly and on time. For some, the sheltered workshop becomes a permanent workplace. For others, it is an important step toward better-
 sheltered workshop A supervised workplace for people who are not yet ready for competitive jobs.
sheltered workshop A supervised workplace for people who are not yet ready for competitive jobs.
An alternative work opportunity for people with severe psychological disorders is supported employment, in which vocational agencies and counselors help clients find competitive jobs in the community and provide psychological support while the clients are employed (Solar, 2014: Bell et al., 2011). Like sheltered workshops, supported employment opportunities are often in short supply.
How Has Community Treatment Failed?
There is no doubt that effective community programs can help people with schizophrenia and other severe mental disorders recover. However, fewer than half of all the people who need them receive appropriate community mental health services (Burns & Drake, 2011; Lehman et al., 2004; McGuire, 2000). In fact, in any given year, 40 to 60 percent of all people with schizophrenia and other severe mental disorders receive no treatment at all (Wang et al., 2002; Torrey, 2001). Two factors are primarily responsible: poor coordination of services and a shortage of services.
Poor Coordination of ServicesThe various mental health agencies in a community often fail to communicate with one another. There may be an opening at a nearby halfway house, for example, and the therapist at the community mental health center may not know about it. In addition, even within a community agency a patient may not have continuing contacts with the same staff members and may fail to receive consistent services. Still another problem is poor communication between state hospitals and community mental health centers, particularly at times of discharge (Torrey, 2001).
To help deal with such problems in communication and coordination, a growing number of community therapists have become case managers for people with schizophrenia and other severe mental disorders (Mas-
 case manager A community therapist who offers a full range of services for people with schizophrenia or other severe disorders, including therapy, advice, medication, guidance, and protection of patients’ rights.
case manager A community therapist who offers a full range of services for people with schizophrenia or other severe disorders, including therapy, advice, medication, guidance, and protection of patients’ rights.
Shortage of ServicesThe number of community programs—
There are various reasons for this shortage of services. Perhaps the primary one is economic (Feldman et al., 2014; Covell et al., 2011). On the one hand, more public funds are available for people with psychological disorders now than in the past. In 1963 a total of $1 billion was spent in this area, whereas today approximately $171 billion in public funding is devoted each year to people with mental disorders (Rampell, 2013; Gill, 2010; Redick et al., 1992). This represents a significant increase even when inflation and so-

What Are the Consequences of Inadequate Community Treatment?What happens to people with schizophrenia and other severe disorders whose communities do not provide the services they need and whose families cannot afford private treatment (see Figure 15-2)? As you have read, a large number receive no treatment at all; many others spend a short time in a state hospital or semihospital and are then discharged prematurely, often without adequate follow-
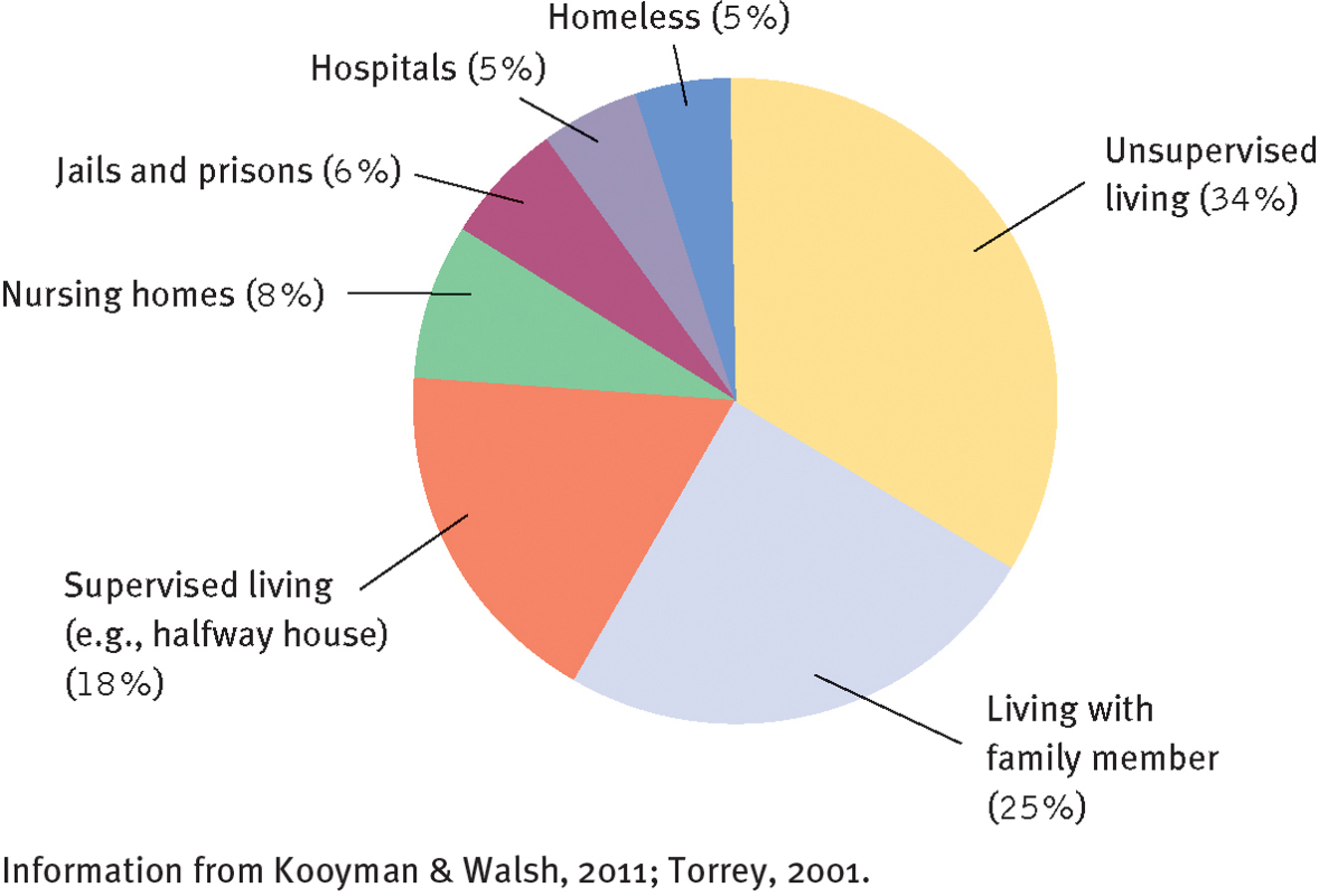
Where do people with schizophrenia live?
More than one-
Many of the people with schizophrenia and other severe disorders return to their families and receive medication and perhaps emotional and financial support, but little else in the way of treatment (Barrowclough & Lobban, 2008). Around 8 percent enter an alternative institution such as a nursing home or rest home, where they receive only custodial care and medication (Torrey, 2001). As many as 18 percent are placed in privately run residences where supervision often is provided by untrained staff—
Another 34 percent of people with schizophrenia and other severe disorders live in totally unsupervised settings. Some are equal to the challenge of living alone, supporting themselves effectively, and maintaining nicely furnished apartments. But many cannot really function independently and wind up in rundown single-

Why do so many people continue to perceive people with schizophrenia as dangerous and violent, despite evidence to the contrary?
Finally, a great number of people with schizophrenia and other severe disorders have become homeless (Ogden, 2014; Kooyman & Walsh, 2011). There are between 400,000 and 800,000 homeless people in the United States, and approximately one-
The Promise of Community Treatment
BETWEEN THE LINES
Mistaken Impression
Most of the “violent” acts committed by people with schizophrenia are relatively minor, such as shoving or slapping.
(Swanson, 2010)
Despite these very serious problems, proper community care has shown great potential for assisting people in recovering from schizophrenia and other severe disorders, and clinicians and many government officials continue to press to make it more available. In addition, a number of national interest groups have formed in countries around the world that push for better community treatment (Frese, 2008). In the United States, for example, the National Alliance on Mental Illness (NAMI) began in 1979 with 300 members and has expanded to 200,000 members in more than 1,000 chapters (NAMI, 2014). Made up largely of families and people affected by severe mental disorders (particularly schizophrenia, bipolar disorders, and major depressive disorder), NAMI has become not only a source of information, support, and guidance for its members but also a powerful lobbying force in state and national legislatures; and it has pressured community mental health centers to treat more people with schizophrenia and other severe disorders.
MediaSpeak
“Alternative” Mental Health Care
By Merrill Balassone, Washington Post, December 6, 2010
An 18-
A woman lets out a long guttural scream to nobody in particular to turn off the lights.
A 24-
This is not the inside of a psychiatric hospital. It’s the B-
Stanislaus County is not unique. Experts say U.S. prisons and jails have become the country’s largest mental health institutions, its new asylums. Nearly four times more Californians with serious mental illnesses are housed in jails and prisons than in hospitals…. Nationally, 16 to 20 percent of prisoners are mentally ill, said Harry K. Wexler, a psychologist specializing in crime and substance abuse.
“I think it’s a national tragedy,” Wexler said. “Prisons are the institutions of last resort. The mentally ill are generally socially undesirable, less employable, more likely to be homeless and get on that slippery slope of repeated involvement in the criminal justice system.”
Those who staff prisons and jails are understandably ill-
Why is it shortsighted—
Mentally ill offenders have higher recidivism rates than other inmates (they’re called “frequent fliers” in the criminal justice world) because they receive little psychiatric care after their release, researchers say. They cost more to jail because of the cost of medications and psychiatric examinations, and they can cause security problems by their aggressive and destructive behavior in lockup.
Wexler said these inmates also are more likely to commit suicide. Because they’re less capable of conforming to the rigid rules of a jailhouse, they can end up in isolation as punishment, Wexler said.

At 4:30 a.m. in the … jail—
Because of the lack of hospital space, police are often forced to take the mentally ill who commit minor misdemeanors—
One nationally recognized solution is called a mental health treatment court, which gives offenders the choice between going to jail or following a treatment plan—
But at the same time, [because of budget cuts, mental health treatment courts have been] forced to stop taking new offenders…. “We deal every day with this crisis of the mentally ill—
December 6, 2010, “Jails, Prisons Increasingly Taking Care of Mentally Ill” by Merrill Balassone. From The Modesto Bee, 12/6/2010, © 2010 McClatchy. All rights reserved. Used by permission and protected by the copyright laws of the United States. The printing, copying, redistribution, or retransmission of this content without express written permission is prohibited.
Today, community care is a major feature of treatment for people recovering from severe mental disorders in countries around the world. Both in the United States and abroad, well-