4.3 Treatment: How Might the Client Be Helped?
BETWEEN THE LINES
Contradictory Trends
Since 1998, the number of patients receiving psychotherapy alone has fallen by 34 percent. The number receiving medication alone has increased by 23 percent.
However, today’s patients express a three-
times- greater preference for psychotherapy over medications (Gaudiano, 2013).
Over the course of 10 months, Franco was treated for depression and related symptoms. He improved considerably during that time, as the following report describes:
During therapy, Franco’s debilitating depression relented. Increasingly, he came to appreciate that his mother’s accusations against him—
Franco also managed to straighten out his problems at work. He explained his recent difficulties to his immediate supervisor at the bank and committed himself to improving his recent performance. His supervisor, with whom he had been friendly before his recent struggles, said she was glad that he was communicating openly, and emphasized that he would be given the opportunity to improve his performance. He was surprised to hear how highly he had been regarded over the years, although as she put it, “Why would you have been promoted otherwise?”
Over the course of therapy, Franco also forced himself to spend more time having fun with his friends. He found his mood on the upswing as a result of these re-
Clearly, treatment helped Franco, and by its conclusion he was a happier, more functional person than the man who had first sought help 10 months earlier. But how did his therapist decide on the treatment program that proved to be so helpful?
Treatment Decisions
Franco’s therapist began, like all therapists, with assessment information and diagnostic decisions. Knowing the specific details and background of Franco’s problem (idiographic data) and combining this individual information with broad information about the nature and treatment of depression (nomothetic data), the clinician arrived at a treatment plan for him.
Yet therapists may be influenced by additional factors when they make treatment decisions. Their treatment plans typically reflect their theoretical orientations and how they have learned to conduct therapy (Prochaska & Norcross, 2013; Sharf, 2012). As therapists apply a favored model in case after case, they become more and more familiar with its principles and treatment techniques and tend to use them in work with still other clients.
Current research may also play a role. Most clinicians say that they value research as a guide to practice (Beutler et al., 1995). However, not all of them actually read research articles, so they cannot be directly influenced by them (Rivett, 2011; Stewart & Chambless, 2007). In fact, according to surveys, therapists gather much of their information about the latest developments in the field from colleagues, professional newsletters, workshops, conferences, Web sites, books, and the like (Simon, 2011; Corrie & Callanan, 2001). Unfortunately, the accuracy and usefulness of these sources vary widely.
To help clinicians become more familiar with and apply research findings, there is an ever-
 empirically supported treatment Therapy that has received clear research support for a particular disorder and has corresponding treatment guidelines. Also known as evidence-
empirically supported treatment Therapy that has received clear research support for a particular disorder and has corresponding treatment guidelines. Also known as evidence-
The Effectiveness of Treatment
Altogether, more than 400 forms of therapy are currently practiced in the clinical field (Wedding & Corsini, 2014). Naturally, the most important question to ask about each of them is whether it does what it is supposed to do. Does a particular treatment really help people overcome their psychological problems? If so, the practitioner has performed a major service for the client. On the surface, the question may seem simple. In fact, it is one of the most difficult questions for clinical researchers to answer.
The first problem is how to define “success.” If, as Franco’s therapist implies, he still has much progress to make at the conclusion of therapy, should his recovery be considered successful? The second problem is how to measure improvement (Hunsley & Lee, 2014; Lambert, 2010; Luborsky, 2004). Should researchers give equal weight to the reports of clients, friends, relatives, therapists, and teachers? Should they use rating scales, inventories, therapy insights, observations, or some other measure?
BETWEEN THE LINES
The Stigma Continues
|
33% |
Americans who would not seek counseling for fear of being labeled “mentally ill” |
|
51% |
Americans who would hesitate to see a psychotherapist if a diagnosis were required |
|
67% |
Americans who would not tell their employer that they were seeking mental health treatment |
|
37% |
Americans who would be reluctant to seek treatment because of confidentiality concerns |
|
41% |
Americans who believe they should be able to handle psychological problems on their own |
|
(Opinion Research Corporation, 2011, 2004) |
|
Perhaps the biggest problem in determining the effectiveness of treatment is the variety and complexity of the treatments currently in use. People differ in their problems, personal styles, and motivations for therapy. Therapists differ in skill, experience, orientation, and personality. And therapies differ in theory, format, and setting. Because an individual’s progress is influenced by all these factors and more, the findings of a particular study will not always apply to other clients and therapists.
Proper research procedures address some of these problems. By using control groups, random assignment, matched research participants, and the like, clinicians can draw certain conclusions about various therapies. Even in studies that are well designed, however, the variety and complexity of treatment limit the conclusions that can be reached (Kazdin, 2013, 2011, 2006, 2004).
Despite these difficulties, the job of evaluating therapies must be done, and clinical researchers have plowed ahead with it. Investigators have, in fact, conducted thousands of therapy outcome studies, studies that measure the effects of various treatments. The studies typically ask one of three questions: (1) Is therapy in general effective? (2) Are particular therapies generally effective? (3) Are particular therapies effective for particular problems?
Is Therapy Generally Effective?Studies suggest that therapy often is more helpful than no treatment or than placebos. A pioneering review examined 375 controlled studies, covering a total of almost 25,000 people seen in a wide assortment of therapies (Smith, Glass, & Miller, 1980; Smith & Glass, 1977). The reviewers combined the findings of these studies by using a special statistical technique called meta-
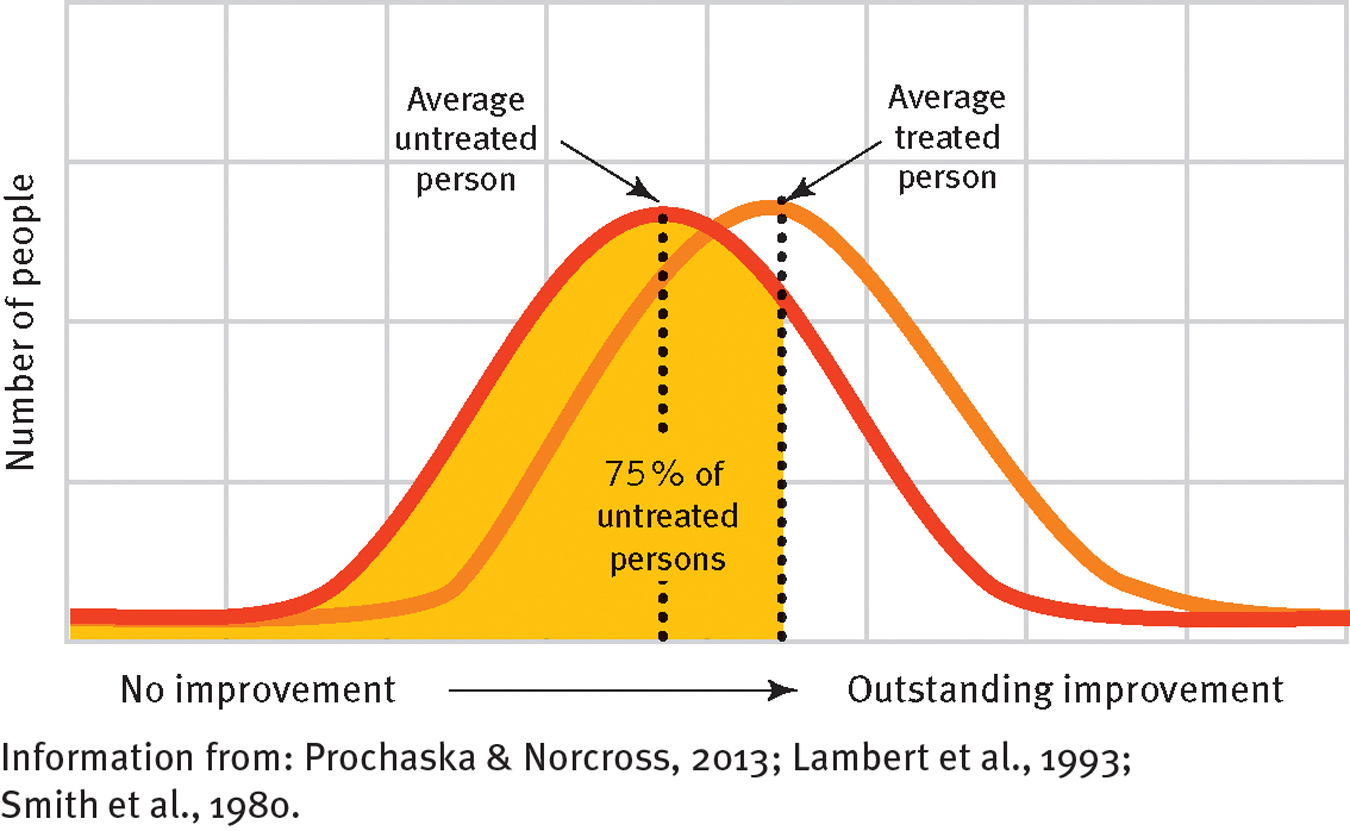
Does therapy help?
Combining participants and results from hundreds of studies, investigators have determined that the average person who receives psychotherapy improves more than do 75 percent of all untreated people with similar problems.
Some clinicians have concerned themselves with an important related question: Can therapy be harmful? A number of studies suggest that 5 to 10 percent of patients actually seem to get worse because of therapy (Lambert, 2010). Their symptoms may become more intense, or they may develop new ones, such as a sense of failure, guilt, reduced self-
Are Particular Therapies Generally Effective?The studies you have read about so far have lumped all therapies together to consider their general effectiveness. Many researchers, however, consider it wrong to treat all therapies alike. Some critics suggest that these studies are operating under a uniformity myth—a false belief that all therapies are equivalent despite differences in the therapists’ training, experience, theoretical orientations, and personalities (Good & Brooks, 2005; Kiesler, 1995, 1966).
Thus, an alternative approach examines the effectiveness of particular therapies. Most research of this kind shows each of the major forms of therapy to be superior to no treatment or to placebo treatment (Prochaska & Norcross, 2010). A number of other studies have compared particular therapies with one another and found that no one form of therapy generally stands out over all others (Luborsky et al., 2006, 2003, 2002, 1975).
How can people make wise decisions about therapists and treatment approaches when they are seeking treatment?
If different kinds of therapy have similar successes, might they have something in common? People in the rapprochement movement have tried to identify a set of common factors, or common strategies, that may run through all effective therapies, regardless of the clinicians’ particular orientations (Sharf, 2012) (see InfoCentral below). Surveys of highly successful therapists suggest, for example, that most give feedback to clients, help clients focus on their own thoughts and behavior, pay attention to the way they and their clients are interacting, and try to promote self-
 rapprochement movement A movement to identify a set of common factors, or common strategies, that run through all successful therapies.
rapprochement movement A movement to identify a set of common factors, or common strategies, that run through all successful therapies.
Are Particular Therapies Effective for Particular Problems?People with different disorders may respond differently to the various forms of therapy (Norcross & Beutler, 2014; Beutler, 2011). In an oft-
As you read previously, studies also show that some clinical problems may respond better to combined approaches (Norcross & Beutler, 2014; Valencia et al., 2013). Drug therapy is sometimes combined with certain forms of psychotherapy, for example, to treat depression. In fact, it is now common for clients to be seen by two therapists—
 psychopharmacologist A psychiatrist who primarily prescribes medications.
psychopharmacologist A psychiatrist who primarily prescribes medications.
InfoCentral
COMMON FACTORS IN THERAPY
The evidence-
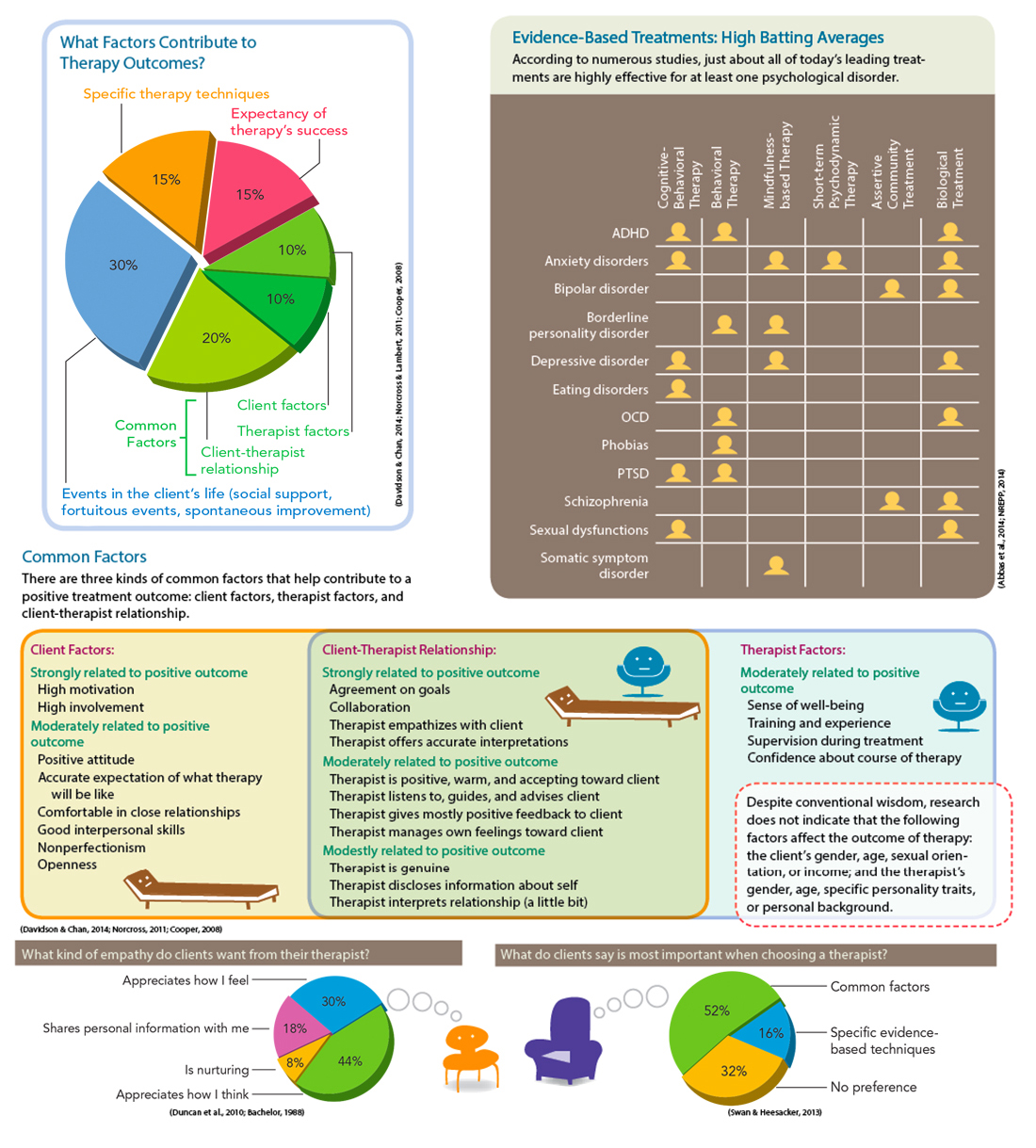
Obviously, knowledge of how particular therapies fare with particular disorders can help therapists and clients alike make better decisions about treatment (Beutler, 2011, 2002, 2000; Beutler et al., 2011) (see Figure 4-5). We will keep returning to this issue as we examine the various disorders throughout the book.
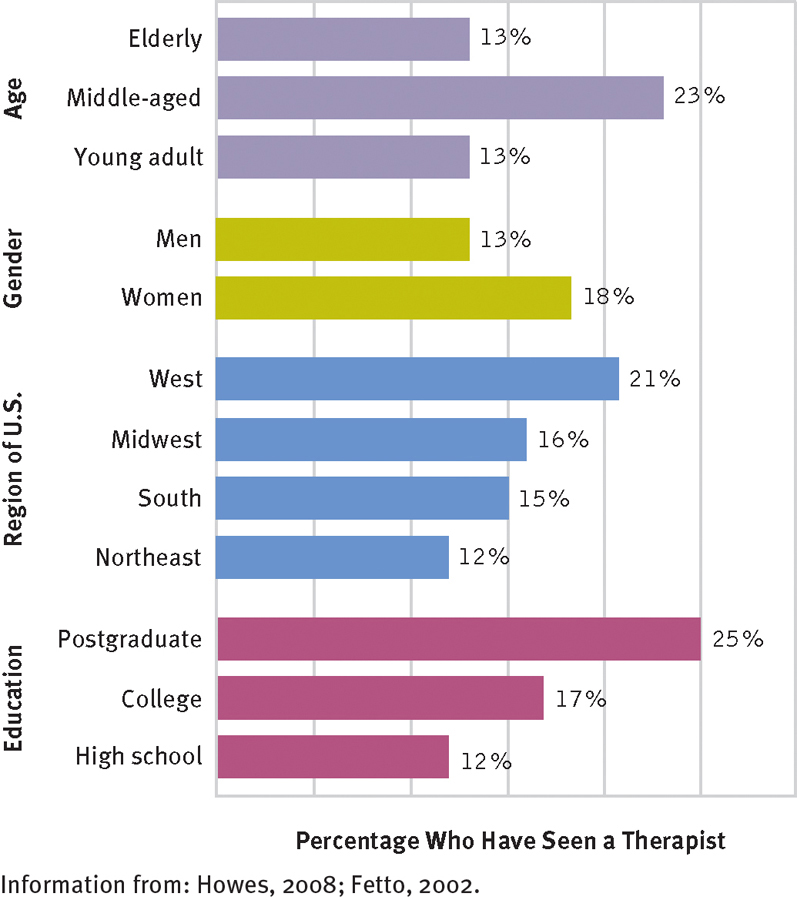
Who seeks therapy? According to surveys conducted in the United States, people who are middle-