1.3 How Was Abnormality Viewed and Treated in the Past?
In any given year, as many as 30 percent of the adults and 19 percent of the children and adolescents in the United States display serious psychological disturbances and are in need of clinical treatment (Merikangas et al., 2013; Kessler et al., 2012, 2009). The rates in other countries are similarly high. It is tempting to conclude that something about the modern world is responsible for these many emotional problems—
Ancient Views and Treatments
Historians who have examined the unearthed bones, artwork, and other remnants of ancient societies have concluded that these societies probably regarded abnormal behavior as the work of evil spirits. People in prehistoric societies apparently believed that all events around and within them resulted from the actions of magical, sometimes sinister, beings who controlled the world. In particular, they viewed the human body and mind as a battleground between external forces of good and evil. Abnormal behavior was typically interpreted as a victory by evil spirits, and the cure for such behavior was to force the demons from a victim’s body.
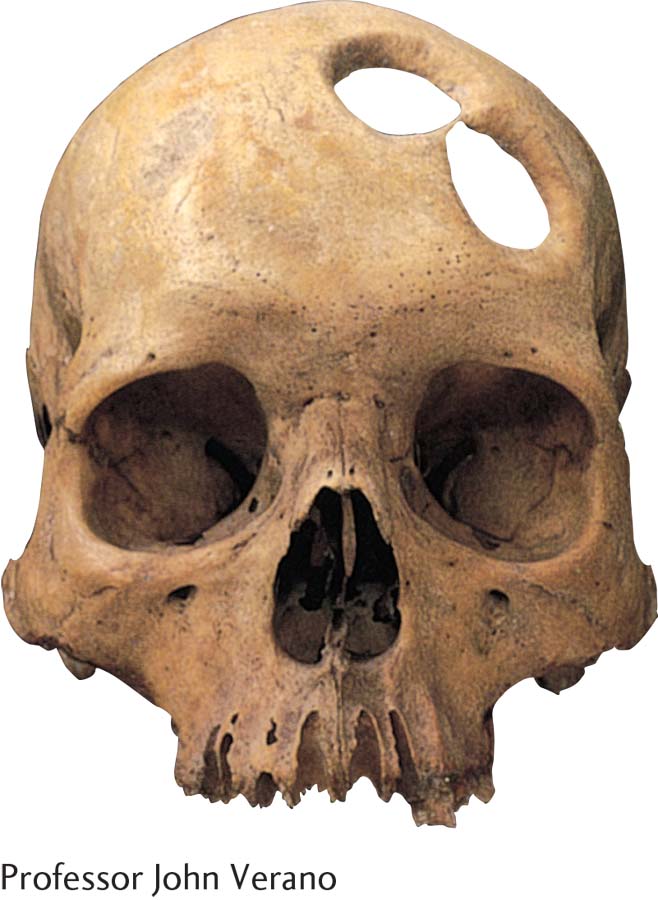
trephination An ancient operation in which a stone instrument was used to cut away a circular section of the skull, perhaps to treat abnormal behavior.
This supernatural view of abnormality may have begun as far back as the Stone Age, a half-
Later societies also explained abnormal behavior by pointing to possession by demons. Egyptian, Chinese, and Hebrew writings all account for psychological deviance this way, and the Bible describes how an evil spirit from the Lord affected King Saul and how David pretended to be mad to convince his enemies that he was visited by divine forces.
What demonological explanations or treatments, besides exorcism, are still around today, and why do they persist?
The treatment for abnormality in these early societies was often exorcism. The idea was to coax the evil spirits to leave or to make the person’s body an uncomfortable place in which to live. A shaman, or priest, might recite prayers, plead with the evil spirits, insult the spirits, perform magic, make loud noises, or have the person drink bitter potions. If these techniques failed, the shaman performed a more extreme form of exorcism, such as whipping or starving the person.
Greek and Roman Views and Treatments
humors According to the Greeks and Romans, bodily chemicals that influence mental and physical functioning.
In the years from roughly 500 B.C. to 500 A.D., when the Greek and Roman civilizations thrived, philosophers and physicians often offered different explanations and treatments for abnormal behaviors. Hippocrates (460–
To treat psychological dysfunctioning, Hippocrates sought to correct the underlying physical pathology. He believed, for instance, that the excess of black bile underlying sadness could be reduced by a quiet life, a diet of vegetables, exercise, celibacy, and even bleeding. Hippocrates’ focus on internal causes for abnormal behavior was shared by the great Greek philosophers Plato (427–
Europe in the Middle Ages: Demonology Returns
The enlightened views of Greek and Roman physicians and scholars were not enough to shake ordinary people’s belief in demons. And with the decline of Rome, demonological views and practices became popular once again. A growing distrust of science spread throughout Europe.
How might Twitter, text messaging, Instagram, Facebook, the Internet, or other technologies facilitate current forms of mass madness?
From 500 to 1350 A.D., the period known as the Middle Ages, the power of the clergy increased greatly throughout Europe. In those days the church rejected scientific forms of investigation, and it controlled all education. Religious beliefs, which were highly superstitious and demonological, came to dominate all aspects of life. Deviant behavior, particularly psychological dysfunctioning, was seen as evidence of Satan’s influence.
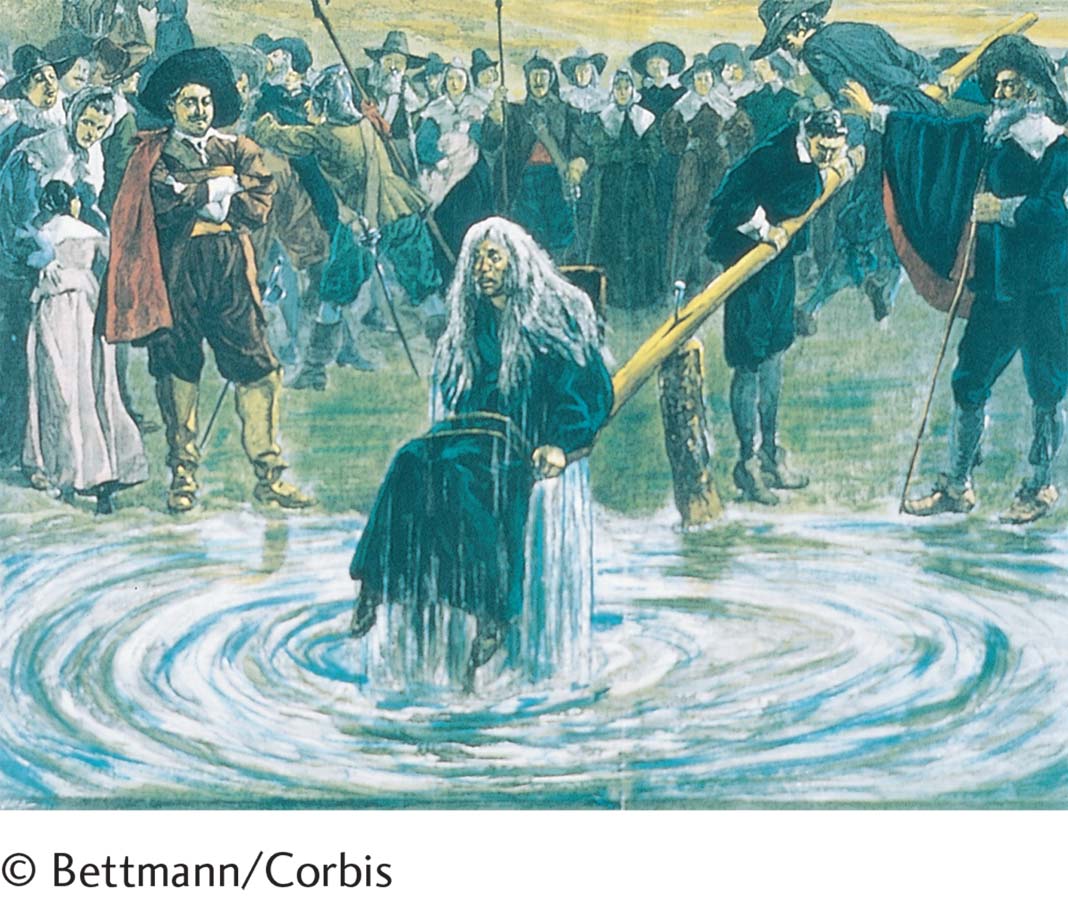
The Middle Ages were a time of great stress and anxiety—
Not surprisingly, some of the earlier demonological treatments for psychological abnormality reemerged during the Middle Ages. Once again the key to the cure was to rid the person’s body of the devil that possessed it. Exorcisms were revived, and clergymen, who generally were in charge of treatment during this period, would plead, chant, or pray to the devil or evil spirit (Sluhovsky, 2011, 2007). If these techniques did not work, they had others to try, some amounting to torture.
It was not until the Middle Ages drew to a close that demonology and its methods began to lose favor. Towns throughout Europe grew into cities, and government officials gained more power and took over nonreligious activities. Among their other responsibilities, they began to run hospitals and direct the care of people suffering from mental disorders. Medical views of abnormality gained favor once again, and many people with psychological disturbances received treatment in medical hospitals, such as the Trinity Hospital in England (Allderidge, 1979).
The Renaissance and the Rise of Asylums
During the early part of the Renaissance, a period of flourishing cultural and scientific activity from about 1400 to 1700, demonological views of abnormality continued to decline. German physician Johann Weyer (1515–
The care of people with mental disorders improved in this atmosphere. In England, such individuals might be kept at home while their families were aided financially by the local parish. Across Europe, religious shrines were devoted to the humane and loving treatment of people with mental disorders. Perhaps the best known of these shrines was at Gheel in Belgium. Beginning in the fifteenth century, people came to Gheel from all over the world for psychic healing. Local residents welcomed these pilgrims into their homes, and many stayed on to form the world’s first “colony” of mental patients. Gheel was the forerunner of today’s community mental health programs (Guarnieri, 2009; Aring, 1975, 1974). Many patients still live in foster homes there, interacting with other residents, until they recover.
asylum A type of institution that first became popular in the sixteenth century to provide care for persons with mental disorders. Most became virtual prisons.
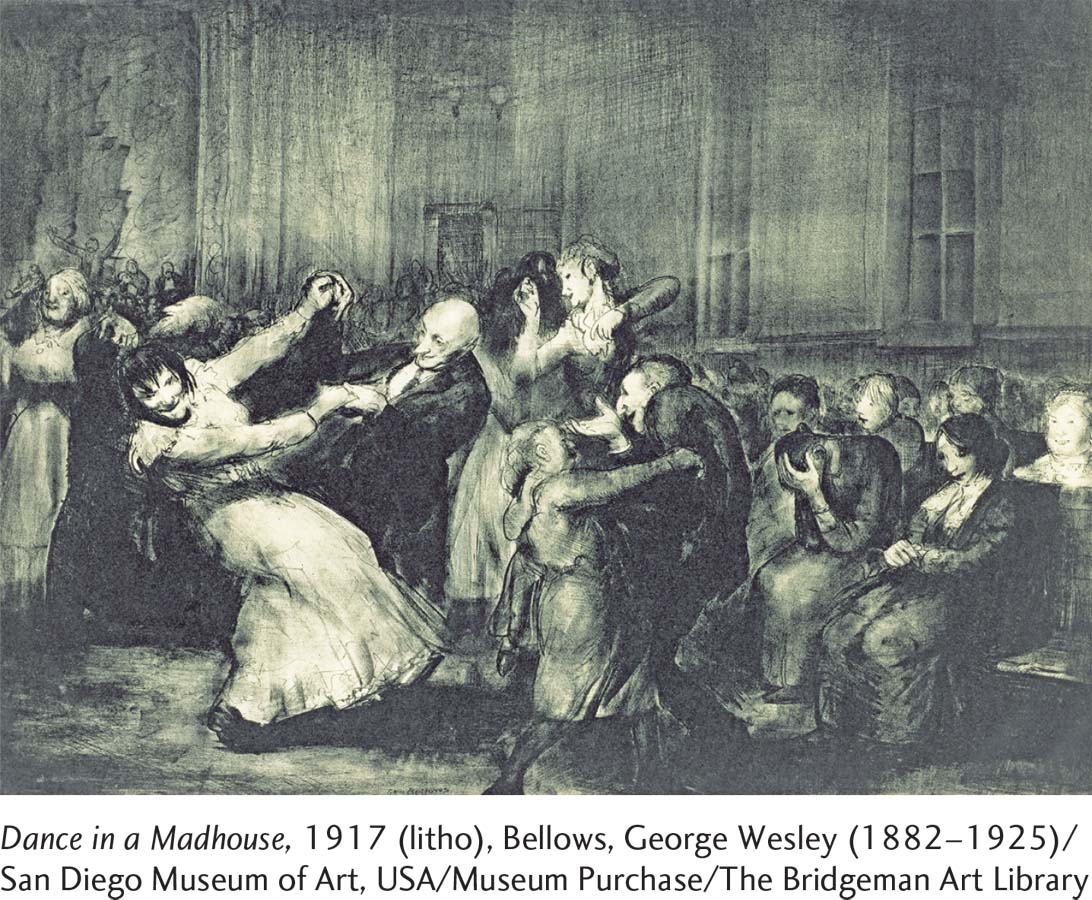
Unfortunately, these improvements in care began to fade by the mid-
In 1547, for example, Bethlehem Hospital was given to the city of London by Henry VIII for the sole purpose of confining the mentally ill. In this asylum, patients bound in chains cried out for all to hear. The hospital even became a popular tourist attraction; people were eager to pay to look at the howling and gibbering inmates. The hospital’s name, pronounced “Bedlam” by the local people, has come to mean a chaotic uproar (Selling, 1940).
The Nineteenth Century: Reform and Moral Treatment
Historians usually point to La Bicêtre, an asylum in Paris for male patients, as the first site of asylum reform. In 1793, during the French Revolution, Philippe Pinel (1745–
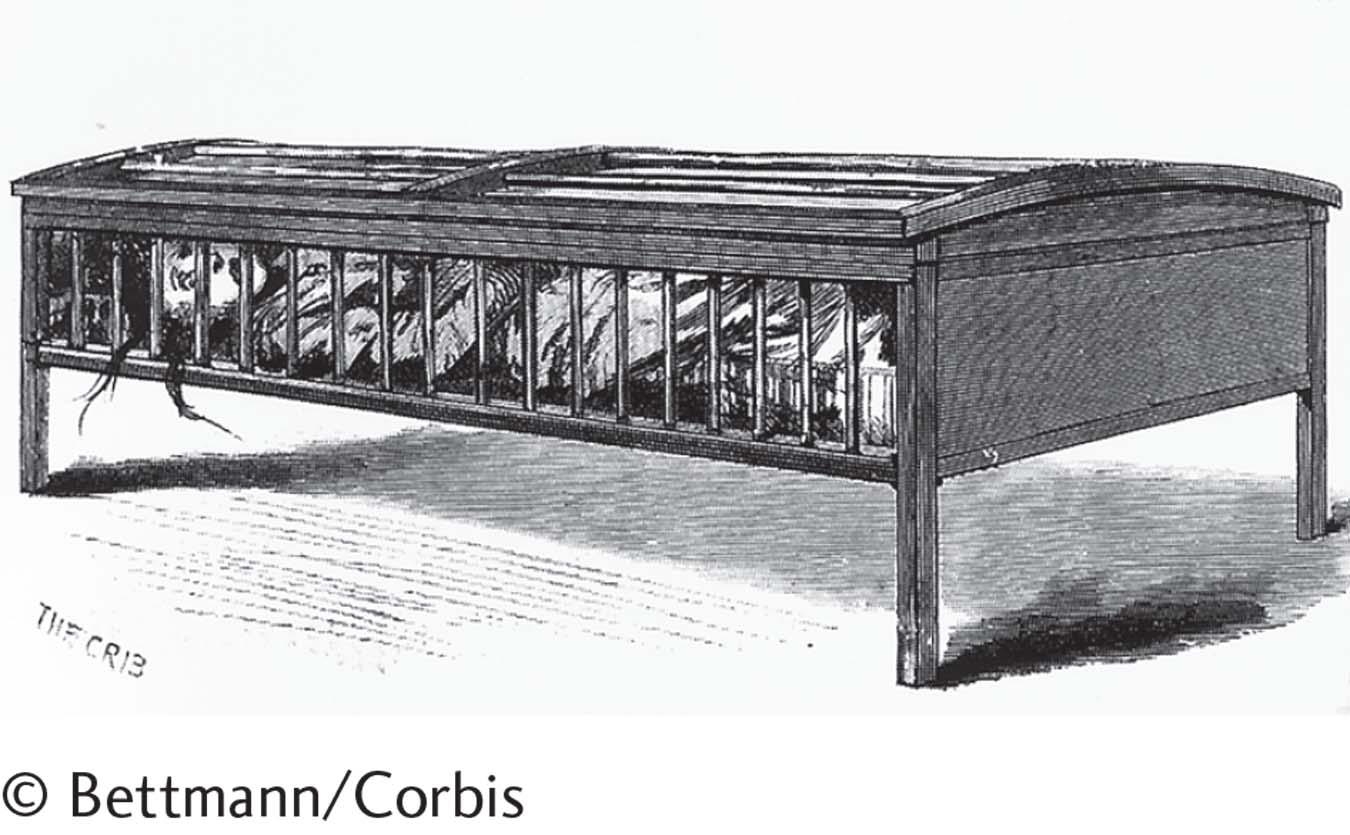
Meanwhile, an English Quaker named William Tuke (1732–
moral treatment A nineteenth-
The Spread of Moral Treatment The methods of Pinel and Tuke, called moral treatment because they emphasized moral guidance and humane and respectful techniques, caught on throughout Europe and the United States. Patients with psychological problems were increasingly perceived as potentially productive human beings who deserved individual care, including discussions of their problems, useful activities, work, companionship, and quiet.
The person most responsible for the early spread of moral treatment in the United States was Benjamin Rush (1745–
state hospitals State-
BETWEEN THE LINES
Early Asylums
Most of the patients in Middle Age asylums, from all classes and circumstances, were women.
The first asylum in colonial America was established in Williamsburg, Virginia, in 1773.
(faqs.org, 2014; Barton, 2004)
Rush’s work was influential, but it was a Boston schoolteacher named Dorothea Dix (1802–
The Decline of Moral Treatment By the 1850s, a number of mental hospitals throughout Europe and America reported success using moral approaches. By the end of that century, however, several factors led to a reversal of the moral treatment movement (Kazano, 2012). One factor was the speed with which the movement had spread. As mental hospitals multiplied, severe money and staffing shortages developed, recovery rates declined, and overcrowding in the hospitals became a major problem. Another factor was the assumption behind moral treatment that all patients could be cured if treated with humanity and dignity. For some, this was indeed sufficient. Others, however, needed more effective treatments than any that had yet been developed. An additional factor contributing to the decline of moral treatment was the emergence of a new wave of prejudice against people with mental disorders. The public came to view them as strange and dangerous, undeserving of donations or government funds. Moreover, many of the patients entering public mental hospitals in the United States in the late nineteenth century were poor foreign immigrants, whom the public had little interest in helping.
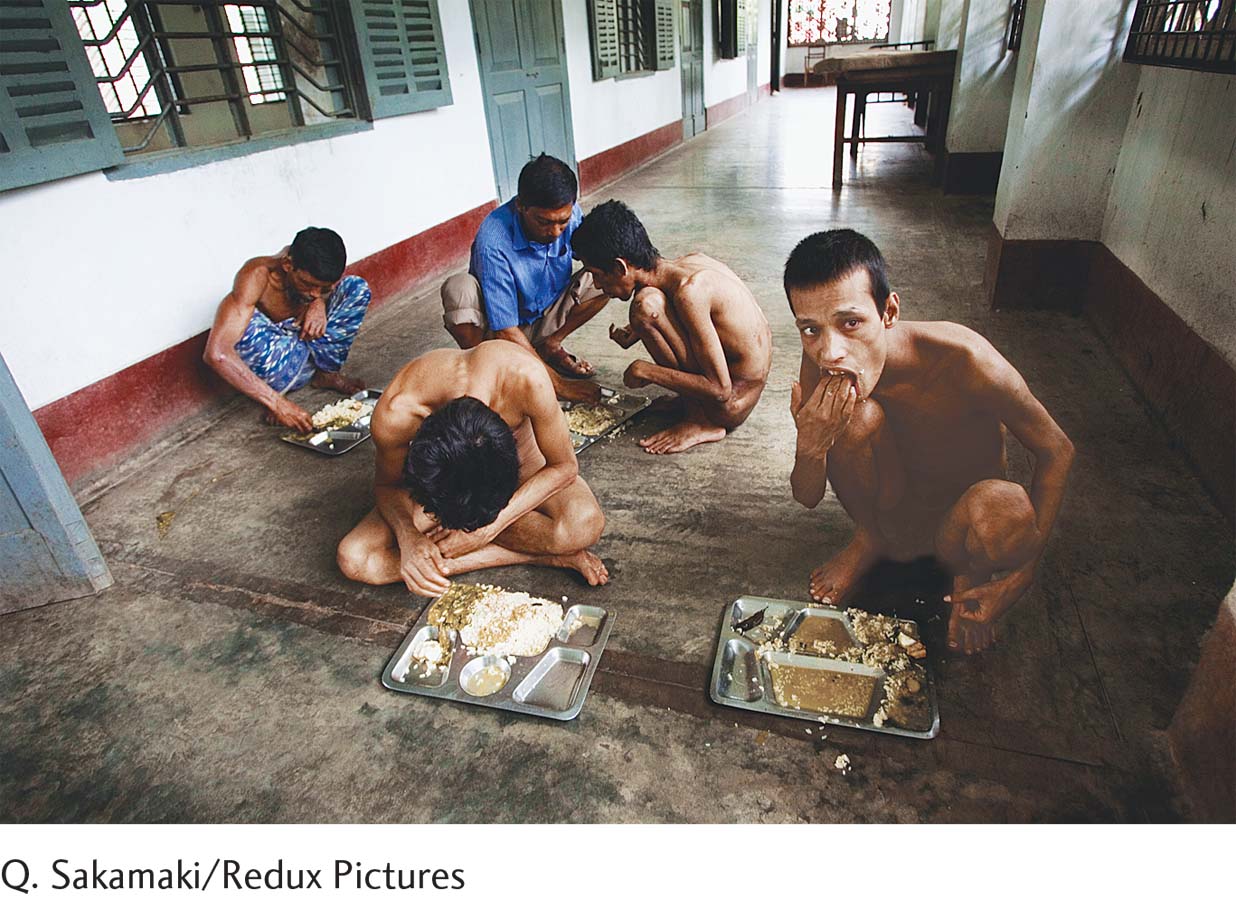
By the early years of the twentieth century, the moral treatment movement had ground to a halt in both the United States and Europe. Public mental hospitals were providing only custodial care and ineffective medical treatments and were becoming more overcrowded every year. Long-
The Early Twentieth Century: The Somatogenic and Psychogenic Perspectives
somatogenic perspective The view that abnormal psychological functioning has physical causes.
psychogenic perspective The view that the chief causes of abnormal functioning are psychological.
As the moral movement was declining in the late 1800s, two opposing perspectives emerged and began to compete for the attention of clinicians: the somatogenic perspective, the view that abnormal psychological functioning has physical causes, and the psychogenic perspective, the view that the chief causes of abnormal functioning are psychological. These perspectives came into full bloom during the twentieth century.
The Somatogenic Perspective The somatogenic perspective has at least a 2,400-
BETWEEN THE LINES
Famous Psych Lines from the Movies
“Crying helps me slow down and obsess over the weight of life’s problems.” (Inside Out, 2015)
“Do you have any idea how crazy you are?” (No Country for Old Men, 2007)
“Are you talkin’ to me?” (Taxi Driver, 1976)
“Mother’s not herself today.” (Psycho, 1960)
“Dave, my mind is going. I can feel it.” (2001: A Space Odyssey, 1968)
“I’m not going to be ignored!” (Fatal Attraction, 1987)
Two factors were responsible for this rebirth. One was the work of a distinguished German researcher, Emil Kraepelin (1856–
New biological discoveries also triggered the rise of the somatogenic perspective. One of the most important discoveries was that an organic disease, syphilis, led to general paresis, an irreversible disorder that featured both mental symptoms such as delusions of grandeur and physical ones like paralysis (Hogebrug et al., 2013). In 1897, German neurologist Richard von Krafft-
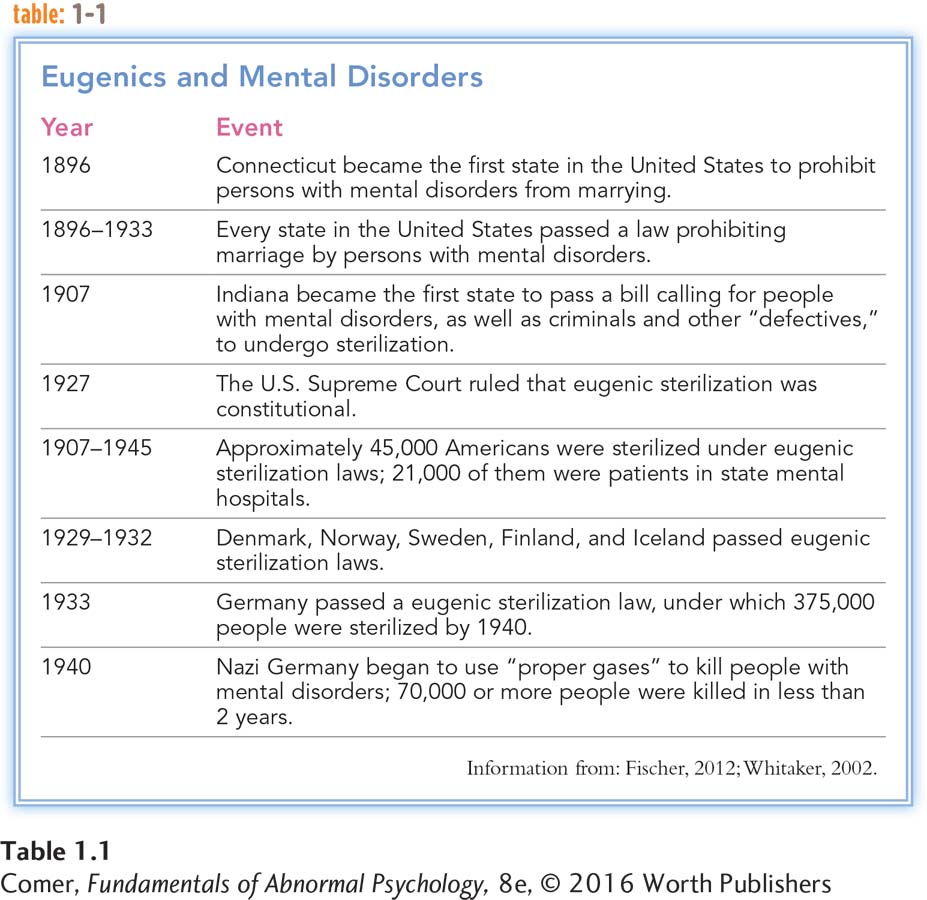
Despite the general optimism, biological approaches yielded mostly disappointing results throughout the first half of the twentieth century. Although many medical treatments were developed for patients in mental hospitals during that time, most of the techniques failed to work. Physicians tried tooth extraction, tonsillectomy, hydrotherapy (alternating hot and cold baths), and lobotomy, a surgical cutting of certain nerve fibers in the brain. Even worse, biological views and claims led, in some circles, to proposals for immoral solutions such as eugenic sterilization, the elimination (through medical or other means) of individuals’ ability to reproduce (see Table 1.1). Not until the 1950s, when a number of effective medications were finally discovered, did the somatogenic perspective truly begin to pay off for patients.
The Psychogenic Perspective The late 1800s also saw the emergence of the psychogenic perspective, the view that the chief causes of abnormal functioning are often psychological. This view, too, had a long history, but it did not gain much of a following until studies of hypnotism demonstrated its potential.
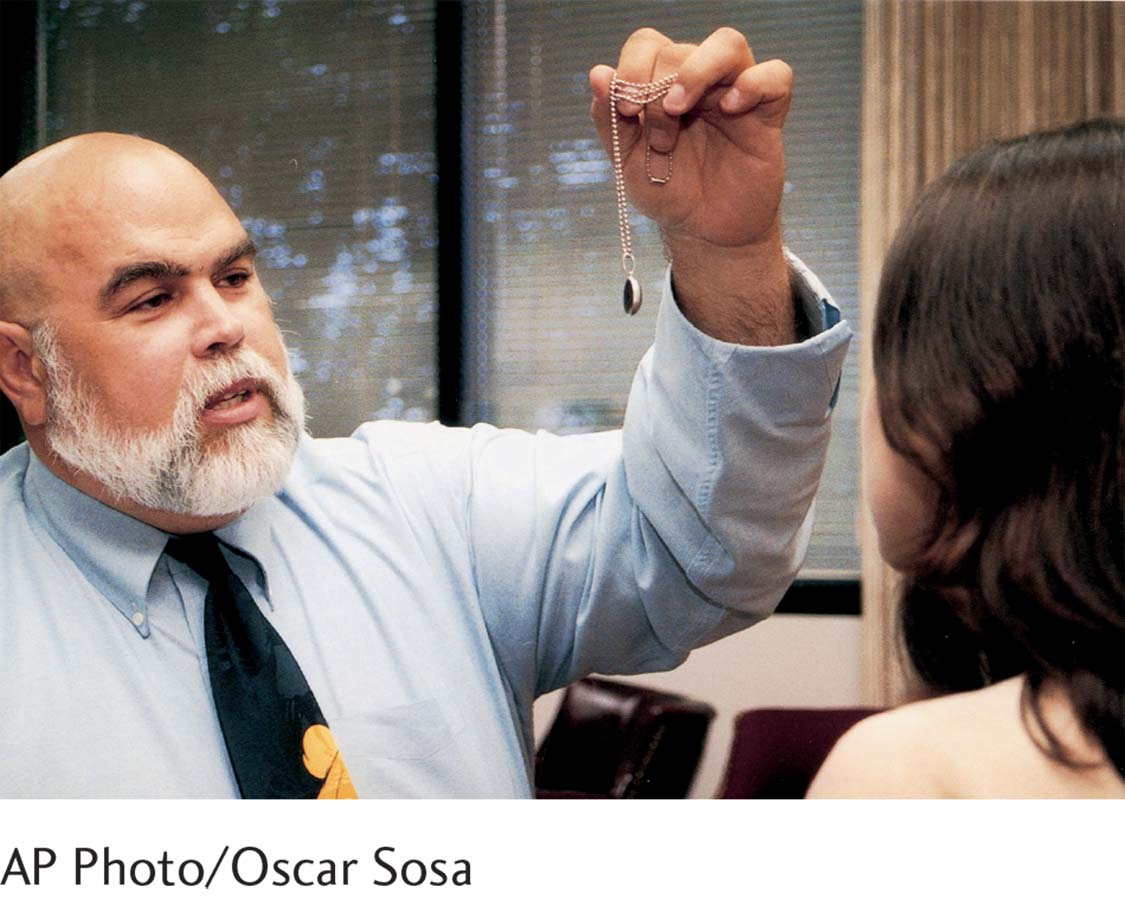
Hypnotism is a procedure in which a person is placed in a trancelike mental state during which he or she becomes extremely suggestible. It was used to help treat psychological disorders as far back as 1778, when an Austrian physician named Friedrich Anton Mesmer (1734–
It was not until years after Mesmer died that many researchers had the courage to investigate his procedure, later called hypnotism (from hypnos, the Greek word for “sleep”), and its effects on hysterical disorders. The experiments of two physicians practicing in the city of Nancy in France, Hippolyte-
psychoanalysis Either the theory or the treatment of abnormal mental functioning that emphasizes unconscious psychological forces as the cause of psychopathology.
Among those who studied the effects of hypnotism on hysterical disorders was Josef Breuer (1842–
BETWEEN THE LINES
All About Freud
Freud’s parents often favored Sigmund over his siblings.
Freud’s fee for one session of therapy was $20.
For almost 40 years, Freud treated patients 10 hours per day, 5 or 6 days per week.
Freud’s four sisters died in Nazi concentration camps.
Freud was nominated for the Nobel Prize in 12 different years, but never won.
(Nobel Media, 2014; Cherry, 2010; Hess, 2009; Gay, 2006, 1999; Jacobs, 2003)
Freud also developed the technique of psychoanalysis, a form of discussion in which clinicians help troubled people gain insight into their unconscious psychological processes. He believed that such insight, even without hypnotic procedures, would help the patients overcome their psychological problems. Freud and his followers offered treatment to patients in their offices for sessions of approximately an hour—
Summing Up
HOW WAS ABNORMALITY VIEWED AND TREATED IN THE PAST? The history of psychological disorders stretches back to ancient times. Prehistoric societies apparently viewed abnormal behavior as the work of evil spirits. There is evidence that Stone Age cultures used trephination, a primitive form of brain surgery, to treat abnormal behavior. People of early societies also sought to drive out evil spirits by exorcism.
Physicians of the Greek and Roman empires offered more enlightened explanations of mental disorders. Hippocrates believed that abnormal behavior was caused by an imbalance of the four bodily fluids, or humors.
Unfortunately, throughout history each period of enlightened thinking about psychological functioning has been followed by a period of backward thinking. In the Middle Ages, for example, Europeans returned to demonological explanations of abnormal behavior. The clergy was very influential and held that mental disorders were the work of the devil. As the Middle Ages drew to a close, such explanations and treatments began to decline, and care of people with mental disorders improved during the early part of the Renaissance. Certain religious shrines became dedicated to the humane treatment of such individuals. Unfortunately, this enlightened approach was short-
Care of people with mental disorders started to improve again in the nineteenth century. In Paris, Philippe Pinel started the movement toward moral treatment. In the United States, Dorothea Dix spearheaded a movement to ensure legal rights and protection for people with mental disorders and to establish state hospitals for their care. Unfortunately, the moral treatment movement disintegrated by the late nineteenth century, and mental hospitals again became warehouses where inmates received minimal care.
The turn of the twentieth century saw the return of the somatogenic perspective, the view that abnormal psychological functioning is caused primarily by physical factors. The same period saw the rise of the psychogenic perspective, the view that the chief causes of abnormal functioning are psychological. Sigmund Freud’s psychogenic approach, psychoanalysis, eventually gained wide acceptance and influenced future generations of clinicians.