4.5 Obsessive-Compulsive Disorder
obsession A persistent thought, idea, impulse, or image that is experienced repeatedly, feels intrusive, and causes anxiety.
compulsion A repetitive and rigid behavior or mental act that a person feels driven to perform in order to prevent or reduce anxiety.
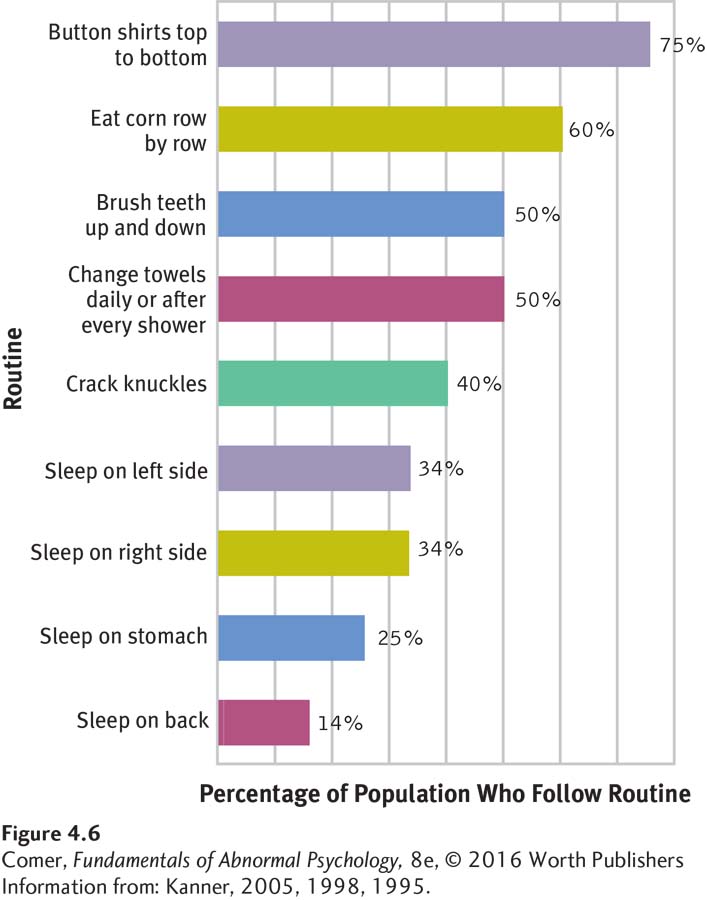
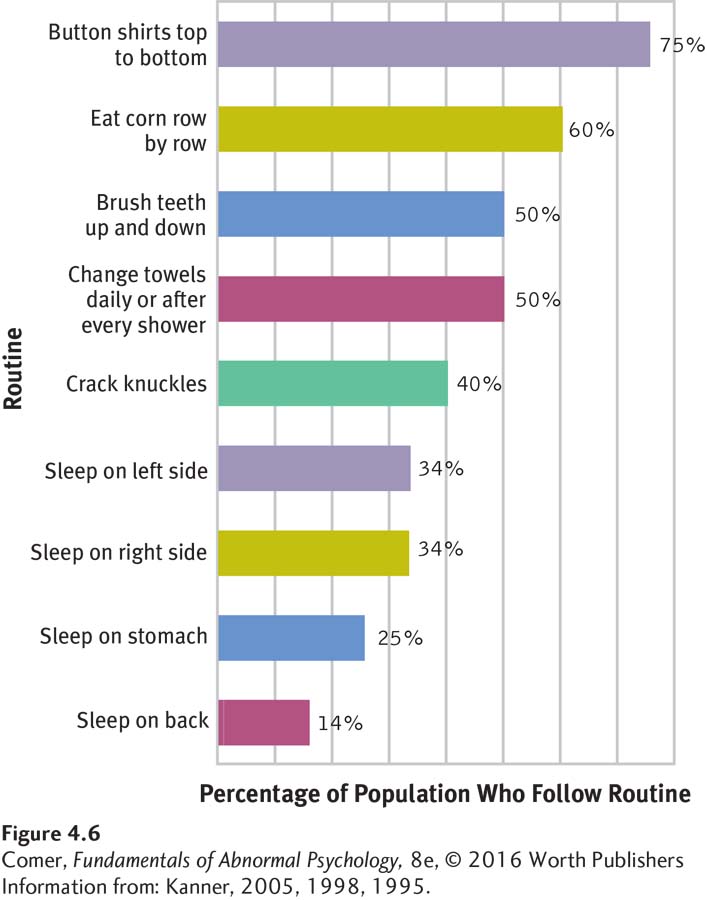
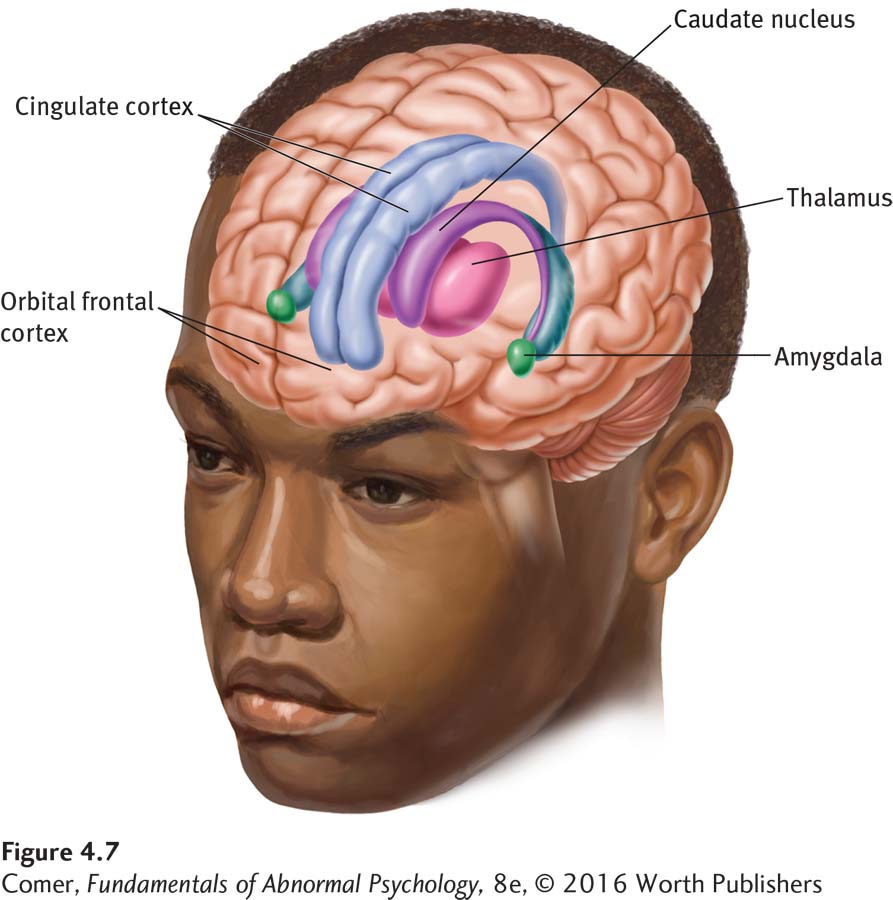
Figure 4.6: figure 4.6 Normal routines Most people find it comforting to follow set routines when they carry out everyday activities, and, in fact, 40 percent become irritated if they must depart from their routines. (Information from: Kanner, 2005, 1998, 1995.)
Obsessions are persistent thoughts, ideas, impulses, or images that seem to invade a person’s consciousness. Compulsions are repetitive and rigid behaviors or mental acts that people feel they must perform in order to prevent or reduce anxiety. As Figure 4.6 indicates, minor obsessions and compulsions are familiar to almost everyone. You may find yourself filled with thoughts about an upcoming performance or exam or keep wondering whether you forgot to turn off the stove or lock the door. You may feel better when you avoid stepping on cracks, turn away from black cats, or arrange your closet in a particular manner. Repetitive thoughts or behaviors of this kind, however, are hardly a reflection of abnormality.
obsessive-compulsive disorder A disorder in which a person has recurrent and unwanted thoughts, a need to perform repetitive and rigid actions, or both.
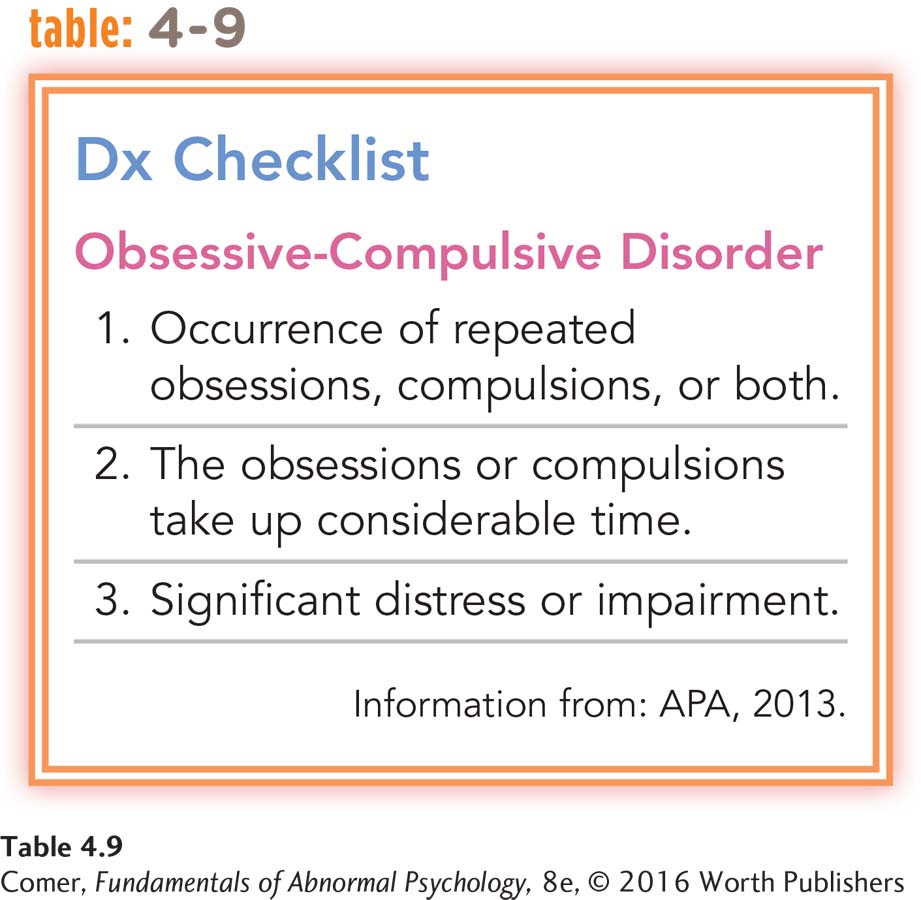
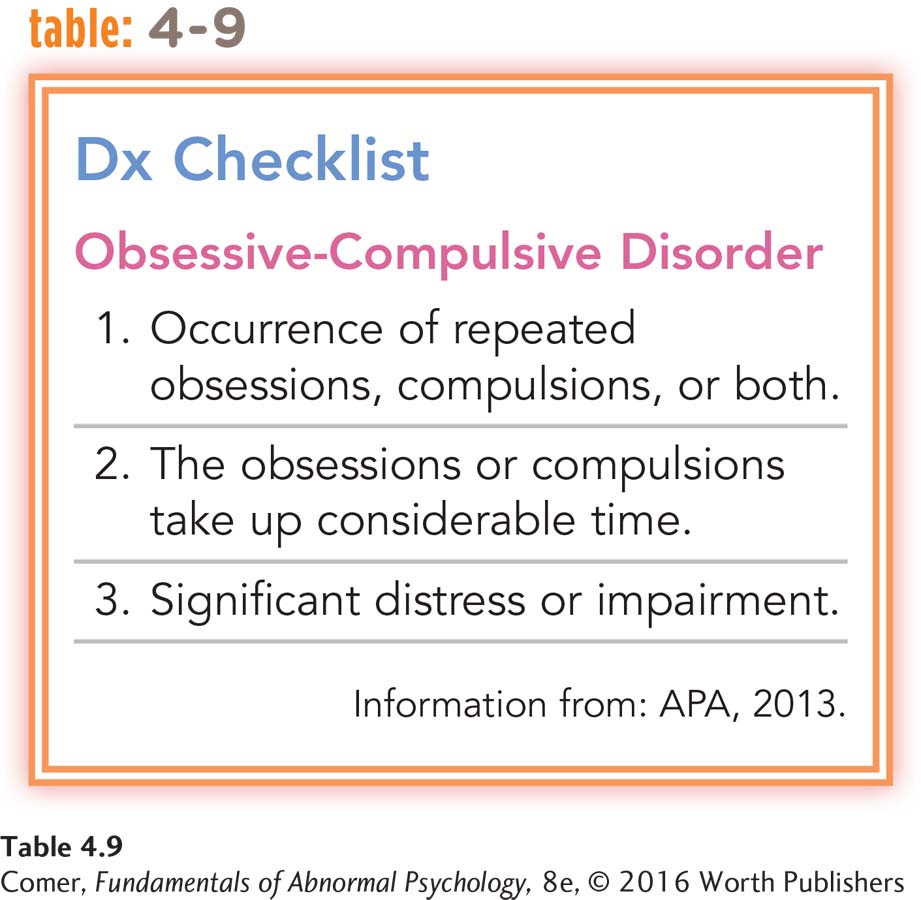
According to DSM-5, a diagnosis of obsessive-compulsive disorder is called for when obsessions or compulsions feel excessive or unreasonable, cause great distress, take up much time, and interfere with daily functions (see Table 4.9 below). Although obsessive-compulsive disorder is not classified as an anxiety disorder in DSM-5, anxiety does play a major role in this pattern. The obsessions cause intense anxiety, while the compulsions are aimed at preventing or reducing anxiety. In addition, anxiety rises if a person tries to resist his or her obsessions or compulsions.
An individual with this disorder observed: “I can’t get to sleep unless I am sure everything in the house is in its proper place so that when I get up in the morning, the house is organized. I work like mad to set everything straight before I go to bed, but, when I get up in the morning, I can think of a thousand things that I ought to do…. I can’t stand to know something needs doing and I haven’t done it” (McNeil, 1967, pp. 26–28). Research indicates that several additional disorders are closely related to obsessive-compulsive disorder in their features, causes, and treatment responsiveness, and so, as you will soon see, DSM-5 has grouped them together with obsessive-compulsive disorder.
Between 1 and 2 percent of the people in the United States and other countries throughout the world suffer from obsessive-compulsive disorder in any given year (Kessler et al., 2012; Björgvinsson & Hart, 2008). As many as 3 percent develop the disorder at some point during their lives. It is equally common in men and women and among people of different races and ethnic groups (Matsunaga & Seedat, 2011). The disorder usually begins by young adulthood and typically persists for many years, although its symptoms and their severity may fluctuate over time. It is estimated that more than 40 percent of people with obsessive-compulsive disorder may seek treatment, many for an extended period (Patel et al., 2014; Kessler et al., 1999, 1994).
What Are the Features of Obsessions and Compulsions?
Obsessive thoughts feel both intrusive and foreign to the people who experience them. Attempts to ignore or resist these thoughts may arouse even more anxiety, and before long they come back more strongly than ever. People with obsessions typically are quite aware that their thoughts are excessive.
Certain basic themes run through the thoughts of most people troubled by obsessive thinking (Bokor & Anderson, 2014). The most common theme appears to be dirt or contamination (Torres et al., 2013). Other common ones are violence and aggression, orderliness, religion, and sexuality.
Compulsions are similar to obsessions in many ways. For example, although compulsive behaviors are technically under voluntary control, the people who feel they must do them have little sense of choice in the matter. Most of these individuals recognize that their behavior is unreasonable, but they believe at the same time something terrible will happen if they don’t perform the compulsions. After performing a compulsive act, they usually feel less anxious for a short while. For some people the compulsive acts develop into detailed rituals. They must go through the ritual in exactly the same way every time, according to certain rules.
Cultural rituals Rituals do not necessarily reflect compulsions. Indeed, cultural and religious rituals often give meaning and comfort to their practitioners. Here Buddhist monks splash water over themselves during their annual winter prayers at a temple in Tokyo. This cleansing ritual is performed to pray for good luck.
Page 138
Like obsessions, compulsions take various forms. Cleaning compulsions are very common. People with these compulsions feel compelled to keep cleaning themselves, their clothing, or their homes. The cleaning may follow ritualistic rules and be repeated dozens or hundreds of times a day. People with checking compulsions check the same items over and over—door locks, gas taps, important papers—to make sure that all is as it should be. Another common compulsion is the constant effort to seek order or balance. People with this compulsion keep placing certain items (clothing, books, foods) in perfect order in accordance with strict rules. Touching, verbal, and counting compulsions are also common.
Although some people with obsessive-compulsive disorder experience obsessions only or compulsions only, most experience both. In fact, compulsive acts are often a response to obsessive thoughts. One study found that in most cases, compulsions seemed to represent a yielding to obsessive doubts, ideas, or urges (Akhtar et al., 1975). A woman who keeps doubting that her house is secure may yield to that obsessive doubt by repeatedly checking locks and gas jets, or a man who obsessively fears contamination may yield to that fear by performing cleaning rituals. The study also found that compulsions sometimes serve to help control obsessions. A teenager describes how she tried to control her obsessive fears of contamination by performing counting and verbal rituals:
| Patient: |
If I heard the word, like, something that had to do with germs or disease, it would be considered something bad, and so I had things that would go through my mind that were sort of like “cross that out and it’ll make it okay” to hear that word. |
| Interviewer: |
What sort of things? |
| Patient: |
Like numbers or words that seemed to be sort of like a protector. |
| Interviewer: |
What numbers and what words were they? |
| Patient: |
It started out to be the number 3 and multiples of 3 and then words like “soap and water,” something like that; and then the multiples of 3 got really high, and they’d end up to be 124 or something like that. It got real bad then. |
(Spitzer et al., 1981, p. 137)
Obsessive-compulsive disorder was once among the least understood of the psychological disorders. In recent decades, however, researchers have begun to learn more about it. The most influential explanations and treatments come from the psychodynamic, behavioral, cognitive, and biological models.
The Psychodynamic Perspective
As you have seen, psychodynamic theorists believe that an anxiety disorder develops when children come to fear their own id impulses and use ego defense mechanisms to lessen the resulting anxiety. What distinguishes obsessive-compulsive disorder from other anxiety disorders, in their view, is that here the battle between anxiety-provoking id impulses and anxiety-reducing defense mechanisms is not buried in the unconscious but is played out in overt thoughts and actions. The id impulses usually take the form of obsessive thoughts, and the ego defenses appear as counterthoughts or compulsive actions. A woman who keeps imagining her mother lying broken and bleeding, for example, may counter those thoughts with repeated safety checks throughout the house.
Page 139
Sigmund Freud traced obsessive-compulsive disorder to the anal stage of development (occurring at about 2 years of age). He proposed that during this stage some children experience intense rage and shame as a result of negative toilet-training experiences. Other psychodynamic theorists have argued instead that such early rage reactions are rooted in feelings of insecurity (Erikson, 1963; Sullivan, 1953; Horney, 1937). Either way, these children repeatedly feel the need to express their strong aggressive id impulses while at the same time knowing they should try to restrain and control the impulses. If this conflict between the id and ego continues, it may eventually blossom into obsessive-compulsive disorder. Overall, research has not clearly supported the psychodynamic explanation (Busch et al., 2010; Fitz, 1990).
When treating patients with obsessive-compulsive disorder, psychodynamic therapists try to help the individuals uncover and overcome their underlying conflicts and defenses, using the customary techniques of free association and therapist interpretation. Research has offered little evidence, however, that a traditional psychodynamic approach is of much help (Ponniah, Magiati, & Hollon, 2013). Thus some psychodynamic therapists now prefer to treat these patients with short-term psychodynamic therapies, which, as you saw in Chapter 2, are more direct and action-oriented than the classical techniques.
The Behavioral Perspective
Behaviorists have concentrated on explaining and treating compulsions rather than obsessions. They propose that people happen upon their compulsions quite randomly. In a fearful situation, they happen just coincidentally to wash their hands, say, or dress a certain way. When the threat lifts, they link the improvement to that particular action. After repeated accidental associations, they believe that the action is bringing them good luck or actually changing the situation, and so they perform the same actions again and again in similar situations. The act becomes a key method of avoiding or reducing anxiety (Grayson, 2014; Frost & Steketee, 2001).
Have you ever tried an informal version of exposure and response prevention in order to stop behaving in certain ways?
Famous clinical scientist Stanley Rachman and his associates have shown that compulsions do appear to be rewarded by a reduction in anxiety. In one of their experiments, for example, 12 research participants with compulsive hand-washing rituals were placed in contact with objects that they considered contaminated (Hodgson & Rachman, 1972). As behaviorists would predict, the hand-washing rituals of these participants seemed to lower their anxiety.

Getting down and dirty In one exposure and response prevention assignment, clients with cleaning compulsions might be instructed to do heavy-duty gardening and then resist washing their hands or taking a shower. They may never go so far as to participate in and enjoy mud wrestling, like these delightfully filthy individuals at the annual Mud Day event in Westland, Michigan, but you get the point.
exposure and response prevention A behavioral treatment for obsessive-compulsive disorder that exposes a client to anxiety-arousing thoughts or situations and then prevents the client from performing his or her compulsive acts. Also called exposure and ritual prevention.
If people keep performing compulsive behaviors in order to prevent bad outcomes and ensure positive outcomes, can’t they be taught that such behaviors are not really serving this purpose? In a behavioral treatment called exposure and response prevention (or exposure and ritual prevention), first developed by psychiatrist Victor Meyer (1966), clients are repeatedly exposed to objects or situations that produce anxiety, obsessive fears, and compulsive behaviors, but they are told to resist performing the behaviors they feel so bound to perform. Because people find it very difficult to resist such behaviors, therapists may set an example first.
According to surveys, almost half of adults double back after leaving home to make sure they have turned off an appliance.
More than half of all people who use an alarm clock check it repeatedly to be sure they’ve set it.
Page 140
Many behavioral therapists now use exposure and response prevention in both individual and group therapy formats. Some of them also have people carry out self-help procedures at home (Franklin & Foa, 2014). That is, they assign homework in exposure and response prevention, such as these assignments given to a woman with a cleaning compulsion:
Do not mop the floor of your bathroom for a week. After this, clean it within three minutes, using an ordinary mop. Use this mop for other chores as well without cleaning it.
Buy a fluffy mohair sweater and wear it for a week. When taking it off at night do not remove the bits of fluff. Do not clean your house for a week.
You, your husband, and children all have to keep shoes on. Do not clean the house for a week.
Drop a cookie on the contaminated floor, pick the cookie up and eat it.
Leave the sheets and blankets on the floor and then put them on the beds. Do not change these for a week.
(Emmelkamp, 1982, pp. 299–300)
Eventually this woman was able to set up a reasonable routine for cleaning herself and her home.
Between 55 and 85 percent of clients with obsessive-compulsive disorder have been found to improve considerably with exposure and response prevention, improvements that often continue indefinitely (Abramowitz et al., 2011, 2008; McKay, Taylor, & Abramowitz, 2010). The effectiveness of this approach suggests that people with this disorder are like the superstitious man in the old joke who keeps snapping his fingers to keep elephants away. When someone points out, “But there aren’t any elephants around here,” the man replies, “See? It works!” One review concludes, “With hindsight, it is possible to see that the [obsessive-compulsive] individual has been snapping his fingers, and unless he stops (response prevention) and takes a look around at the same time (exposure), he isn’t going to learn much of value about elephants” (Berk & Efran, 1983, p. 546).
The Cognitive Perspective

Personal knowledge The HBO hit series Girls follows the struggles of Hannah Horvath and her friends as they navigate their 20s, “one mistake at a time.” The show’s creator and star, Lena Dunham, says that Hannah’s difficulties often are inspired by her own real-life experiences, including her childhood battle with OCD and anxiety.
neutralizing A person’s attempt to eliminate unwanted thoughts by thinking or behaving in ways that put matters right internally, making up for the unacceptable thoughts.
Cognitive theorists begin their explanation of obsessive-compulsive disorder by pointing out that everyone has repetitive, unwanted, and intrusive thoughts. Anyone might have thoughts of harming others or being contaminated by germs, for example, but most people dismiss or ignore them with ease. Those who develop this disorder, however, typically blame themselves for such thoughts and expect that somehow terrible things will happen (Grayson, 2014; Salkovskis, 1999, 1985). To avoid such negative outcomes, they try to neutralize the thoughts—thinking or behaving in ways meant to put matters right or to make amends (Jacob et al., 2014; Salkovskis et al., 2003).
Neutralizing acts might include requesting special reassurance from others, deliberately thinking “good” thoughts, washing one’s hands, or checking for possible sources of danger. When a neutralizing effort brings about a temporary reduction in discomfort, it is reinforced and will likely be repeated. Eventually the neutralizing thought or act is used so often that it becomes, by definition, an obsession or compulsion. At the same time, the individual becomes more and more convinced that his or her unpleasant intrusive thoughts are dangerous. As the person’s fear of such thoughts increases, the thoughts begin to occur more frequently and they, too, become obsessions.
Page 141
In support of this explanation, studies have found that people with obsessive-compulsive disorder have intrusive thoughts more often than other people, resort to more elaborate neutralizing strategies, and experience reductions in anxiety after using neutralizing techniques (Jacob et al., 2014; Salkovskis et al., 2003).
Although everyone sometimes has undesired thoughts, only some people develop obsessive-compulsive disorder. Why do these individuals find such normal thoughts so disturbing to begin with? Researchers have found that this population tends (1) to have exceptionally high standards of conduct and morality (Whitton, Henry, & Grisham, 2014; Rachman, 1993), (2) to believe intrusive negative thoughts are equivalent to actions and capable of causing harm (Lawrence & Williams, 2011), and (3) to believe that they should have perfect control over all of their thoughts and behaviors in life (Gelfand & Radomsky, 2013).
Cognitive therapists help clients focus on the cognitive processes involved in their obsessive-compulsive disorder. Initially, they educate the clients, pointing out how misinterpretations of unwanted thoughts, an excessive sense of responsibility, and neutralizing acts help produce and maintain their symptoms. The therapists then guide the clients to identify, challenge, and change their distorted cognitions. It appears that cognitive techniques of this kind often help reduce the number and impact of obsessions and compulsions (Franklin & Foa, 2014). While the behavioral approach (exposure and response prevention) and the cognitive approach have each been of help to clients with obsessive-compulsive disorder, some research suggests that a combination of the two approaches is often more effective than either intervention alone (Grayson, 2014; McKay et al., 2010).
The Biological Perspective
In recent years, two lines of research have uncovered more direct evidence that biological factors play a key role in obsessive-compulsive disorder, and promising biological treatments for the disorder have been developed as well. This research points to (1) abnormally low activity of the neurotransmitter serotonin and (2) abnormal functioning in key regions of the brain.
serotonin A neurotransmitter whose abnormal activity is linked to depression, obsessive-compulsive disorder, and eating disorders.
Serotonin, like GABA and norepinephrine, is a brain chemical that carries messages from neuron to neuron. The first clue to its role in obsessive-compulsive disorder was, once again, a surprising finding by clinical researchers—this time that two antidepressant drugs, clomipramine and fluoxetine (Anafranil and Prozac), reduce obsessive and compulsive symptoms (Bokor & Anderson, 2014). Since these particular drugs increase serotonin activity, some researchers concluded that the disorder might be caused by low serotonin activity. In fact, only those antidepressant drugs that increase serotonin activity help in cases of obsessive-compulsive disorder; antidepressants that mainly affect other neurotransmitters typically have little or no effect on it (Jenike, 1992). Although serotonin is the neurotransmitter most often cited in explanations of obsessive-compulsive disorder, recent studies have suggested that other neurotransmitters, particularly glutamate, GABA, and dopamine, may also play important roles in the development of the disorder (Bokor & Anderson, 2014).
orbitofrontal cortex A region of the brain in which impulses involving excretion, sexuality, violence, and other primitive activities normally arise.
caudate nuclei Structures in the brain, within the region known as the basal ganglia, that help convert sensory information into thoughts and actions.
Another line of research has linked obsessive-compulsive disorder to the abnormal functioning of specific regions of the brain, particularly the orbitofrontal cortex (just above each eye) and the caudate nuclei (structures located within the brain region known as the basal ganglia). These regions are part of a brain circuit that usually converts sensory information into thoughts and actions. The circuit begins in the orbitofrontal cortex, where sexual, violent, and other primitive impulses normally arise. These impulses next move on to the caudate nuclei, which act as filters that send only the most powerful impulses on to the thalamus, the next stop on the circuit (see Figure 4.7). If impulses reach the thalamus, the person is driven to think further about them and perhaps to act. Many theorists now believe that either the orbitofrontal cortex or the caudate nuclei of some people are too active, leading to a constant eruption of troublesome thoughts and actions (Endrass et al., 2011). Additional parts of this brain circuit have also been identified in recent years, including the cingulate cortex and, yet again, the amygdala (Via et al., 2014; Stein & Fineberg, 2007).
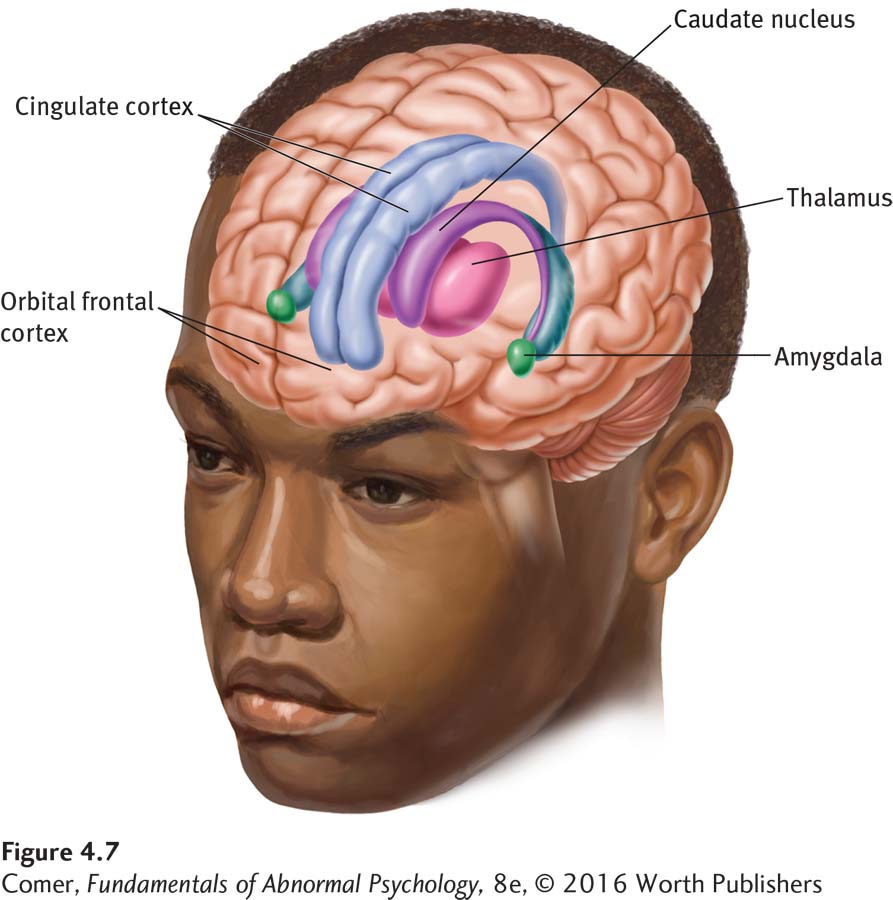
Figure 4.7: figure 4.7 The biology of obsessive-compulsive disorder Brain structures that have been linked to obsessive-compulsive disorder include the orbitofrontal cortex, caudate nucleus, thalamus, amygdala, and cingulate cortex. The structures may be too active in people with the disorder.
Page 142
In support of this brain circuit explanation, medical scientists have observed for years that obsessive-compulsive symptoms do sometimes arise or subside after the orbitofrontal cortex, caudate nuclei, or other regions in the circuit are damaged by accident or illness (Hofer et al., 2013). Similarly, brain scan studies have shown that the caudate nuclei and the orbitofrontal cortex of research participants with obsessive-compulsive disorder are more active than those of control participants (Marsh et al., 2014; Baxter et al., 2001, 1990).
The serotonin and brain circuit explanations may themselves be linked. It turns out that serotonin—along with the neurotransmitters glutamate, GABA, and dopamine—plays a key role in the operation of the orbitofrontal cortex, caudate nuclei, and other parts of the brain circuit; certainly abnormal activity by one or more of these neurotransmitters could be contributing to the improper functioning of the circuit.
Ever since researchers first discovered that particular antidepressant drugs help to reduce obsessions and compulsions, these drugs have been used to treat obsessive-compulsive disorder (Bokor & Anderson, 2014). We now know that the drugs not only increase brain serotonin activity but also help produce more normal activity in the orbitofrontal cortex and caudate nuclei (McCabe & Mishor, 2011). Studies have found that these antidepressant drugs bring improvement to between 50 and 80 percent of those with obsessive-compulsive disorder (Bareggi et al., 2004). The obsessions and compulsions do not usually disappear totally, but on average they are cut almost in half within 8 weeks of treatment (DeVeaugh-Geiss et al., 1992).
An Obsession That Changed the World
The experiments that led Louis Pasteur to the pasteurization process may have been driven in part by his obsession with contamination and infection. Apparently he would not shake hands and regularly wiped his glass and plate before dining (Asimov, 1997).
People who are treated with such drugs alone, however, tend to relapse if their medication is stopped. Thus, more and more individuals with obsessive-compulsive disorder are now being treated by a combination of behavioral, cognitive, and drug therapies. According to research, such combinations often yield higher levels of symptom reduction and bring relief to more clients than do each of the approaches alone—improvements that may continue for years (Romanelli et al., 2014; Simpson et al., 2013).
Obviously, the treatment picture for obsessive-compulsive disorder has improved greatly over the past 15 years, and indeed, this disorder is now helped by several forms of treatment, often used in combination. In fact, some studies suggest that the behavioral, cognitive, and biological approaches may ultimately have the same effect on the brain. In these investigations, both participants who responded to cognitive-behavioral treatments and those who responded to antidepressant drugs showed marked reductions in activity in the caudate nuclei and other parts of the obsessive-compulsive brain circuit (Jabr, 2013; Baxter et al., 2000, 1992).
Obsessive-Compulsive-Related Disorders
Page 143
Some people perform particular patterns of repetitive and excessive behavior that greatly disrupt their lives. Among the most common such patterns are excessive appearance-checking, hoarding, hair-pulling, and skin-picking. DSM-5 has created the group name obsessive-compulsive-related disorders and assigned four of these patterns to that group: hoarding disorder, trichotillomania (hair-pulling disorder), excoriation (skin-picking) disorder, and body dysmorphic disorder. Collectively, these four disorders are displayed by at least 5 percent of all people (Frost et al., 2012; Keuthen et al., 2012, 2010; Wolrich, 2011).
hoarding disorder A disorder in which individuals feel compelled to save items and become very distressed if they try to discard them, resulting in an excessive accumulation of items.
People who display hoarding disorder feel that they must save items, and they become very distressed if they try to discard them (APA, 2013). These feelings make it difficult for them to part with possessions, resulting in an extraordinary accumulation of items that clutters their lives and living areas. This pattern causes the individuals significant distress and may greatly impair their personal, social, or occupational functioning (Ong et al., 2015; Frost et al., 2012). It is common for them to wind up with numerous useless and valueless items, from junk mail to broken objects to unused clothes. Parts of their homes may become inaccessible because of the clutter. For example, sofas, kitchen appliances, or beds may be unusable. In addition, the pattern often results in fire hazards, unhealthful sanitation conditions, or other dangers.
trichotillomania A disorder in which people repeatedly pull out hair from their scalp, eyebrows, eyelashes, or other parts of the body. Also called hair-pulling disorder.
People with trichotillomania, also known as hair-pulling disorder, repeatedly pull out hair from their scalp, eyebrows, eyelashes, or other parts of the body (APA, 2013). The disorder usually centers on just one or two of these body sites, most often the scalp. Typically, those with the disorder pull one hair at a time. It is common for anxiety or stress to trigger or accompany the hair-pulling behavior. Some sufferers follow specific rituals as they pull their hair, including pulling until the hair feels “just right” and selecting certain types of hairs for pulling (Starcevic, 2015; Keuthen et al., 2012). Because of the distress, impairment, or embarrassment caused by this behavior, the individuals often try to reduce or stop the hair-pulling. The term “trichotillomania” is derived from the Greek for “frenzied hair-pulling.”
excoriation disorder A disorder in which people repeatedly pick at their skin, resulting in significant sores or wounds. Also called skin-picking disorder.
People with excoriation (skin-picking) disorder keep picking at their skin, resulting in significant sores or wounds (APA, 2013). Like those with hair-pulling disorder, they often try to reduce or stop the behavior. Most sufferers pick with their fingers and center their picking on one area, most often the face (Grant et al., 2015, 2012; Odlaug & Grant, 2012). Other common areas of focus include the arms, legs, lips, scalp, chest, and extremities such as fingernails and cuticles. The behavior is typically triggered or accompanied by anxiety or stress.

A messy aftermath This man prepares to clean out his mother’s home after her death. This is not an easy task–emotionally or physically–under the best of circumstances, but it is particularly difficult in this instance: his mother had suffered from hoarding disorder.
Page 144
body dysmorphic disorder A disorder in which individuals become preoccupied with the belief that they have certain defects or flaws in their physical appearance. Such defects or flaws are imagined or greatly exaggerated.
People with body dysmorphic disorder become preoccupied with the belief that they have a particular defect or flaw in their physical appearance. Actually, the perceived defect or flaw is imagined or greatly exaggerated in the person’s mind (APA, 2013). Such beliefs drive the individuals to repeatedly check themselves in the mirror, groom themselves, pick at the perceived flaw, compare themselves with others, seek reassurance, or perform other, similar behaviors. Here, too, those with the problem experience significant distress or impairment.
Body dysmorphic disorder is the obsessive-compulsive-related disorder that has received the most study to date. Researchers have found that, most often, individuals with this problem focus on wrinkles; spots on the skin; excessive facial hair; swelling of the face; or a misshapen nose, mouth, jaw, or eyebrow (Fang & Wilhelm, 2015; Veale & Bewley, 2015). Some worry about the appearance of their feet, hands, breasts, penis, or other body parts. Still others, like the woman described here, are concerned about bad odors coming from sweat, breath, genitals, or the rectum.
A woman of 35 had for 16 years been worried that her sweat smelled terrible…. For fear that she smelled, for 5 years she had not gone out anywhere except when accompanied by her husband or mother. She had not spoken to her neighbors for 3 years…. She avoided cinemas, dances, shops, cafes, and private homes…. Her husband was not allowed to invite any friends home; she constantly sought reassurance from him about her smell…. Her husband bought all her new clothes as she was afraid to try on clothes in front of shop assistants. She used vast quantities of deodorant and always bathed and changed her clothes before going out, up to 4 times daily.
Worldwide influence A lingerie ad in a subway station in Shanghai, China, displays a woman in a push-up bra. As West meets East, Asian women have been bombarded by ads encouraging them to make Western-like changes to their various body parts. Perhaps not so coincidentally, cases of body dysmorphic disorder among Asians are becoming more and more similar to those among Westerners.
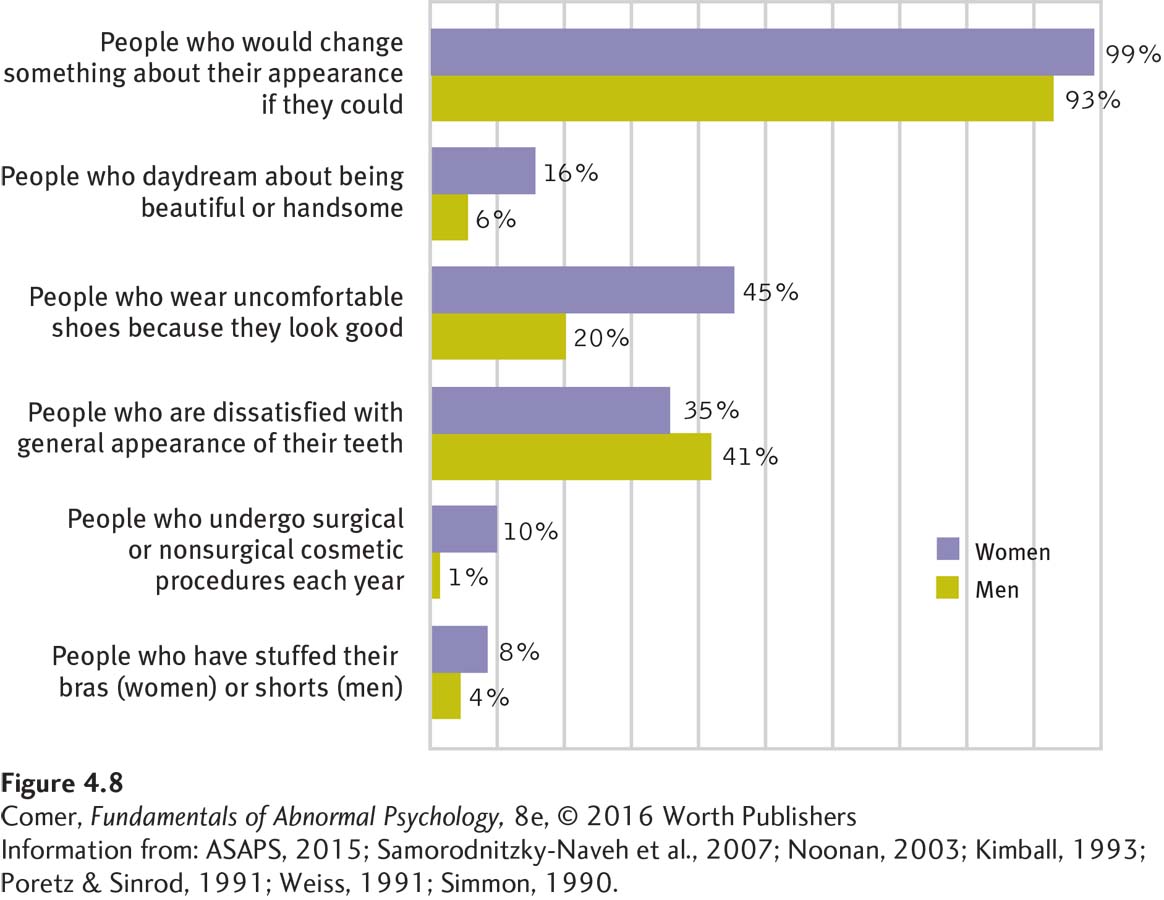
Of course, it is common in our society to worry about appearance (see Figure 4.8). Many teenagers and young adults worry about acne, for instance. The concerns of people with body dysmorphic disorder, however, are extreme. Sufferers may severely limit contact with other people, be unable to look others in the eye, or go to great lengths to conceal their “defects”—say, always wearing sunglasses to cover their supposedly misshapen eyes. As many as half of people with the disorder seek plastic surgery or dermatology treatment, and often they feel worse rather than better afterward (Dey et al., 2015; McKay et al., 2008). A large number are housebound, and more than 10 percent may attempt suicide (Buhlmann et al., 2010; Phillips et al., 1993).
As with the other obsessive-compulsive-related disorders, theorists typically account for body dysmorphic disorder by using the same kinds of explanations, both psychological and biological, that have been applied to obsessive-compulsive disorder (Hartmann et al., 2015; Witthöft & Hiller, 2010). Similarly, clinicians typically treat clients with this disorder by applying the kinds of treatment used with obsessive-compulsive disorder, particularly antidepressant drugs, exposure and response prevention, and cognitive therapy (Fang & Wilhelm, 2015; Krebs et al., 2012).
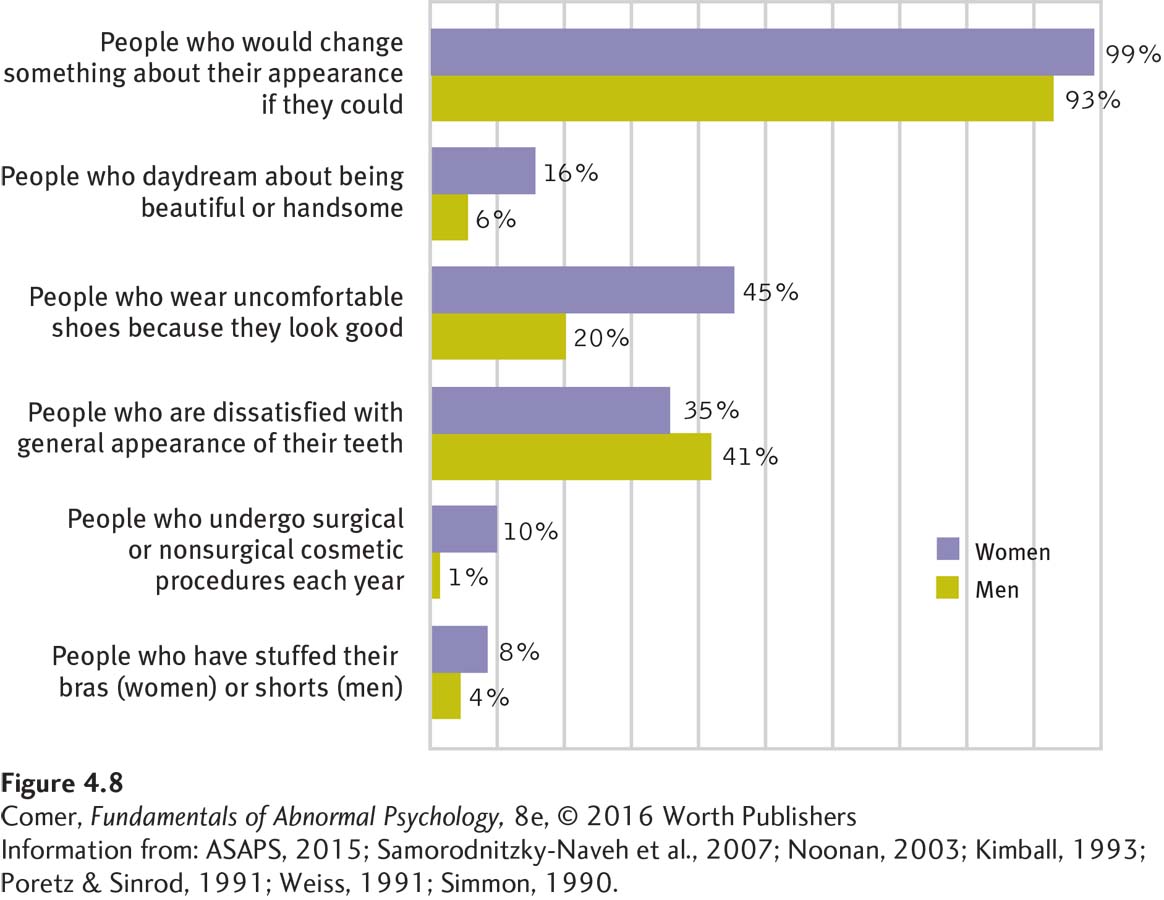
Figure 4.8: figure 4.8 “Mirror, mirror, on the wall …” People with body dysmorphic disorder are not the only ones who have concerns about their appearance. Surveys find that in our appearance-conscious society, large percentages of people regularly think about and try to change the way they look. (Information from: ASAPS, 2015; Samorodnitzky-Naveh et al., 2007; Noonan, 2003; Kimball, 1993; Poretz & Sinrod, 1991; Weiss, 1991; Simmon, 1990.)
Page 145
In one study, for example, 17 clients with this disorder were treated with exposure and response prevention. Over the course of 4 weeks, the clients were repeatedly reminded of their perceived physical defects and, at the same time, prevented from doing anything to help reduce their discomfort (such as checking their appearance) (Neziroglu et al., 2004, 1996). By the end of treatment, these individuals were less concerned with their “defects” and spent less time checking their body parts and avoiding social interactions.
Summing Up
OBSESSIVE-COMPULSIVE DISORDER People with obsessive-compulsive disorder are beset by obsessions, perform compulsions, or both. Compulsions are often a response to a person’s obsessive thoughts.
People who try to avoid all contamination and rid themselves and their world of all germs are fighting a losing battle. While talking, the average person sprays 300 microscopic saliva droplets per minute, or 2.5 per word.
According to the psychodynamic view, obsessive-compulsive disorder arises out of a battle between id impulses and ego defense mechanisms. Behaviorists believe that compulsive behaviors develop through chance associations. The leading behavioral treatment combines prolonged exposure with response prevention. Cognitive theorists believe that obsessive-compulsive disorder grows from a normal human tendency to have unwanted and unpleasant thoughts. The efforts of some people to understand, eliminate, or avoid such thoughts actually lead to obsessions and compulsions. Cognitive therapists educate clients and help them correct their misinterpretations of the unwanted thoughts. Research suggests that a combined cognitive-behavioral approach may be more effective than either therapy alone.
Biological researchers have tied obsessive-compulsive disorder to low serotonin activity and abnormal functioning in the orbitofrontal cortex and caudate nuclei. Antidepressant drugs that raise serotonin activity are a useful form of treatment.
Page 146
In addition to obsessive-compulsive disorder, DSM-5 lists a group of obsessive-compulsive-related disorders, disorders in which obsessive-like concerns drive individuals to repeatedly and excessively perform specific patterns of behavior that greatly disrupt their lives. This group consists of hoarding disorder, trichotillomania, excoriation (skin-picking) disorder, and body dysmorphic disorder.