12.1 The Clinical Picture of Schizophrenia
The symptoms of schizophrenia vary greatly from sufferer to sufferer, and so do its triggers, course, and responsiveness to treatment (APA, 2013). In fact, a number of clinicians believe that schizophrenia is actually a group of distinct disorders that happen to have some features in common (Boutros et al., 2014). Regardless of whether schizophrenia is a single disorder or several disorders, the lives of people who struggle with its symptoms are filled with pain and turmoil.
What Are the Symptoms of Schizophrenia?
Think back to Laura and Richard, the two people described at the beginning of the chapter. Both of them deteriorated from a normal level of functioning to become ineffective in dealing with the world. Each had some of the symptoms found in schizophrenia. The symptoms can be grouped into three categories: positive symptoms (excesses of thought, emotion, and behavior), negative symptoms (deficits of thought, emotion, and behavior), and psychomotor symptoms (unusual movements or gestures). Some people with schizophrenia are more dominated by positive symptoms and others by negative symptoms, although most tend to have both kinds of symptoms to some degree. In addition, around half of those with schizophrenia have significant difficulties with memory and other kinds of cognitive functioning (Ragland et al., 2015; Eich et al., 2014).
positive symptoms Symptoms of schizophrenia that seem to be excesses of or bizarre additions to normal thoughts, emotions, or behaviors.
Positive Symptoms Positive symptoms are “pathological excesses,” or bizarre additions, to a person’s behavior. Delusions, disorganized thinking and speech, heightened perceptions and hallucinations, and inappropriate affect are the ones most often found in schizophrenia.
delusion A strange false belief firmly held despite evidence to the contrary.
DELUSIONS Many people with schizophrenia develop delusions, ideas that they believe wholeheartedly but that have no basis in fact. Some people hold a single delusion that dominates their lives and behavior; others have many delusions. Delusions of persecution are the most common in schizophrenia (APA, 2013). People with such delusions believe they are being plotted or discriminated against, spied on, slandered, threatened, attacked, or deliberately victimized. Laura believed that her neighbors were trying to irritate her and that other people were trying to harm her and her husband.
Philosopher Friedrich Nietzsche said, “Insanity in individuals is something rare—
People with schizophrenia may also have delusions of reference: they attach special and personal meaning to the actions of others or to various objects or events. Richard, for example, interpreted arrows on street signs as indicators of the direction he should take. People with delusions of grandeur believe themselves to be great inventors, religious saviors, or other specially empowered persons. And those with delusions of control believe their feelings, thoughts, and actions are being controlled by other people.
formal thought disorder A disturbance in the production and organization of thought.
DISORGANIZED THINKING AND SPEECH People with schizophrenia may not be able to think logically (Briki et al., 2014) and may speak in peculiar ways (Millier et al., 2014). These formal thought disorders can cause the sufferer great confusion and make communication extremely difficult. Often such thought disorders take the form of positive symptoms (pathological excesses), as in loose associations, neologisms, perseveration, and clang.
People who have loose associations, or derailment, the most common formal thought disorder, rapidly shift from one topic to another, believing that their incoherent statements make sense. A single, perhaps unimportant word in one sentence becomes the focus of the next. One man with schizophrenia, asked about his itchy arms, responded:
The problem is insects. My brother used to collect insects. He’s now a man 5 foot 10 inches. You know, 10 is my favorite number. I also like to dance, draw, and watch television.

Some people with schizophrenia use neologisms, made-
HEIGHTENED PERCEPTIONS AND HALLUCINATIONS The perceptions and attention of some people with schizophrenia seem to intensify (Rossi-
hallucination The experiencing of sights, sounds, or other perceptions in the absence of external stimuli.
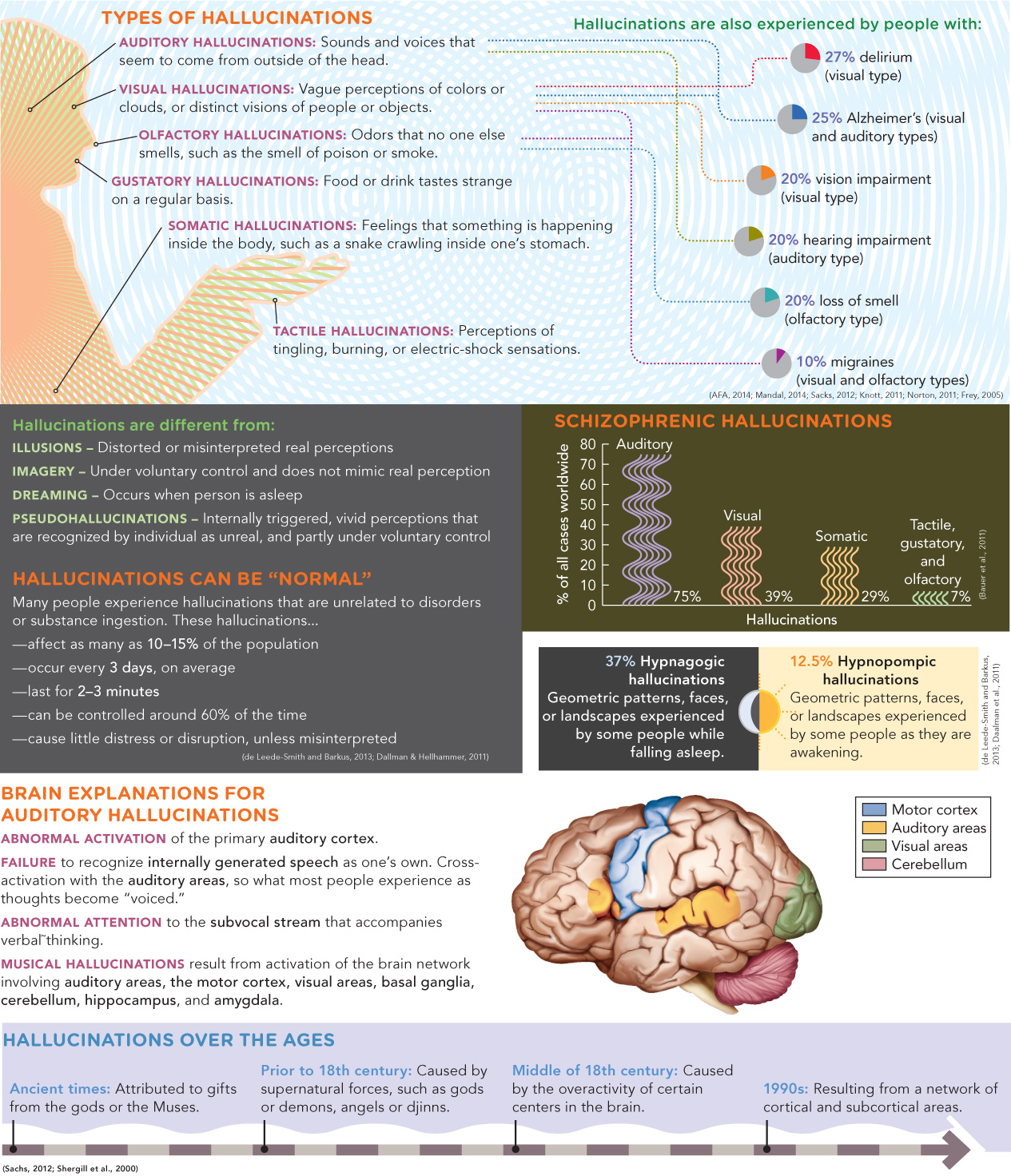
Another kind of perceptual problem in schizophrenia consists of hallucinations, perceptions that a person has in the absence of external stimuli (see InfoCentral below). People who have auditory hallucinations, by far the most common kind in schizophrenia, hear sounds and voices that seem to come from outside their heads. The voices may talk directly to the hallucinator, perhaps giving commands or warning of dangers, or they may be experienced as overheard.
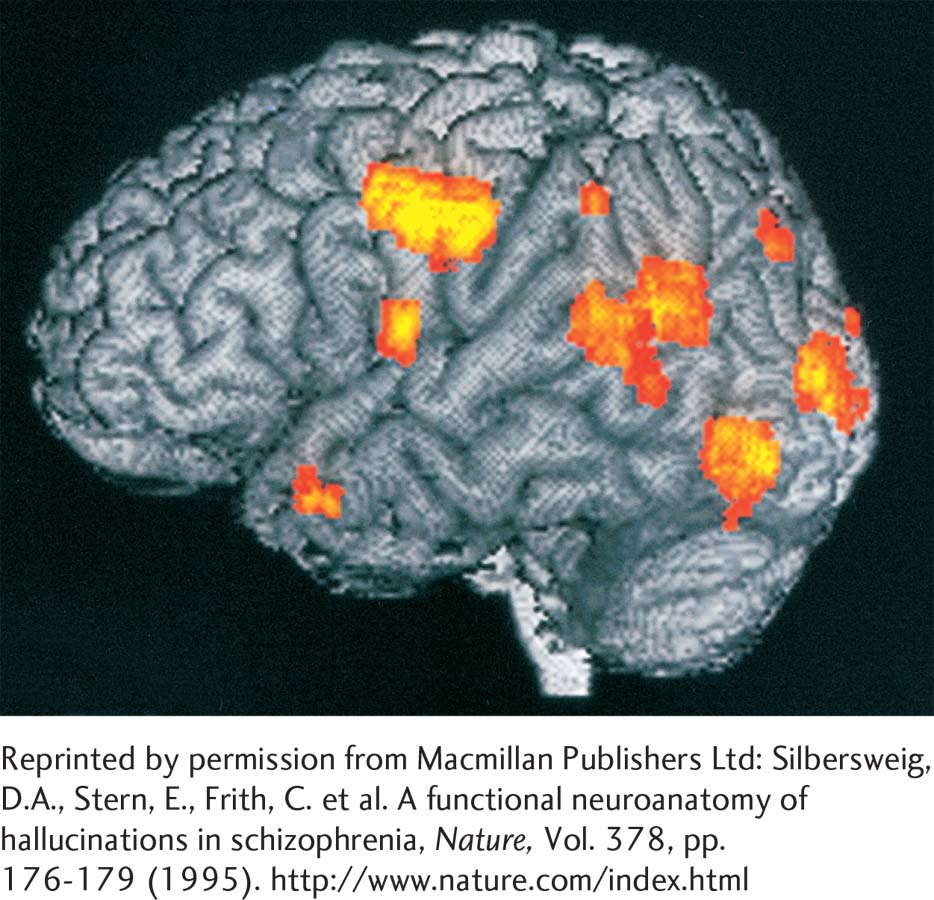
Research suggests that people with auditory hallucinations actually produce the nerve signals of sound in their brains, “hear” them, and then believe that external sources are responsible (Chun et al., 2014; Sarin & Wallin, 2014). One study instructed six men with schizophrenia to press a button whenever they had an auditory hallucination (Silbersweig et al., 1995). PET scans revealed increased activity near the surfaces of their brains, in the tissues of the auditory cortex, the brain’s hearing center, when they pressed the button.
Hallucinations can also involve any of the other senses. Tactile hallucinations may take the form of tingling, burning, or electric-
Hallucinations and delusional ideas often occur together (Cutting, 2015; Shiraishi et al., 2014). A woman who hears voices issuing commands, for example, may have the delusion that the commands are being placed in her head by someone else. Whatever the cause and whichever comes first, the hallucination and delusion eventually feed into each other.
I thought the voices I heard were being transmitted through the walls of my apartment and through the washer and dryer and that these machines were talking and telling me things. I felt that the government agencies had planted transmitters and receivers in my apartment so that I could hear what they were saying and they could hear what I was saying.
(Anonymous, 1996, p. 183)
inappropriate affect Displays of emotions that are unsuited to the situation; a symptom of schizophrenia.
INAPPROPRIATE AFFECT Many people with schizophrenia display inappropriate affect, emotions that are unsuited to the situation (Taylor et al., 2014; Gard et al., 2011). They may smile when making a somber statement or upon being told terrible news, or they may become upset in situations that should make them happy. They may also undergo inappropriate shifts in mood. During a tender conversation with his wife, for example, a man with schizophrenia suddenly started yelling obscenities at her and complaining about her inadequacies.
In at least some cases, these emotions may be merely a response to other features of the disorder. Consider a woman with schizophrenia who smiles when told of her husband’s serious illness. She may not actually be happy about the news; in fact, she may not be understanding or even hearing it. She could, for example, be responding instead to another of the many stimuli flooding her senses, perhaps a joke coming from an auditory hallucination.
InfoCentral
HALLUCINATIONS
Hallucinations are the experiencing of sights, sounds, smells, and other perceptions that occur in the absence of external stimuli.
negative symptoms Symptoms of schizophrenia that seem to be deficits in normal thought, emotions, or behaviors.
Negative Symptoms Negative symptoms are those that seem to be “pathological deficits,” characteristics that are lacking in a person. Poverty of speech, restricted affect, loss of volition, and social withdrawal are commonly found in schizophrenia (Azorin et al., 2014; Rocca et al., 2014). Such deficits greatly affect one’s life and activities.
alogia A decrease in speech or speech content; a symptom of schizophrenia. Also known as poverty of speech.
POVERTY OF SPEECH People with schizophrenia often have alogia, or poverty of speech, a reduction in speech or speech content. Some people with this negative kind of formal thought disorder think and say very little. Others say quite a bit but still manage to convey little meaning (Haas et al., 2014).
RESTRICTED AFFECT Many people with schizophrenia have a blunted affect—they show less anger, sadness, joy, and other feelings than most people (Rocca et al., 2014). And some show almost no emotions at all, a condition known as flat affect. Their faces are still, their eye contact is poor, and their voices are monotonous. In some cases, people with these problems may have anhedonia, a general lack of pleasure or enjoyment. In other cases, however, the restricted affect may reflect an inability to express emotions as others do. One study had participants view very emotional film clips. The participants with schizophrenia showed less facial expression than the others; however, they reported feeling just as much positive and negative emotion and in fact displayed more skin arousal (Kring & Neale, 1996).
LOSS OF VOLITION Many people with schizophrenia experience avolition, or apathy, feeling drained of energy and of interest in normal goals and unable to start or follow through on a course of action (Gard et al., 2014; Gold et al., 2014). This problem is particularly common in people who have had schizophrenia for many years, as if they have been worn down by it. Similarly, people with schizophrenia may feel ambivalence, or conflicting feelings, about most things. The avolition and ambivalence of Richard, the young man you read about earlier, made eating, dressing, and undressing impossible ordeals for him.
SOCIAL WITHDRAWAL People with schizophrenia may withdraw from their social environment and attend only to their own ideas and fantasies (Gard et al., 2014; Pinkham, 2014). Because their ideas are illogical and confused, the withdrawal has the effect of distancing them still further from reality. The social withdrawal seems also to lead to a breakdown of social skills, including the ability to recognize other people’s needs and emotions accurately (Fogley et al., 2014; Lysaker et al., 2014).
catatonia A pattern of extreme psychomotor symptoms, found in some forms of schizophrenia, which may include catatonic stupor, rigidity, or posturing.
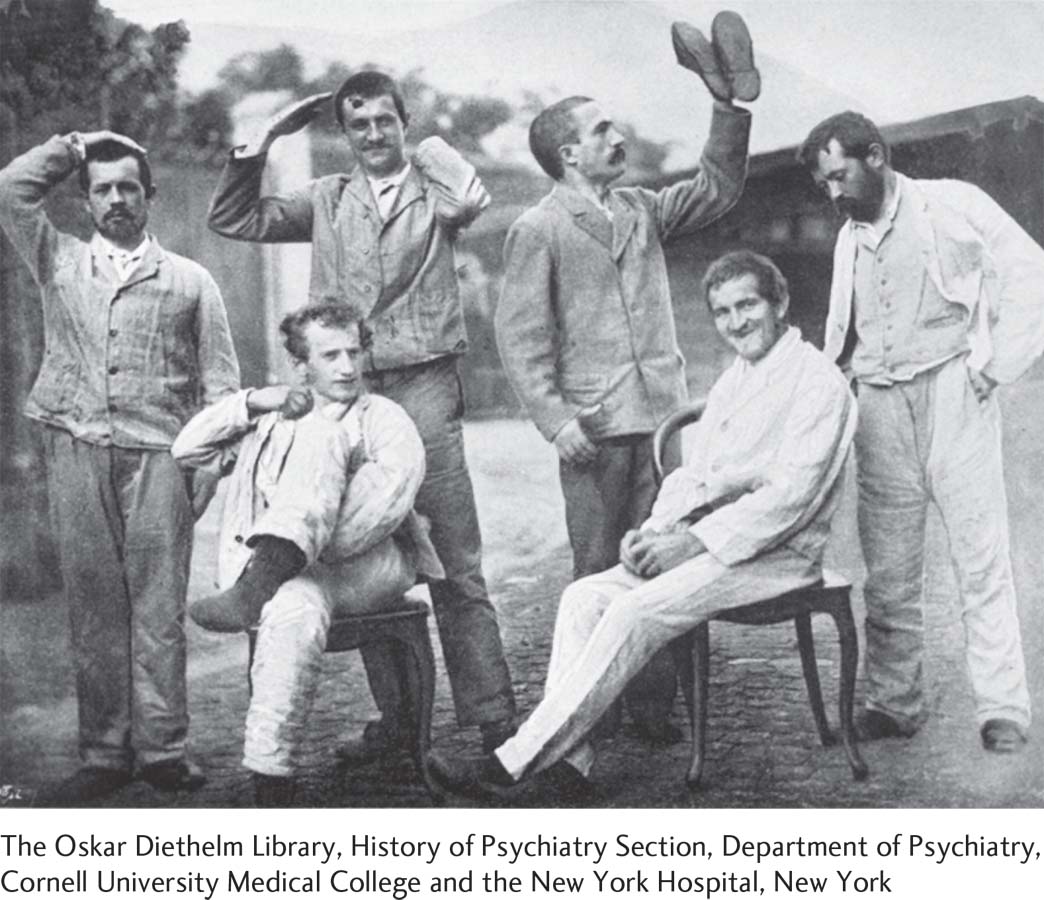
Psychomotor Symptoms People with schizophrenia sometimes experience psychomotor symptoms, for example, awkward movements or repeated grimaces and odd gestures that seem to have a private purpose—
People in a catatonic stupor stop responding to their environment, remaining motionless and silent for long stretches of time. Recall how Richard would lie motionless and mute in bed for days. People with catatonic rigidity maintain a rigid, upright posture for hours and resist efforts to be moved. Still others exhibit catatonic posturing, assuming awkward, bizarre positions for long periods of time. Finally, people with catatonic excitement, a different form of catatonia, move excitedly, sometimes wildly waving their arms and legs.
What Is the Course of Schizophrenia?
Schizophrenia usually first appears between the person’s late teens and mid-
A fuller recovery from schizophrenia is more likely in people who functioned quite well before the disorder; whose disorder is triggered by stress, comes on abruptly, or develops during middle age; and who receive early treatment (Remberk et al., 2015). Relapses are apparently more likely during times of life stress (Bebbington & Kuipers, 2011).
Many researchers believe that in order to help predict the course of schizophrenia, there should be a distinction between so-
Summing Up
THE CLINICAL PICTURE OF SCHIZOPHRENIA Schizophrenia is a disorder in which functioning deteriorates as a result of disturbed thought processes, distorted perceptions, unusual emotions, and motor abnormalities. Approximately 1 percent of the world’s population suffers from this disorder. The symptoms of schizophrenia fall into three groupings. Positive symptoms include delusions, certain formal thought disorders, hallucinations and other disturbances in perception and attention, and inappropriate affect. Negative symptoms include poverty of speech, restricted affect, loss of volition, and social withdrawal. Schizophrenia may also include psychomotor symptoms, collectively called catatonia in their extreme form. Schizophrenia usually emerges during late adolescence or early adulthood and tends to progress through three phases: prodromal, active, and residual.