15.6 Disorders of Cognition
Most of us worry from time to time that we are losing our memory and other mental abilities (Glauberman, 2014). You rush out the door without your keys, you meet a familiar person and cannot remember her name, or you forget that you have seen a particular film. Actually such mishaps are a common and quite normal feature of stress or of aging. As people move through middle age, these memory difficulties and lapses of attention increase, and they may occur regularly by the age of 60 or 70 (see MindTech below). Sometimes, however, people have memory and other cognitive changes that are far more extensive and problematic.
In Chapter 5 you saw that problems in memory and related cognitive processes can occur without biological causes, in the form of dissociative disorders. More often, though, significant cognitive problems do involve biological factors, particularly when they appear late in life. The leading such disorders among the elderly are delirium, major neurocognitive disorder, and mild neurocognitive disorder.
Delirium
delirium A rapidly developing, acute disturbance in attention and orientation that makes it very difficult to concentrate and think in a clear and organized manner.
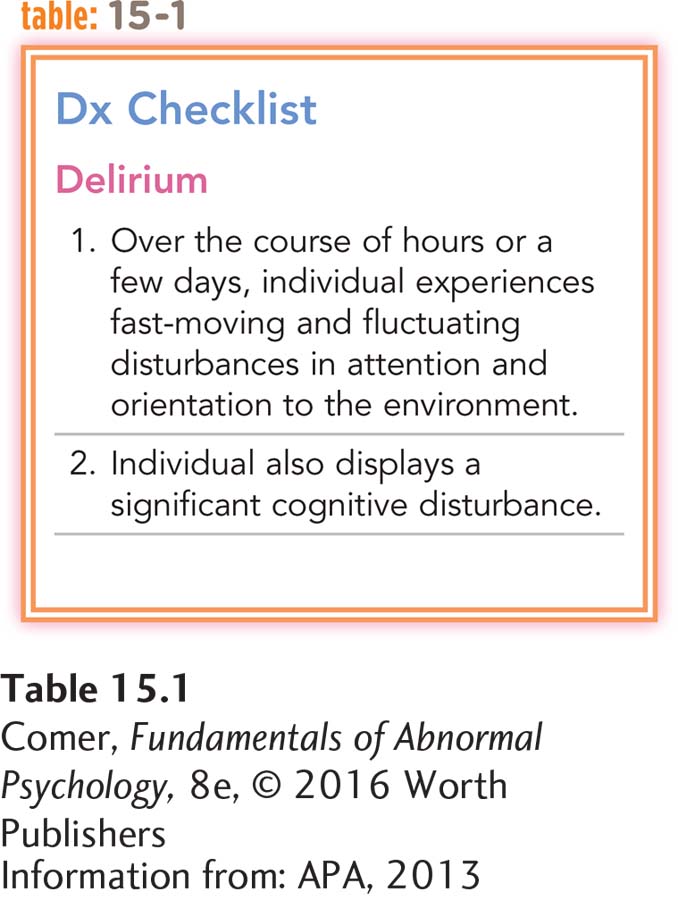
Delirium is a major disturbance in attention and orientation to the environment (see Table 15.1). As the person’s focus becomes less clear, he or she has great difficulty concentrating and thinking in an organized way, leading to misinterpretations, illusions, and, on occasion, hallucinations (Lin et al., 2015). Sufferers may believe that it is morning in the middle of the night or that they are home when actually they are in a hospital room.
This state of massive confusion typically develops over a short period of time, usually hours or days (APA, 2013). Delirium may occur in any age group, including children, but is most common in elderly people. Fewer than 0.5 percent of the nonelderly population experience delirium, compared with 1 percent of people over 55 years of age and 14 percent of those over 85 years of age (Tune & DeWitt, 2011). When elderly people enter a hospital to be treated for a general medical condition, 1 in 10 of them shows the symptoms of delirium. At least another 10 percent develop delirium during their stay in the hospital (Bagnall & Faiz, 2014; Inouye, 2006; Inouye et al., 2003). Around 17 percent of patients admitted for surgery develop delirium (de Castro et al., 2014). Sixty percent of nursing home residents older than 75 years of age have some delirium, compared with 35 percent of similar people living independently with the assistance of home health services (Tune & DeWitt, 2011).
Fever, certain diseases and infections, poor nutrition, head injuries, strokes, and stress (including the trauma of surgery) may all cause delirium (Lawlor & Bush, 2014; Eeles & Bhat, 2010). So may intoxication by certain substances, such as prescription drugs. Partly because older people face so many of these problems, they are more likely than younger ones to experience delirium. If a clinician accurately identifies delirium, it can often be easy to correct—
MindTech
 Remember to Tweet; Tweet to Remember
Remember to Tweet; Tweet to Remember
Social media sites such as Facebook and Twitter, and the Internet in general, are often thought of as the province of the young. However, elderly people are going online and joining social networking sites at increasing rates (Pew Internet, 2014). Some 45 percent of all elderly people online now use Facebook; 9 percent use Pinterest; 5 percent tweet, and 1 percent use Instagram—

Social networking among the elderly is much more than just an interesting statistic; it may be downright therapeutic. Several studies have found that online activity actually helps elderly people maintain and possibly improve their cognitive skills, coping skills, social pleasures, and emotions (Piatt, 2013; Szalavitz, 2013). Clinical theorists have offered several possible explanations for this phenomenon. It may be, for example, that the cognitive stimulation derived from Internet activity activates memory and other cognitive faculties or that the engagement with the world and family provided by the Internet through social networking directly satisfies social and emotional needs. Whatever the reason, more and more studies indicate that elderly people who are wired often function and feel better than those who do not pursue online activities.
One study in Italy, for example, focused on residents from two elder-
In another study, researchers at the University of Arizona recruited 42 adults, ages 68 to 91, and trained 14 of them on Facebook (Piatt, 2013; Wohltmann, 2013). The study found a 25 percent improvement in the cognitive performances of the 14 participants, including improvements in their mental “updating” skills—
Many elderly people resist the Internet and social networking, saying things like “It’s not for me” or “You can’t teach an old dog new tricks.” However, this growing body of research suggests that they may want to embrace social networking and the Internet for better functioning and for better mental health.
Alzheimer’s Disease and Other Neurocognitive Disorders
neurocognitive disorder A disorder marked by a significant decline in at least one area of cognitive functioning.
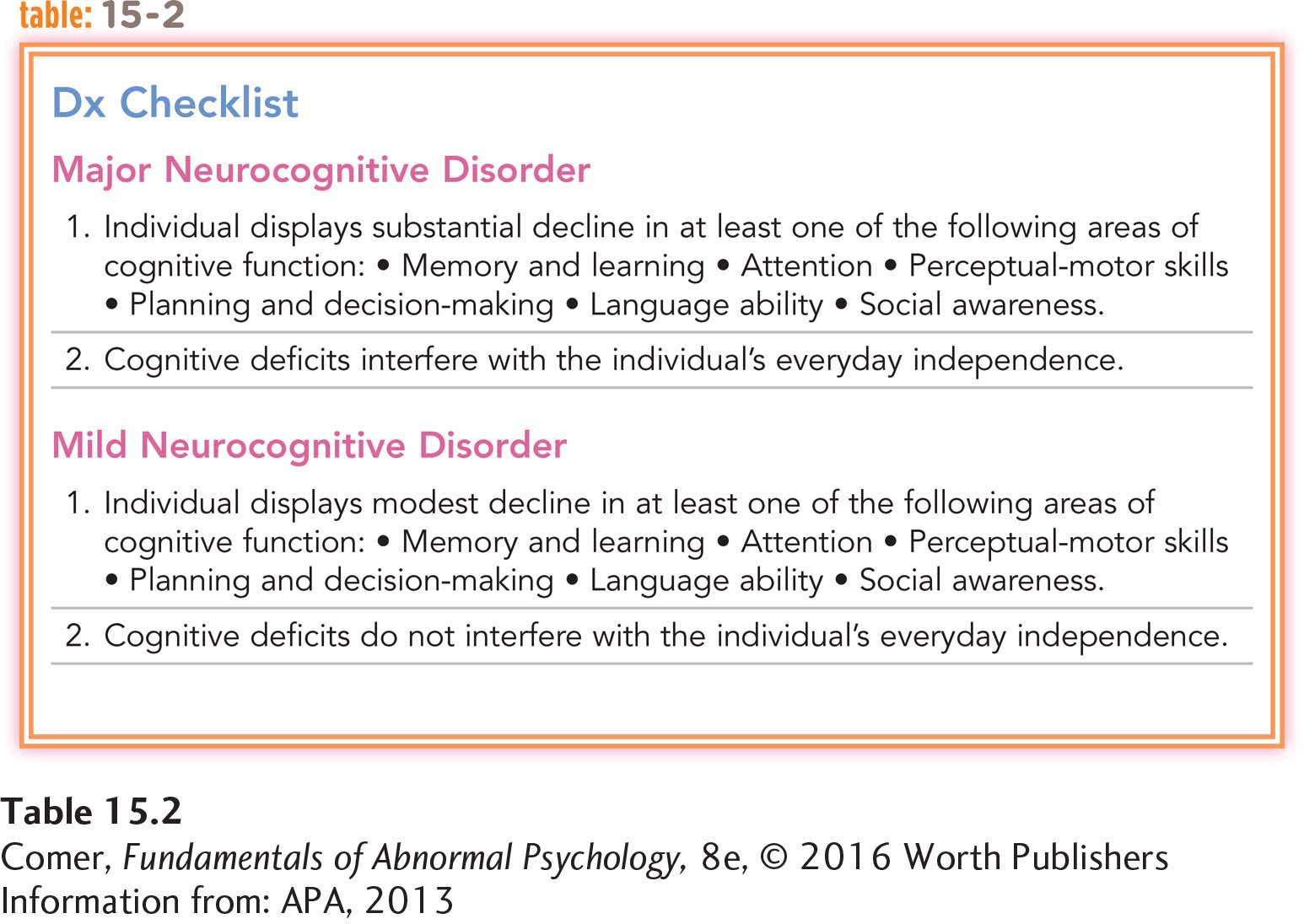
People with a neurocognitive disorder experience a significant decline in at least one (often more than one) area of cognitive functioning, such as memory and learning, attention, visual perception, planning and decision making, language ability, or social awareness (APA, 2013). Those who have certain types of neurocognitive disorders may also undergo personality changes—
major neurocognitive disorder A neurocognitive disorder in which the decline in cognitive functioning is substantial and interferes with a person’s ability to be independent.
mild neurocognitive disorder A neurocognitive disorder in which the decline in cognitive functioning is modest and does not interfere with a person’s ability to be independent.
If the person’s cognitive decline is substantial and interferes significantly with his or her ability to be independent, a diagnosis of major neurocognitive disorder is in order. If the decline is modest and does not interfere with independent functioning, the appropriate diagnosis is mild neurocognitive disorder (see Table 15.2).
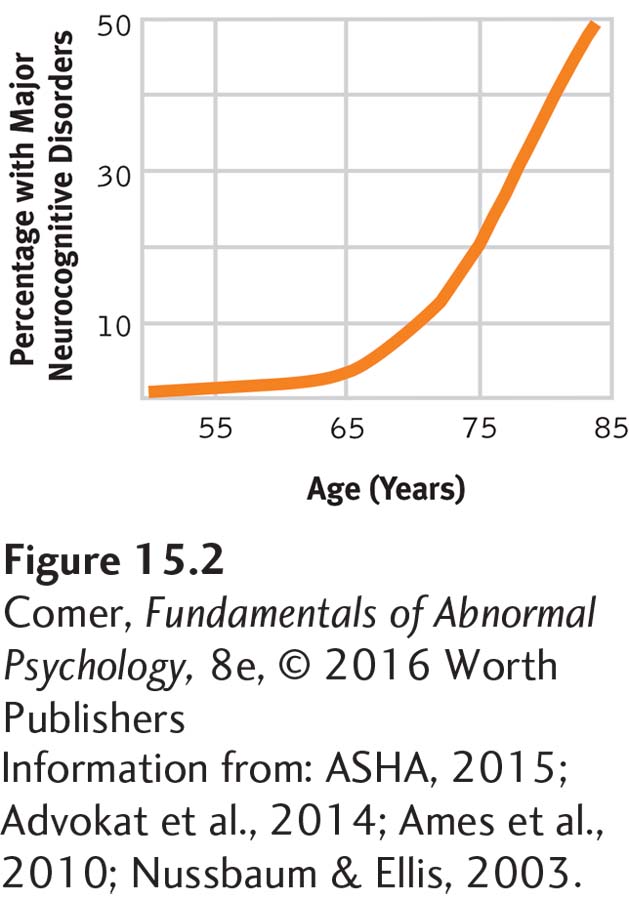
There are currently 44 million people with neurocognitive disorders around the world, with 4.6 million new cases emerging each year (Hollingworth et al., 2011). The number of cases is expected to reach 135 million by 2050 unless a cure is found (Sifferlin, 2013). The occurrence of neurocognitive disorders is closely related to age (see Figure 15.2). Among people 65 years of age, the prevalence is around 1 to 2 percent, increasing to as much as 50 percent among those over the age of 85 (ASHA, 2015; Apostolova & Cummings, 2008).
BETWEEN THE LINES
Universal Concern
In a survey of more than 3,000 adults across the United States, 84 percent of the respondents expressed concern that they or a family member would be affected by Alzheimer’s disease (Shriver, 2014, 2011).
Alzheimer’s disease The most common type of neurocognitive disorder, marked most prominently by memory impairment.
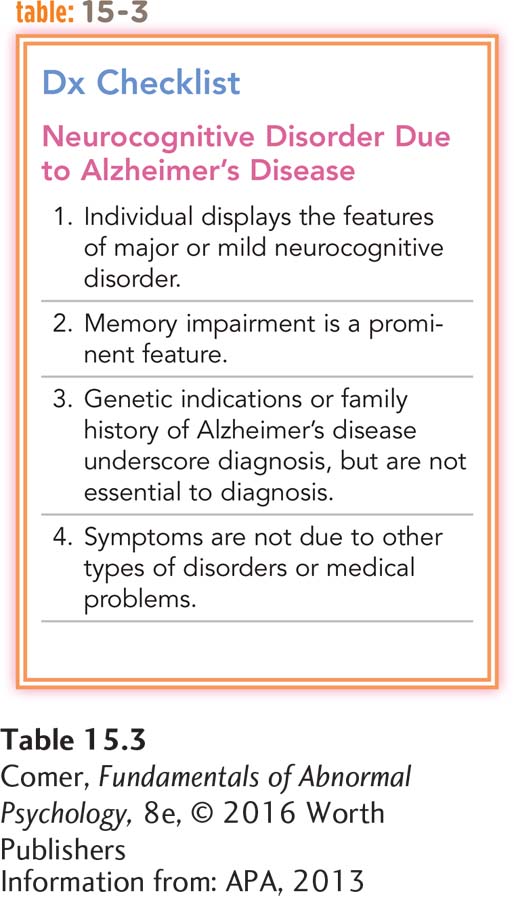
As you read earlier, Alzheimer’s disease is the most common type of neurocognitive disorder, accounting for around two-
Alzheimer’s disease is a gradually progressive disease in which memory impairment is the most prominent cognitive dysfunction (APA, 2013). Technically, sufferers receive a DSM-
Alzheimer’s disease is named after Alois Alzheimer, the German physician who formally identified it in 1907. Alzheimer first became aware of the syndrome in 1901 when a new patient, Auguste D., was placed under his care:
On November 25, 1901, a . . . woman with no personal or family history of mental illness was admitted to a psychiatric hospital in Frankfurt, Germany, by her husband, who could no longer ignore or hide quirks and lapses that had overtaken her in recent months. First, there were unexplainable bursts of anger, and then a strange series of memory problems. She became increasingly unable to locate things in her own home and began to make surprising mistakes in the kitchen. By the time she arrived at Städtische Irrenanstalt, the Frankfurt Hospital for the Mentally Ill and Epileptics, her condition was as severe as it was curious. The attending doctor, senior physician Alois Alzheimer, began the new file with these notes. . . .
She sits on the bed with a helpless expression.
“What is your name?”
Auguste.
“Last name?”
Auguste.
“What is your husband’s name?”
Auguste, I think.
“How long have you been here?”
(She seems to be trying to remember.)
Three weeks.
It was her second day in the hospital. Dr. Alzheimer, a thirty-
He spoke her name again. She wrote “Augu” and again stopped.
When Alzheimer prompted her a third time, she was able to write her entire first name and the initial “D” before finally giving up, telling the doctor, “I have lost myself.”
Her condition did not improve. It became apparent that there was nothing that anyone at this or any other hospital could do for Frau D. except to insure her safety and try to keep her as clean and comfortable as possible for the rest of her days. Over the next four and a half years, she became increasingly disoriented, delusional, and incoherent. She was often hostile.
“Her gestures showed a complete helplessness,” Alzheimer later noted in a published report. “She was disoriented as to time and place. From time to time she would state that she did not understand anything, that she felt confused and totally lost. . . . Often she would scream for hours and hours in a horrible voice.”
By November 1904, three and a half years into her illness, Auguste D. was bedridden, incontinent, and largely immobile. . . . Notes from October 1905 indicate that she had become permanently curled up in a fetal position with her knees drawn up to her chest, muttering but unable to speak, and requiring assistance to be fed.
(Shenk, 2001, pp. 12–
Although some people with Alzheimer’s disease may survive for as many as 20 years, the time between onset and death is typically 8 to 10 years (Advokat et al., 2014; Soukup, 2006). It usually begins with mild memory problems, lapses of attention, and difficulties in language and communication. As symptoms worsen, the person has trouble completing complicated tasks or remembering important appointments. Eventually sufferers also have difficulty with simple tasks, forget distant memories, and have changes in personality that often become very noticeable. For example, a gentle man may become uncharacteristically aggressive.
People with Alzheimer’s disease may at first deny that they have a problem, but they soon become anxious or depressed about their state of mind; many also become agitated. A woman from Virginia describes her memory loss as the disease progresses:
Very often I wander around looking for something which I know is very pertinent, but then after a while I forget about what it is I was looking for. . . . Once the idea is lost, everything is lost and I have nothing to do but wander around trying to figure out what it was that was so important earlier.
(Shenk, 2001, p. 43)
As the neurocognitive symptoms intensify, people with Alzheimer’s disease show less and less awareness of their limitations. They may withdraw from others during the late stages of the disorder, become more confused about time and place, wander, and show very poor judgment. Eventually they become fully dependent on other people. They may lose almost all knowledge of the past and fail to recognize the faces of even close relatives. They also become increasingly uncomfortable at night and take frequent naps during the day (Ferman et al., 2015). During the late phases of the disorder, they require constant care.
People with Alzheimer’s usually remain in fairly good health until the later stages of the disease. As their mental functioning declines, however, they become less active and spend much of their time just sitting or lying in bed. This makes them prone to develop illnesses such as pneumonia, which can result in death (Park et al., 2014). Alzheimer’s disease is currently responsible for close to 84,000 deaths each year in the United States (NCHS, 2014), which makes it the sixth leading cause of death in the country, the third leading cause among the elderly (CDC, 2015).
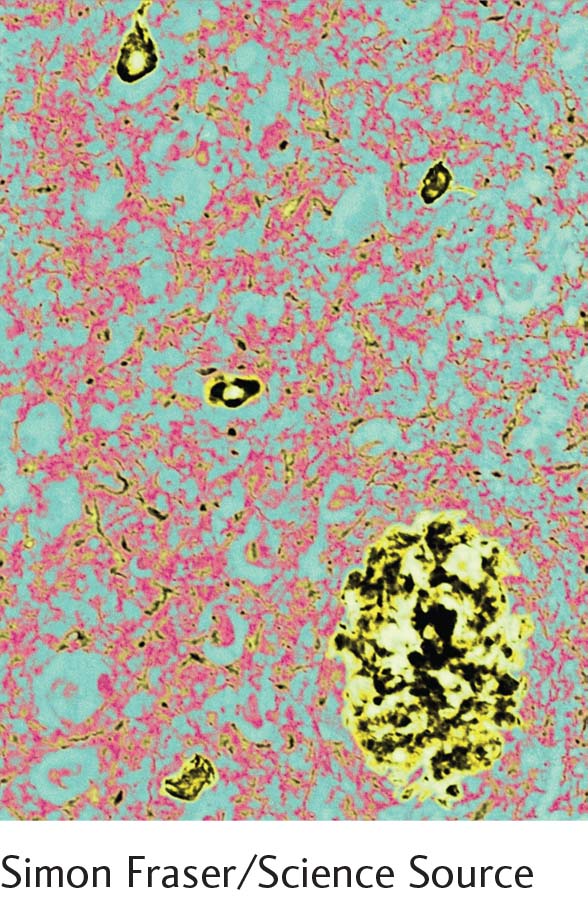
senile plaques Sphere-
neurofibrillary tangles Twisted protein fibers that form within certain brain cells as people age. People with Alzheimer’s disease have an excessive number of such tangles.
In most cases, Alzheimer’s disease can be diagnosed with certainty only after death, when structural changes in the person’s brain, such as excessive senile plaques and neurofibrillary tangles, can be fully examined. Senile plaques are sphere-

Scientists do not fully understand what role excessive numbers of plaques and tangles play in Alzheimer’s disease, but they suspect they are very important. Today’s leading explanations for this disease center on these plaques and tangles and on the various factors that may contribute to their formation.
What Are the Genetic Causes of Alzheimer’s Disease? To understand the genetic theories of Alzheimer’s disease, we must first appreciate the nature and role of proteins. Proteins are fundamental components of all living cells, including, of course, brain cells. They are large molecules made up of chains of carbon, hydrogen, oxygen, nitrogen, and sulfur. There are many different kinds of proteins, each with a different function. Collectively, they are essential for the proper functioning of an organism.
The plaques and tangles that are so plentiful in the brains of Alzheimer’s patients seem to occur when two important proteins start acting in a frenzied manner. Abnormal activity by the beta-
What causes this chain of events? Genetic factors are a major culprit. However, the genetic factors that are responsible differ for the early-
EARLY-
BETWEEN THE LINES
Leading Causes of Death Among the Elderly
| #1 | Heart disease |
| #2 | Cancer |
| #3 | Chronic low respiratory disease |
| #4 | Cerebrovascular disease |
| #5 | Alzheimer’s disease |
(CDC, 2015)
LATE-
A gene called the apolipoprotein E (ApoE) gene is normally responsible for the production of a protein that helps carry various fats into the bloodstream. This gene comes in various forms. About 30 percent of the population inherit the form called ApoE-
Although the ApoE-
BETWEEN THE LINES
DSM-
DSM-
AN ALTERNATIVE GENETIC THEORY OF ALZHEIMER’S DISEASE As you have just read, the leading genetic theories of Alzheimer’s disease point to gene forms, such as ApoE-
How Do Brain Structure and Biochemical Activity Relate to Alzheimer’s Disease? We know that genetic factors may predispose people to Alzheimer’s disease, but we still need to know what abnormalities in brain structure and/or biochemical activity result from such factors and help promote Alzheimer’s disease. Researchers have identified a number of possibilities.
Certain brain structures seem to be especially important in memory. Among the most important structures in short-
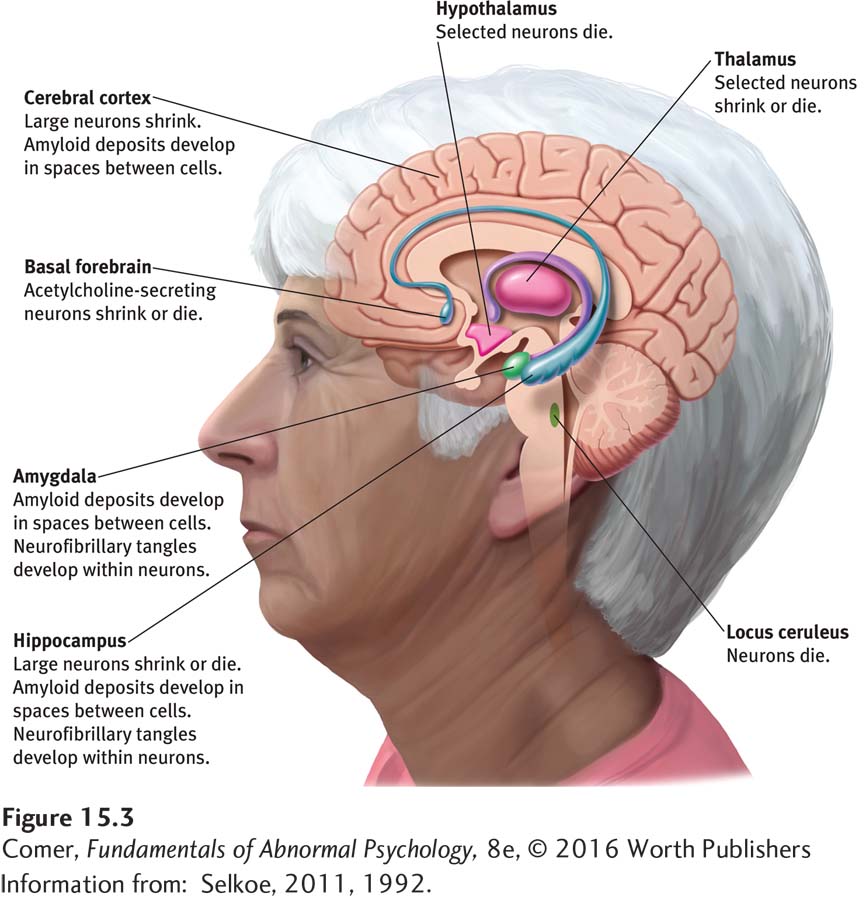
Similarly, certain biochemical activities seem to be especially important in memory. In order for new information to be acquired and stored, certain proteins must be produced in key brain cells. Several chemicals—
Other Explanations of Alzheimer’s Disease Several lines of research suggest that certain substances found in nature may act as toxins, damage the brain, and contribute to the development of Alzheimer’s disease. For example, researchers have detected high levels of zinc in the brains of some Alzheimer’s patients (Xu et al., 2014; Schrag et al., 2011). This finding has gained particular attention because in some animal studies zinc has been observed to trigger a clumping of the beta-
Another line of research suggests that the environmental toxin lead may contribute to the development of Alzheimer’s disease (Lee & Freeman, 2014; Ritter, 2008). Lead was phased out of gasoline products between 1976 and 1991, leading to an 80 percent drop of lead levels in people’s blood. However, many of today’s elderly were exposed to high levels of lead in the 1960s and 1970s, regularly inhaling air pollution from vehicle exhausts—
Two other explanations for Alzheimer’s disease have also been offered. One is the autoimmune theory. On the basis of certain irregularities found in the immune systems of people with Alzheimer’s disease, several researchers have speculated that changes in aging brain cells may trigger an autoimmune response (that is, a mistaken attack by the immune system against itself) that helps lead to the disease (Marchese et al., 2014). The other explanation is a viral theory. Because Alzheimer’s disease resembles Creutzfeldt-
Would people be better off knowing that they will eventually develop a disease that has no known cure?
Assessing and Predicting Alzheimer’s Disease As you read earlier, most cases of Alzheimer’s disease can be diagnosed with absolute certainty only after death, when an autopsy is performed. However, brain scans, which reveal abnormalities in the living brain, now are used commonly as assessment tools and often provide clinicians with considerable confidence in their diagnoses of Alzheimer’s disease (Haris et al., 2015). In addition, several research teams currently are trying to develop tools that can identify those people who are likely to develop Alzheimer’s disease and other types of neurocognitive disorders.
One promising line of work, for example, comes from the laboratory of neuroscientist Lisa Mosconi and her colleagues (Mosconi et al., 2014, 2010, 2008; Mosconi, 2013). Using a special kind of PET scan, this research team examined activity in certain parts of the hippocampus in dozens of elderly research participants and then conducted follow-
BETWEEN THE LINES
Would You Want to Know?
| 78% | Percentage of U.S. adults who would want to have a test done to diagnose a disease even if there were no treatment or cure available |
| 22% | Percentage of U.S. adults who would not want to know |
(Information from: Siemens Healthcare, 2013)
As you will see shortly, the most effective interventions for Alzheimer’s disease and other types of neurocognitive disorders are those that help prevent these problems, or at least ones that are applied early. Clearly, then, it is essential to have tools that identify the disorders as early as possible, preferably years before the onset of symptoms (Rabin, 2013). That is what makes the research advances in assessment and diagnosis so exciting.
Other Types of Neurocognitive Disorders There are a number of neurocognitive disorders in addition to Alzheimer’s disease (APA, 2013). Vascular neurocognitive disorder, for example, follows a cerebrovascular accident, or stroke, during which blood flow to specific areas of the brain was cut off, thus damaging the areas (Jia et al., 2014). In many cases, the patient may not even be aware of the stroke (Moorhouse & Rockwood, 2010). Like Alzheimer’s disease, this disorder is progressive, but its symptoms begin suddenly rather than gradually. Moreover, the person’s cognitive functioning may continue to be normal in areas of the brain that have not been affected by the stroke, in contrast to the broad cognitive deficiencies usually displayed by Alzheimer’s patients. Some people have both Alzheimer’s disease and vascular neurocognitive disorder.
Frontotemporal neurocognitive disorder, also known as Pick’s disease, is a rare disorder that affects the frontal and temporal lobes. It has a clinical picture similar to Alzheimer’s disease, but the two diseases can be distinguished at autopsy.
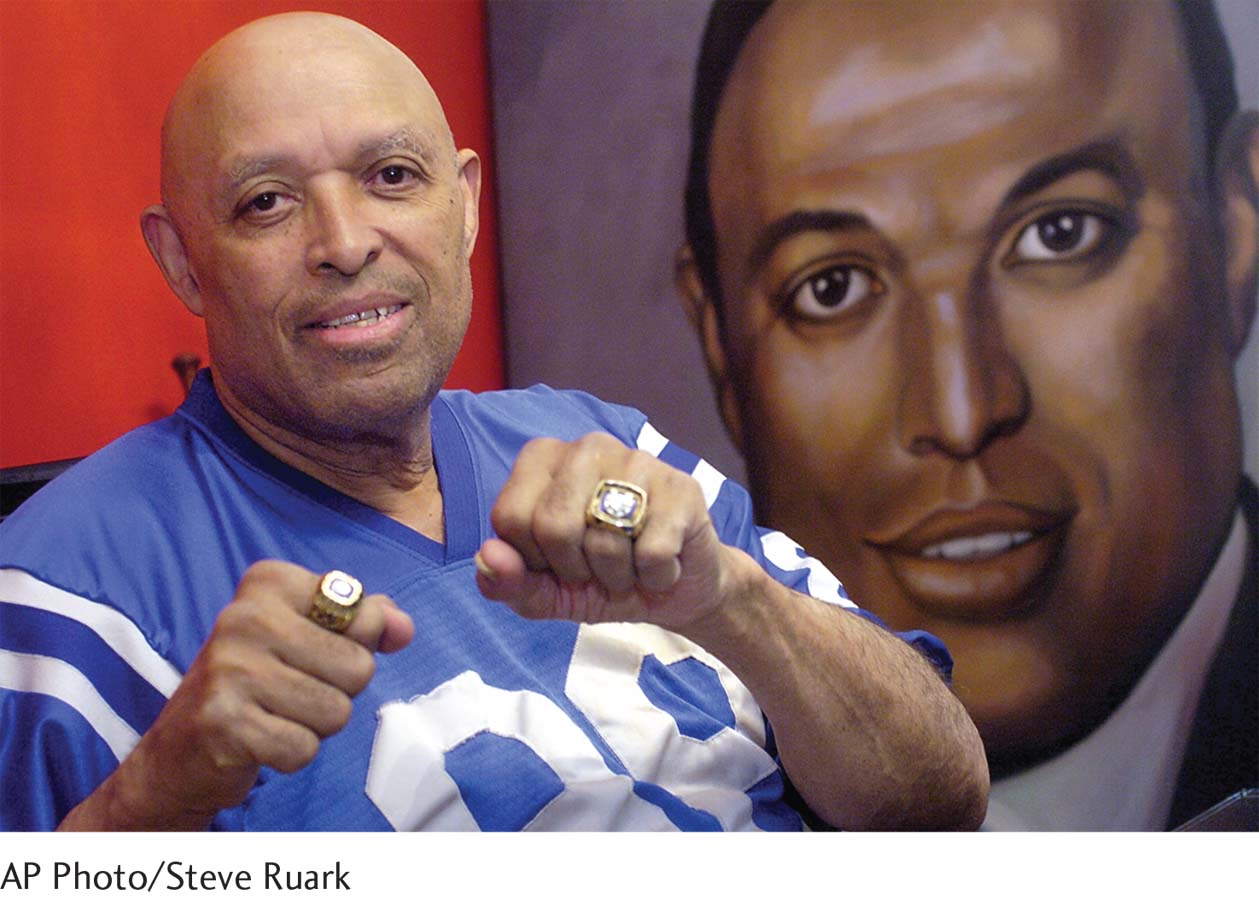
Neurocognitive disorder due to prion disease, also called Creutzfeldt-
Neurocognitive disorder due to Huntington’s disease is an inherited progressive disease in which memory problems, along with personality changes and mood difficulties, worsen over time. People with Huntington’s have movement problems, too, such as severe twitching and spasms. Children of people with Huntington’s disease have a 50 percent chance of developing it.
Parkinson’s disease, the slowly progressive neurological disorder marked by tremors, rigidity, and unsteadiness, can result in neurocognitive disorder due to Parkinson’s disease, particularly in older people or those whose cases are advanced.
Yet other neurocognitive disorders may be caused by HIV infections, traumatic brain injury, substance abuse, or various medical conditions such as meningitis or advanced syphilis.
What Treatments Are Currently Available for Alzheimer’s Disease and Other Neurocognitive Disorders? Treatments for the cognitive features of Alzheimer’s disease and most other types of neurocognitive disorders have been at best modestly helpful. A number of approaches have been applied, including drug therapy, cognitive techniques, behavioral interventions, support for caregivers, and sociocultural approaches.
DRUG TREATMENT The drugs currently prescribed for Alzheimer’s patients are designed to affect acetylcholine and glutamate, the neurotransmitters that play important roles in memory. Such drugs include donepezil (Aricept), rivastigmine (Exelon), galantamine (Razadyne), and memantine (Namenda). The short-
The drugs just discussed are each prescribed after a person has developed Alzheimer’s disease. In contrast, studies suggest that certain substances now available on the marketplace for other kinds of problems may help prevent or delay the onset of Alzheimer’s disease. For example, some studies have found that women who took estrogen, the female sex hormone, for years after menopause cut their risk of developing Alzheimer’s disease in half (Li et al., 2014; Kawas et al., 1997). Other studies have suggested that the long-
BETWEEN THE LINES
Busy Mind, Healthier Brain
Researchers have found fewer plaques and tangles in the brains of lab mice that live in intellectually and physically stimulating environments—
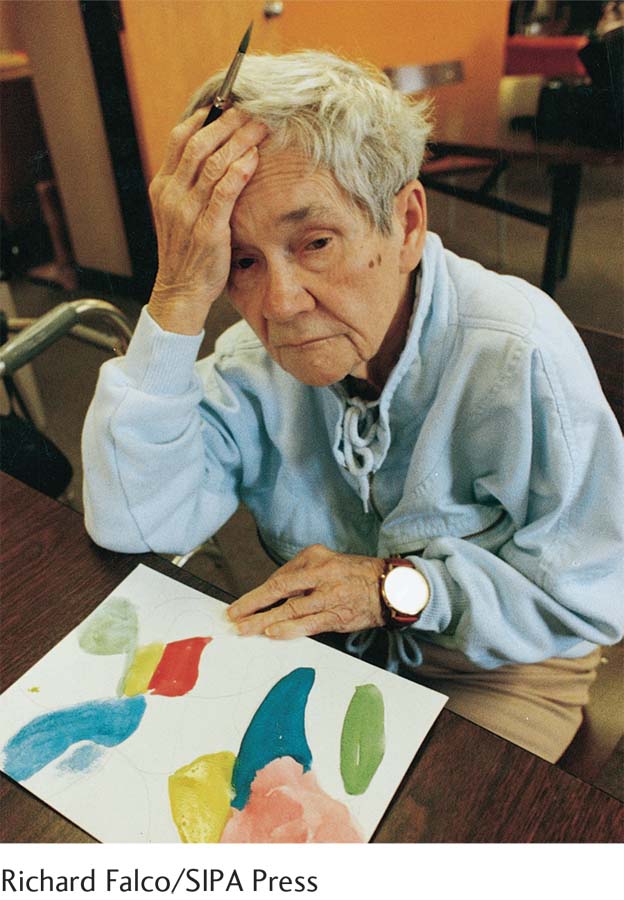
COGNITIVE TECHNIQUES Cognitive treatments have been used in cases of Alzheimer’s disease, with some temporary success (Nelson & Tabet, 2015). In Japan, for example, a number of people with the disease meet regularly in classes, performing simple calculations and reading essays and novels aloud. Proponents of this approach claim that it serves as a mental exercise that helps rehabilitate those parts of the brain linked to memory, reasoning, and judgment. Similarly, some research suggests that cognitive activities, including computer-

BEHAVIORAL INTERVENTIONS Behavioral interventions have also been somewhat successful in helping Alzheimer’s patients. It has become increasingly clear across many studies that physical exercise helps improve cognitive functioning—
Behavioral interventions of a different kind have been used to help improve specific symptoms displayed by Alzheimer’s patients. The approaches typically focus on changing everyday patient behaviors that are stressful for the family, such as wandering at night, loss of bladder control, demands for attention, and inadequate personal care (Lancioni et al., 2011; Lindsey, 2011). The behavioral therapists use a combination of role-
SUPPORT FOR CAREGIVERS Caregiving can take a heavy toll on the close relatives of people with Alzheimer’s disease and other types of neurocognitive disorders (Kang et al., 2014). Almost 90 percent of all people with Alzheimer’s disease are cared for by their relatives (Alzheimer’s Association, 2014, 2007). It is hard to take care of someone who is becoming increasingly lost, helpless, and medically ill. And it is very painful to witness mental and physical decline in someone you love.

One of the most frequent reasons for the institutionalization of people with Alzheimer’s disease is that overwhelmed caregivers can no longer cope with the difficulties of keeping them at home (Di Rosa et al., 2011; Apostolova & Cummings, 2008). Many caregivers experience anger and depression, and their own physical and mental health often declines (Kang et al., 2014). Clinicians now recognize that one of the most important aspects of treating Alzheimer’s disease and other types of neurocognitive disorders is to focus on the emotional needs of the caregivers, including their needs for regular time out, education about the disease, and psychotherapy (Mittelman & Bartels, 2014). Some clinicians also provide caregiver support groups.

SOCIOCULTURAL APPROACHES Sociocultural approaches play an important role in treatment (Fouassier et al., 2015; Pongan et al., 2012) (see MediaSpeak below). A number of day-
Given the progress now unfolding in the understanding and treatment of Alzheimer’s disease and other types of neurocognitive disorders, researchers are looking forward to important advances in the coming years. The brain changes responsible for these disorders are tremendously complex, but most investigators believe that exciting breakthroughs are just over the horizon.

MediaSpeak
Focusing on Emotions
By Pam Belluck, New York Times, January 1, 2011

Margaret Nance was, to put it mildly, a difficult case. Agitated, combative, often reluctant to eat, she would hit staff members and fellow residents at nursing homes, several of which kicked her out. But when Beatitudes nursing home agreed to an urgent plea to accept her, all that changed.
Disregarding typical nursing-
And she was given a baby doll, a move that seemed so jarring that a supervisor initially objected until she saw how calm Ms. Nance became when she rocked, caressed and fed her “baby,” often agreeing to eat herself after the doll “ate” several spoonfuls.
Dementia patients at Beatitudes are allowed practically anything that brings comfort, even an alcoholic “nip at night,” said Tena Alonzo, director of research. “Whatever your vice is, we’re your folks,” she said. . . .
It is an unusual posture for a nursing home, but Beatitudes is actually following some of the latest science. Research suggests that creating positive emotional experiences for Alzheimer’s patients diminishes distress and behavior problems. . . . [Some studies also] recommend making cosmetic changes to rooms and buildings to affect behavior or mood. [One such study] found that brightening lights in dementia facilities decreased depression, cognitive deterioration and loss of functional abilities. . . .
If Alzheimer’s disease is a biologically caused disorder, why would increasing patients’ comfort levels make such a difference?
One program for dementia patients cared for by relatives at home creates specific activities related to something they once enjoyed: arranging flowers, filling photo albums, snapping beans.
“A gentleman who loved fishing could still set up a tackle box, so we gave him a plastic tackle box” to set up every day, said the program’s developer, Laura N. Gitlin, a sociologist . . . at Johns Hopkins University. . . .
Beatitudes, which takes about 30 moderate to severe dementia sufferers, introduced its program 12 years ago, focusing on individualized care. . . . Beatitudes eliminated anything potentially considered restraining, from deep-
It encouraged keeping residents out of diapers if possible, taking them to the toilet to preserve feelings of independence. . . . Beatitudes also changed activity programming, [instructing] staff members [to] conduct one-
These days, hundreds of Arizona physicians, medical students, and staff members at other nursing homes have received Beatitudes’ training, and several Illinois nursing homes are adopting it. . . .
January 01, 2011, “The Vanishing Mind: Giving Alzheimers Patients Their Way, Even Doses of Chocolate” by Pam Belluck. From New York Times 1/1/2011, © 2011 The New York Times. All rights reserved. Used by permission and protected by the copyright laws of the United States. The printing, copying, redistribution, or retransmission of this content without express written permission is prohibited.
BETWEEN THE LINES
Maximum Age
The maximum attainable age by human beings is thought to be 122 years (Basaraba, 2014; Durso et al., 2010).
Summing Up
DISORDERS OF COGNITION Older people are more likely than people of other age groups to experience delirium, a fast-
Neurocognitive disorders, characterized by a significant decline in cognitive function, become increasingly common in older age groups. There are many types of neurocognitive disorders, the most common being Alzheimer’s disease. Alzheimer’s disease has been linked to an unusually high number of senile plaques and neurofibrillary tangles in the brain. According to a leading explanation of late-
A number of other causes have also been proposed for this disease, including high levels of zinc, lead, or other toxins; immune system problems; and a virus of some kind.
Researchers are making significant strides at better assessing Alzheimer’s disease and other types of neurocognitive disorders and even at identifying those who will eventually develop these disorders. Drug, cognitive, and behavioral therapies have been used to treat Alzheimer’s disease, with limited success. Addressing the needs of caregivers is now also recognized as a key part of treatment. In addition, sociocultural approaches such as day-