Preparing to Die
Slide 1 of 16: Synopsis
Author
Catherine Robertson, Grossmont College
Michelle Ryder, Daniel Webster College
Synopsis
This activity explores the process of dying: how different age groups perceive dying, the kinds of care that are available to terminally-ill patients, and the types of support that are necessary and helpful to patients facing their own deaths. People with terminal illnesses go through a process that allows them to prepare for their deaths and to come to terms with the inevitability of their own passing. In video clips, patients share their personal experiences, and experts discuss how the process of dying has changed over time for both patients with terminal illnesses and those who care for them.
References
Berger, K. (2001). The developing person through the life span. New York, NY: Worth Publishers.
Byrock, I. (2002). The meaning and value of death. Journal of Palliative Care, 5(2), 279-288.
Caring Connections: Caring for Someone: Caring for a Child with a Serious Illness. Retrieved from: http://www.caringinfo.org/CaringForSomeone.htm
deVries, B., Bluck, S., & Birren, J. (1993). The understanding of death and dying in a life-span perspective. Gerontologist, 33(3), 366-372.
Kastenbaum, R. (1996). A world without death: First and second thoughts. Mortality, 123(1), 113-123.
Kessler, D. (2000). The needs of the dying: A guide for bringing hope, comfort and love to life’s final chapter. New York, NY: HarperCollins.
Kübler-Ross, E. (1969). On death and dying. New York: Macmillan.
Kübler-Ross, E. (1975). Death: The final stage of growth. Englewood Cliffs, NJ: Prentice Hall.
Lynn, J., & Harrold, J. (2001). Handbook for mortals: Guidance for people facing serious illness. Oxford: Oxford University Press.
Nuland, S. (1995). How we die: Reflections on life’s final chapter. New York: Vintage Press.
Slide 2 of 16: Death and Dying
- Chapters
- descriptions off, selected
- captions settings, opens captions settings dialog
- captions off, selected
- English Captions
This is a modal window.
Beginning of dialog window. Escape will cancel and close the window.
End of dialog window.
This is a modal window. This modal can be closed by pressing the Escape key or activating the close button.
This is a modal window.
Death is a subject that most dislike talking about or even thinking about. Unfortunately, part of life is dealing with death. Inevitably, death invades our lives whether through a sudden death or a terminal illness of someone whom we know.
According to Dr. Kübler-Ross (1969, 1975), a person diagnosed with a terminal illness is likely to go through several stages of emotion when accepting that death will be the final outcome of the illness. Kübler-Ross’s stages of grief occur in the following order: denial, anger, bargaining, depression, and acceptance. While other researchers do not agree exactly with Dr. Kübler-Ross’s findings, most Western researchers do believe that honest, compassionate communication with those who are facing death is important.
In this video, Lucky Star, whose face is blurred to protect her identity, and Dorothy Smith, an older adult, discuss their experiences in confronting their terminal illnesses.
Slide 3 of 16: A Life Span Perspective to Dying: Childhood to Young Adulthood
- Chapters
- descriptions off, selected
- captions settings, opens captions settings dialog
- captions off, selected
- English Captions
This is a modal window.
Beginning of dialog window. Escape will cancel and close the window.
End of dialog window.
This is a modal window. This modal can be closed by pressing the Escape key or activating the close button.
This is a modal window.
As noted in Berger (2001), the age at which a person discovers that he/she is dying has a great effect on how he/she reacts to death. Most young children do not yet understand the concept of death. They may react to their own dying with fear at being separated from loved ones and anger at their disease.
A teenager’s sense of immortality derives from adolescent egocentrism and the concept of the invincibility fable. When an adolescent comes to terms with the fact that he/she is dying, how the process of death will affect his/her social relationships with peers and his/her physical appearance may become of primary importance.
Young adults are very likely to feel depressed and angry at the prospect of dying. They are at a point in their young lives when they are just beginning to access the rights and privileges of adulthood.
In this video, twenty-year-old Laura has cystic fibrosis and speaks about her experience of living with a terminal illness. Even though her illness seems to have made her wise well beyond her years, you may still hear glimpses of her youthful life stage.
Slide 4 of 16: A Life Span Perspective to Dying: Middle to Late Adulthood

Someone in middle adulthood is generally at the point of greatest responsibility in his/her life in terms of family and career. This sense of responsibility may lead someone in middle adulthood to a flurry of preparations for those loved ones and fellow workers to be left behind with his/her death.
Chances are that someone in late adulthood has participated in a life review at some level. If this older adult has not already begun a life review, the diagnosis of a terminal illness certainly becomes the impetus to do so. The more loss of loved ones, such as spouses, brothers, sisters, and friends, that this person in late adulthood has experienced, the more likely he/she will be able to reach acceptance of death without too much difficulty.
Slide 5 of 16: The Changing Experience of Death
- Chapters
- descriptions off, selected
- captions settings, opens captions settings dialog
- captions off, selected
- English Captions
This is a modal window.
Beginning of dialog window. Escape will cancel and close the window.
End of dialog window.
This is a modal window. This modal can be closed by pressing the Escape key or activating the close button.
This is a modal window.
Until fairly recently, doctors often did not tell patients or their families that death was the prognosis. If, by some chance, the family members figured out that their loved one was not going to get better, they were reluctant to even tell him/her. This protecting of the terminal patient from death ended up preventing the dying person from giving or receiving comfort from loved ones, making final preparations and arrangements, or making amends in attempt to heal broken relationships. Since death was not spoken of in front of the dying patient, families were also deprived of saying goodbye and expressing their love and appreciation. This silencing of all talk of death is sometimes referred to as a bad death.
The overall result was that the dying person and his/her family were robbed of the dignity that death should have had. Kübler-Ross and other researchers worked very hard to transform dying from an institutional, impersonal, polite process to a personal, comfortable, and openly emotional process for the patient and the family. This effort included the organization and introduction of the idea of hospice. Today, there are hospices and in-home hospice care options throughout the United States.
In this video, policy expert, Barbara Coombs-Lee, discusses the experience of dying in the United States from a historical perspective.
Slide 6 of 16: A Good Death
A good death is one in which a patient is informed of his/her impending death and has his/her needs met in this important journey. The fact that dying is actually occurring must be recognized. Every dying person must accept the impending loss of life as it has been known, which includes the letting go of everyone and everything that the person has known and/or loved. This is a tremendous task for the dying person to undertake alone. Kessler (2000) has identified the needs of a dying person as:
- the need to be treated as a human being;
- the need for hope;
- the need to express emotions;
- the need to participate in his/her own care;
- the need for honesty;
- the need for spirituality;
- the need to be free of pain.
In a good death, all of these needs are addressed. Additionally, it is important for both the patient and the family to recognize the healing power of going through the stages of grief. Progressing through the stages of grief helps the patient to achieve a semblance of peace while facing the process of dying.
Slide 7 of 16: Decisions that Surround Dying: Palliative Care
- Chapters
- descriptions off, selected
- captions settings, opens captions settings dialog
- captions off, selected
- English Captions
This is a modal window.
Beginning of dialog window. Escape will cancel and close the window.
End of dialog window.
This is a modal window. This modal can be closed by pressing the Escape key or activating the close button.
This is a modal window.
When one is faced with death, a number of decisions must be made. While denial, anger, and bargaining may be long past or even revisited upon occasion, a decision as to when to trade in care that strives to find a cure for palliative care needs to be made. A circle of family and medical personnel is normally involved in the decision of whether or not or when to shift focus to palliative care. The dying patient’s voice, which may be very much influenced by where he/she is in the life span, is vital to this decision. The crucial decisions do not stop with whether or not to progress to palliative care. More important arrangements will need to be considered during the dying process.
In this video, Dr. Jeffrey Birnbaum speaks about the importance of palliative care for patients who are dying.
Slide 8 of 16: Decisions that Surround Dying: Hospice Care
- Chapters
- descriptions off, selected
- captions settings, opens captions settings dialog
- captions off, selected
- English Captions
This is a modal window.
Beginning of dialog window. Escape will cancel and close the window.
End of dialog window.
This is a modal window. This modal can be closed by pressing the Escape key or activating the close button.
This is a modal window.
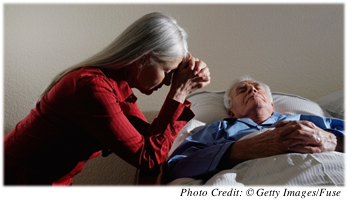
Watch this video of Dorothy, a terminally ill patient and former nursing educator, discussing her decision about hospice care.
Another important decision is to figure out where a terminal patient will die. Today, people are fortunate enough to be generally able to choose where they will die. It is no longer a given that death will occur in a hospital. Hospice agencies abound in the United States. Some hospice agencies deal with providing care and respite at home. This includes providing the proper equipment that a dying person would need in order to be comfortable, such as a hospital bed, a portable toilet, and perhaps a wheelchair or walker. Some hospice agencies offer a place for a person to go and die as well. The decision as to whether or not to involve hospice must be thoroughly discussed by the patient and his/her family, preferably while the patient is still well enough to make sound decisions.
Slide 9 of 16: Decisions that Surround Dying: A Living Will

Death is more complex today than it was in the past because of many medical breakthroughs. Modern medicine has the ability to stave off death with medication, treatments, and machines that keep the body functioning long after it might have quit on its own. A living will can help if a person loses the ability to communicate his/her own wishes. With this kind of will, a person directs what medical interventions should or should not be taken during a medical crisis or the dying process. This decision needs to be made as soon as possible after a person acknowledges that death is impending. By preparing a living will, family and friends are freed from making a difficult choice on behalf of the patient.
Slide 10 of 16: A Controversial Decision: The Right to Die
Some terminally-ill patients would like the ability to choose to end life before the pain and degradation of a disease eradicate all his/her dignity. This choice is often referred to as the patient’s right to die. Patients who believe in their right to die might consider a physician-assisted suicide or voluntary euthanasia. Both of these practices are very controversial and illegal in most of the world except in the state of Oregon in the United States and the nation of the Netherlands in Europe. Although these actions are illegal, these practices are rarely discovered. Unless the death is a public or blatant act, it is usually not subject to prosecution.
Slide 11 of 16: Sharing the Journey

Once death is acknowledged, it is important for the person who is dying to not feel alone in the journey. It is beneficial to the patient, the family, and loved ones to share the journey so that there is as broad a support network as possible for all involved.
Family members and loved ones can help the patient organize and update important papers, such as a will. It is much easier for those left behind if they know the specific requests of the dying person. Active involvement of both the dying individual and his/her loved ones in the preparation of a memorial or funeral service allows for all to be able to communicate and share emotions, ideas, and fond memories.
Whether the emotions and memories are happy or sad, they need to be acknowledged on both sides. If a relationship needs forgiveness and healing, this is the time to do it. This is also the time for exploring one’s own spirituality and any feelings about dying. Embracing one’s spirituality may provide varying levels of comfort when facing one’s own death and can help the patient to move toward acceptance.
Slide 12 of 16: Summary

Most of us do not like to think about or even discuss death. The reality is that death is part of life, and it should be treated as such. People who have terminal illnesses and know that they are dying benefit from a good death in which their physical and emotional needs are met. If they are able to say goodbye, make final business and funeral arrangements, and heal relationships, death may be more comfortable and bearable. Making decisions about the dying process should involve both the dying person and his/her family in effort to make the impending death easier on everyone. Sharing the dying experience with loved ones can make the transition seem much more peaceful and manageable for both the person who is dying and those who will be left behind.
Slide 13 of 16: Assessment: Check Your Understanding
Slide 14 of 16: Assessment: Check Your Understanding
Slide 15 of 16: Assessment: Check Your Understanding
Slide 16 of 16: Assessment: Check Your Understanding

Congratulations! You have completed this activity.Total Score: x out of x points (x%) You have received a provisional score for your essay answers, which have been submitted to your instructor.