Hunger and Eating
Not one man in a billion, when taking his dinner, ever thinks of utility. He eats because the food tastes good and makes him want more.
—William James
Principles of Psychology (1890)
KEY THEME
Hunger is a biological motive, but eating behavior is motivated by a complex interaction of biological, social, and psychological factors.
KEY QUESTIONS
What is energy homeostasis, and how is food converted to energy?
What are the short-
term signals that regulate eating behavior? What chemical signals are involved in the long-
term regulation of a stable body weight? What factors contribute to long-
term weight gain?
It seems simple: You’re hungry, so you eat. But even a moment’s reflection will tell you that eating behavior is not that straightforward. When, what, how much, and how often you eat is influenced by an array of psychological, biological, social, and cultural factors.
For example, think about what you ate yesterday. Now contrast your choices with food preferences in other cultures. A typical diet for the Dusan of northern Borneo in Southeast Asia includes anteater, gibbon (a small ape), snake, mouse, and rat meat. After these meats have spoiled to the point of being liquefied, the Dusan consume them with rice. South American Indians eat head lice, bees, iguanas, and monkeys. The Guianese of South America eat pebbles as a regular part of their diet, while the Vedda of Sri Lanka like rotted wood (see Fieldhouse, 1986). In Nepal, the trekkers were often offered Tibetan butter tea, a thick brew of strong tea, salt, yak butter, and yak milk. Clearly, cultural experience shapes our food choices (Rozin, 2006, 2007).

In the next several sections, we look at what researchers have learned about the factors that trigger hunger and motivate eating behavior.
Energy Homeostasis
CALORIES CONSUMED = CALORIES EXPENDED
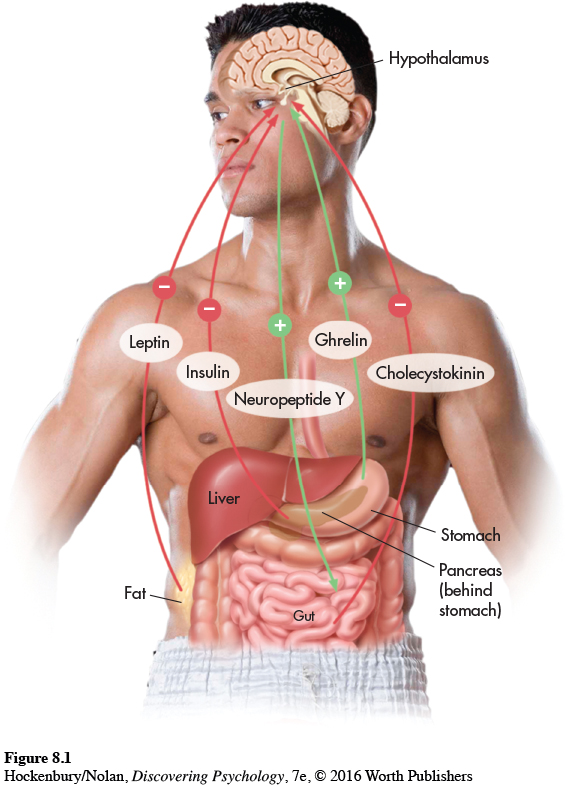
How is food converted to energy in the body? The food that you eat is broken down by enzymes, gradually absorbed in your intestines, and converted into amino acids, fatty acids, and simple sugars. The simple sugar glucose provides the main source of energy for all mammals, including humans. The hormone insulin, secreted by the pancreas, helps control blood levels of glucose and promotes the uptake of glucose by the muscles and other body tissues. Insulin also helps in regulating eating behavior and maintaining a stable body weight.
About one-
Often, there is considerable daily variation in what, when, how often, and how much we eat. Yet despite this variability in eating behavior, our body weight tends to stay relatively constant (Bessesen, 2011). Your typical or average body weight is called your baseline body weight, which is maintained by a process called energy homeostasis.
But what if you eat more—
Short-Term Signals That Regulate Eating
Why do we eat? About 30 minutes before you eat, you experience a slight increase in blood levels of insulin and a slight decrease in blood levels of glucose. In experimental studies with both humans and rats, these small changes reliably predict the initiation of eating (Chaput & Tremblay, 2009). Once the meal is begun, blood glucose levels return to their baseline level. Interestingly, glucose returns to its baseline level well before the food is actually digested and absorbed.
A more important internal signal is ghrelin, a hormone manufactured by cells lining the stomach (Kojima, 2011; Olszweski & others, 2008). Ghrelin was dubbed “the hunger hormone” when research showed that it strongly stimulates appetite. Blood levels of ghrelin rise sharply before and fall abruptly after meals (Cummings, 2006; Cummings & others, 2002). It also seems to be involved in the long-
Eating is also triggered by psychological factors. Both classical conditioning and operant conditioning, described in Chapter 5, affect eating behavior. For example, in much the same way as Pavlov’s dogs were conditioned to salivate at the sound of a bell, your feelings of hunger have probably been classically conditioned by years of experience. Time of day or other stimuli, such as the setting in which you normally eat or just the sight of food utensils, can become associated with the anticipation of eating and trigger the physiological signals that increase your sense of hunger (Davidson, 2000).
Operant conditioning and positive reinforcement play a role in eating, too. Voluntary eating behaviors are followed by a reinforcing stimulus—the taste of food. Because of prior reinforcement experiences, people develop preferences for certain tastes, especially sweet, salty, and fatty tastes. Hence, your motivation to eat is influenced by prior learning experiences that have shaped your expectations, especially the anticipated pleasure of eating certain foods.
Let’s consider a different question: Why do we stop eating? Satiation is the feeling of fullness and diminished desire to eat that follows eating. But what triggers the sense of satiation? One satiation signal involves stretch receptors in the stomach that communicate sensory information to the brainstem. The sensitivity of the stomach’s stretch receptors is increased by a hormone secreted by the small intestines, called cholecystokinin, which is thankfully abbreviated as CCK. In the brain, CCK acts as a neurotransmitter (Delzenne & others, 2010).
Psychological factors play a role in satiation, too. As you eat a meal, food becomes less appealing, especially the specific food that you are eating. By the fourth piece of pizza, the pizza’s appeal begins to diminish. This phenomenon is termed sensory-
Long-Term Signals That Regulate Body Weight
Psychologists and other researchers have discovered many different chemical messengers that monitor and help us maintain a stable body weight over time. Three of the best-
Leptin is a hormone secreted by the body’s adipose tissue into the bloodstream. The amount of leptin that is secreted is directly correlated with the amount of body fat. The brain receptor sites for leptin are located in several areas of the hypothalamus. Neurons in the stomach and the gut also have leptin receptor sites.

Leptin is a key element in the feedback loop that regulates energy homeostasis. When fat stores increase, so do blood levels of leptin. When the leptin level in the brain increases, food intake is reduced and the body’s fat stores shrink over time. When fat stores shrink, blood levels of leptin decrease, triggering eating behavior.
The hormone insulin is also involved in brain mechanisms controlling food intake and body weight. The amount of insulin secreted by the pancreas is directly proportional to the amount of body fat. In the brain, insulin receptors are located in the same hypothalamus areas as leptin receptors. Increased brain levels of insulin are also associated with a reduction in food intake and body weight.
Abbreviated NPY, neuropeptide Y is a neurotransmitter manufactured throughout the brain, including the hypothalamus. During periods of weight loss, decreased leptin and insulin levels promote the secretion of NPY by the hypothalamus (Powley, 2009). In turn, increased brain levels of neuropeptide Y trigger eating behavior, reduce body metabolism, and promote fat storage. Conversely, if weight gain occurs, neuropeptide Y activity decreases.
In combination, the long-
According to set-
Excess Weight and Obesity
KEY THEME
Many different factors contribute to the high rates of overweight and obesity in the United States and other countries.
KEY QUESTIONS
What is BMI?
What factors contribute to excess weight and obesity?
The “thin ideal” is pervasive in American culture. In fact, over the past decades, actresses, models, Miss America Pageant winners, Playboy centerfolds, and even cartoon characters have become progressively thinner (Grabe & others, 2008).
But there is an enormous gap between the cultural ideal of a slender body and the cultural reality of the expanding American waistline. Far from conforming to the “thin ideal,” more than two-

You can calculate your BMI (body mass index) using the handy calculator at this Web site:
http://tinyurl.com/b53foz
BMI is often used as a “quick and dirty” measure of obesity because it can be easily calculated. However, many researchers prefer measures of waist circumference as a measure of obesity, because it indicates the amount of abdominal fat—
How is healthy weight determined? For statistical purposes, the most widely used measure of weight status is body mass index, abbreviated BMI. For adults, the body mass index provides a single numerical value that reflects your weight in relation to your height. A healthy BMI falls between 18 and 25. Generally, people with a BMI between 25 and 29.9 are considered overweight, unless their high BMI is due to muscle or bone rather than fat. Thus, it is possible to have a high BMI and still be very healthy, as are many athletes or bodybuilders. In contrast, people who are obese have a BMI of 30 or greater and an abnormally high proportion of body fat.
Another simple measure of obesity is waist circumference. According to this measure, an adult male’s waist should be no more than 40 inches in circumference, and an adult woman’s waist should be no more than 35 inches. Some researchers prefer this as a measure of obesity because it indicates the amount of abdominal fat tissue, which is considered to be most damaging to physical health.
More than one-
FACTORS INVOLVED IN BECOMING OVERWEIGHT
In the simplest terms, people become overweight when they habitually take in more calories than the amount of energy they expend. That said, multiple factors affect how much people eat and how the calories are metabolized. These factors include:
The “Supersize It” Syndrome: Overeating In the past two decades, average daily caloric intake has increased nearly 10 percent for men and 7 percent for women (Piernas & Popkin, 2011). Children, too, have significantly increased their caloric intake over the same period (Lobstein & others, 2015).
- Page 322
Positive Incentive Value: Highly Palatable Foods Rather than being motivated by hunger, we are often enticed to eat by the positive incentive value of the available foods and the anticipated pleasures of consuming those highly palatable foods (Carr & Epstein, 2011; Epstein & others, 2007).
The Cafeteria Diet Effect: Variety = More Consumed We consume more food when offered a variety of highly palatable foods, such as at a cafeteria or an all-
you- can- eat buffet (Epstein & others, 2010). This is sometimes called the cafeteria diet effect. Sedentary Lifestyles One recent study of almost 300,000 people living in 76 countries found that approximately 1 in 5 persons worldwide leads a sedentary lifestyle, engaging in less than 30 minutes of moderate activity on most days of the week (Dumith & others, 2011). Sedentary lifestyles are more common in urbanized, developed countries than in less developed or more rural countries. And, in the United States, people have become increasingly less active over the past few decades: From 1994 to 2010, the number of women who reported no physical activity during their leisure hours jumped from about 20% to over 50%. For men, the percentage rose from about 11% to 43% (Ladabaum & others, 2014).
Too Little Sleep: Disrupting Hunger Hormones Multiple studies have shown that not getting adequate sleep disrupts metabolism, including the hunger-
related hormones leptin and ghrelin (Taheri & others, 2004). People who sleep fewer than seven hours a night have higher BMIs than people who sleep nine hours or more, and are much more likely to be overweight or obese (Paunio, 2012; Watson & others, 2012). And, when sleep- deprived, people tend to prefer calorie- rich foods like chocolate and potato chips over healthier fare (Greer & others, 2013). - Page 323
Individual Differences and Lifespan Changes Finally, not everyone who overeats gains excess weight. One reason is that people vary greatly in their basal metabolic rate, which accounts for about two-
thirds of your energy expenditure. On average, women have a metabolic rate that is 3 to 5 percent lower than men’s. Metabolism also decreases with age, so that less food is required to meet your basic energy needs. Consequently, it’s not surprising that many people, upon reaching early adulthood, must begin to watch how much they eat.
Of the six factors we’ve covered here, you can exert control over five of them—

CRITICAL THINKING
Has Evolution Programmed Us to Overeat?
The negative consequences of obesity are well known. Along with health problems, people who are overweight or obese are stigmatized in our society—
Psychologist Bruce King (2013) believes that the evolutionary perspective provides several insights. For animals in the wild, food sources are often sporadic and unpredictable. When animals do find food, competition for it can be fierce, even deadly. If an animal waited to eat until it was hungry and its energy reserves were significantly diminished, it would run the risk of starving or falling prey to another animal. Thus, the eating patterns of many animals have evolved so that they readily eat even if not hungry (Berthoud, 2007; Zheng & others, 2009).

Similarly, our prehistoric human ancestors, relying upon the availability of wild game or plant foods, would have also experienced periods of both plentiful food and food shortages. According to King (2013), as a survival mechanism, prehistoric humans would have consumed as much food as possible during times of abundance. Overeating when food is available ensures ample energy reserves to survive times when food is not available.
But for most people living in food-
But unlike our evolutionary ancestors who had to hunt game or forage for seeds, nuts, and fruits, today’s humans simply don’t need to expend physical energy to acquire the food they need to meet their physical needs. As Pinel and his colleagues (2000) explain, “The increases in the availability of high positive-
CRITICAL THINKING QUESTIONS
How might the behavior of overeating be explained by instinct, drive, incentive, and arousal theories?
How could the insights provided by the evolutionary explanation be used to resist the temptation to overeat?
FACTORS INVOLVED IN OBESITY
Especially in the past decade, there has been intensive research investigating the causes of obesity—
MYTH SCIENCE
Is it true that obesity is primarily due to genetics?
Several variables derail the normal mechanisms of energy homeostasis in obesity. First, genetics plays a role. Current research suggests that multiple genes on multiple chromosomes are involved in creating susceptibility to obesity (Friedman, 2009). People with a family history of obesity are two to three times more likely than people with no such family history to become obese. And, the more closely related two people are genetically, the more likely they are to have similar body mass indexes (Bell & others, 2005).
But genetics is not destiny. Even though someone may be genetically predisposed to obesity, environmental factors play an important role. If an individual is genetically susceptible and lives in a high-
Once a person is overweight, metabolic factors are also important. For example, many obese people experience leptin resistance, in which the normal mechanisms through which leptin regulates body weight and energy balance are disrupted (Enriori & others, 2006; Morrison, 2008).


Is this chapter making you hungry? Video Activity: Hunger and Eating explores the factors that cue eating behavior and contribute to weight gain.
Eating habits, of course, affect weight. And while any diet that reduces caloric intake will result in weight loss, the more difficult challenge is to maintain the lower weight. Many overweight or obese dieters experience weight cycling, or yo-
One reason this occurs is because the human body is much more effective at vigorously defending against weight loss than it is at protecting against weight gain (Keel & others, 2007). As caloric intake is reduced and fat cells begin to shrink, the body actively defends against weight loss by decreasing metabolism rate and energy level. With energy expenditure reduced, far fewer calories are needed to maintain the excess weight. In effect, the body is using energy much more efficiently. If dieters continue to restrict caloric intake, weight loss will plateau in a matter of weeks. When they go off the diet, their now more energy-
Test your understanding of Hunger and Eating with  .
.

FOCUS ON NEUROSCIENCE
Dopamine Receptors and Obesity
Eating to Stimulate Brain Reward?
In Chapter 2, we noted that dopamine brain pathways are involved in the reinforcing feelings of pleasure and satisfaction. In Chapter 4, we also noted that many addictive drugs produce their pleasurable effects by increasing brain dopamine levels. These pleasurable effects are most reinforcing in people who have low levels of dopamine brain receptors (Volkow & others, 2007, 2011b). Given that eating can be highly reinforcing and produces pleasurable sensations, could the same mechanisms also play a role in obesity?
In a landmark study, researchers compared dopamine receptors in normal-
But is the lower number of dopamine receptors a cause or a consequence of obesity? In a recent study, one group of rats was allowed to eat as much as they wanted of rat chow—
The rats on the junk-
Even more interesting was what happened to the rats’ brain chemistry. Much like the brain changes associated with drug addiction, dopamine response in the junk-
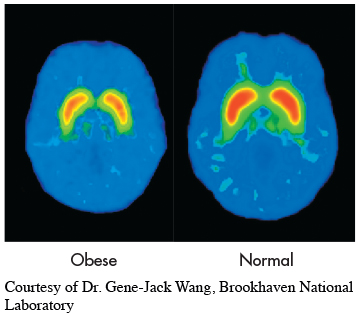
Can overeating lead to brain changes in humans, too? Neuroscientist Eric Stice and his colleagues (2010) used fMRI to scan the brains of overweight women while they drank a rich chocolate milkshake. Six months later, the women returned to the lab and repeated the experience. Some of the women had gained a few pounds, and others had not. The researchers found that there was no difference in the response to the milkshake in the women whose weight had remained stable. But women who had gained weight showed a significant reduction in the response of their brain reward system to the milkshake: the more weight gained, the greater the reduction in dopamine response to the milkshake as compared to six months previously.
Such results imply that obesity can be a vicious circle: People eat more to compensate for reduced brain rewards, but overeating reduces the dopamine reward system levels even further. These findings help explain why people continue to overeat despite suffering the unhealthy consequences of obesity.