Schizophrenia
A DIFFERENT REALITY
KEY THEME
One of the most serious psychological disorders is schizophrenia, which involves severely distorted beliefs, perceptions, and thought processes.
KEY QUESTIONS
What are the major symptoms of schizophrenia, and how do positive and negative symptoms differ?
How does culture affect the symptoms of schizophrenia?
What factors have been implicated in the development of schizophrenia?
Normally, you’ve got a pretty good grip on reality. You can easily distinguish between external reality and the different kinds of mental states that you routinely experience, such as dreams or daydreams. But as we negotiate life’s many twists and turns, the ability to stay firmly anchored in reality is not a given. Rather, we’re engaged in an ongoing process of verifying the accuracy of our thoughts, beliefs, and perceptions.
MYTH SCIENCE
Is it true that people with schizophrenia have a split personality?
If any mental disorder demonstrates the potential for losing touch with reality, it’s the one that Elyn Saks suffered from, schizophrenia. In media accounts and casual conversation, a person with schizophrenia is often mistakenly described as having “a split personality.” Elyn Saks explains the distinction: “the schizophrenic mind is not split, but shattered” (Saks, 2008). Schizophrenia is a psychological disorder that involves severely distorted beliefs, perceptions, and thought processes. During a schizophrenic episode, people lose their grip on reality, like Elyn screaming “I’m flying!” in the chapter Prologue. They become engulfed in an entirely different inner world, one that is often characterized by mental chaos, disorientation, and frustration.
Symptoms of Schizophrenia
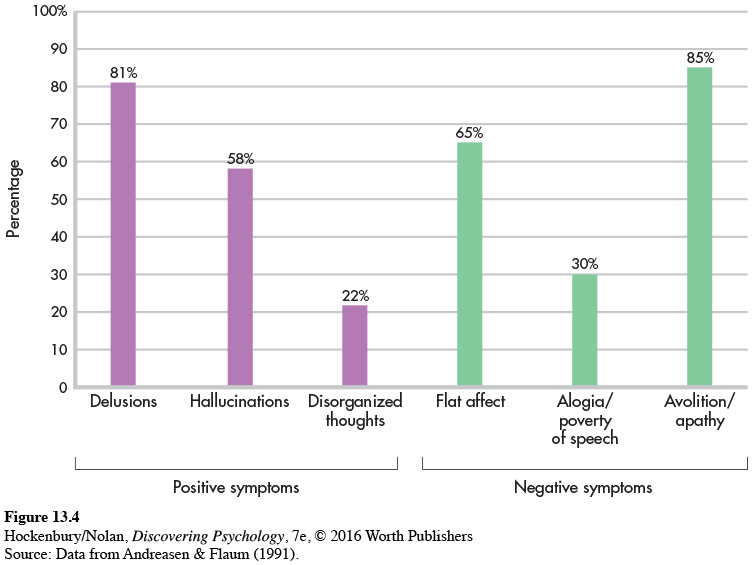
The characteristic symptoms of schizophrenia can be described in terms of two broad categories: positive and negative symptoms. Positive symptoms reflect an excess or distortion of normal functioning. Positive symptoms includes: (1) delusions, or false beliefs; (2) hallucinations, or false perceptions; (3) severely disorganized thought processes and speech; and (4) severely disorganized behavior. In contrast, negative symptoms reflect an absence or reduction of normal functions, such as greatly reduced motivation, emotional expressiveness, or speech.
According to DSM-
Schizophrenia may be diagnosed either with or without catatonia (DSM-
POSITIVE SYMPTOMS
DELUSIONS, HALLUCINATIONS, AND DISTURBANCES IN SENSATION, THINKING, AND SPEECH
A delusion is a false belief that persists despite compelling contradictory evidence. Schizophrenic delusions are not simply unconventional or inaccurate beliefs. Rather, they are bizarre and far-
Certain themes consistently appear in schizophrenic delusions. Delusions of reference reflect the person’s false conviction that other people’s behavior and ordinary events are somehow personally related to her. For example, she is certain that billboards and advertisements are about her or contain cryptic messages directed at her. In contrast, delusions of grandeur involve the belief that the person is extremely powerful, important, or wealthy. In delusions of persecution, the basic theme is that others are plotting against or trying to harm the person or someone close to her. Delusions of being controlled involve the belief that outside forces—

FOCUS ON NEUROSCIENCE
The Hallucinating Brain
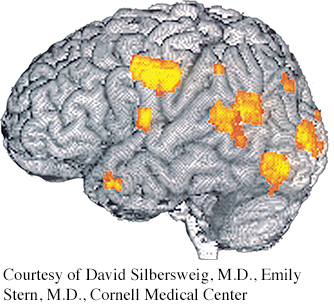
Researcher David Silbersweig and his colleagues (1995) used PET scans to take a “snapshot” of brain activity during schizophrenic hallucinations. The scan shown here was recorded at the exact instant a schizophrenic patient hallucinated disembodied heads yelling orders at him. The bright orange areas reveal activity in the left auditory and visual areas of his brain, but not in the frontal lobe, which normally is involved in organized thought processes.
Schizophrenic delusions are often so convincing that they can provoke inappropriate or bizarre behavior. Delusional thinking may lead to dangerous behaviors, as when a person responds to his delusional ideas by hurting himself or attacking others.
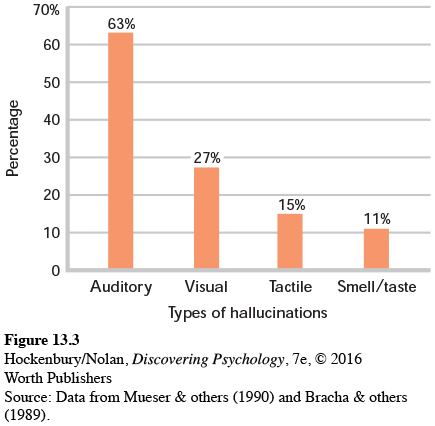
Among the most disturbing experiences in schizophrenia are hallucinations, which are false or distorted perceptions—
People with schizophrenia might hear the roars of Satan or the whispers of children. They might move armies with their thoughts and receive instructions from other worlds. They might feel penetrated by scheming parasites, stalked by enemies, or praised by guardian angels. People with schizophrenia might also speak nonsensically, their language at once intricate and impenetrable. And many would push, or be pushed, to the edge of the social landscape, overcome by solitude.
—R. Walter Heinrichs (2005)
When a schizophrenic episode is severe, hallucinations can be virtually impossible to distinguish from objective reality. For example, Elyn reported that she could sometimes hear someone calling her name when she knew she was completely alone (Saks, 2008). When schizophrenic symptoms are less severe, the person may recognize that the hallucination is a product of his own mind. As Elyn reported, she knew that she had to try to control her psychotic thoughts at school and in social settings and was sometimes able to do so.
Other positive symptoms of schizophrenia include disturbances in sensation, thinking, and speech. Visual, auditory, and tactile experiences may seem distorted or unreal. For example, one woman described the sensory distortions in this way:
Looking around the room, I found that things had lost their emotional meaning. They were larger than life, tense, and suspenseful. They were flat, and colored as if in artificial light. I felt my body to be first giant, then minuscule. My arms seemed to be several inches longer than before and did not feel as though they belonged to me. (Anonymous, 1990)
Along with sensory distortions, the person may experience severely disorganized thinking. It becomes enormously difficult to concentrate, remember, and integrate important information while ignoring irrelevant information (Barch, 2005). The person’s mind drifts from topic to topic in an unpredictable, illogical manner, such as the Prologue example of Elyn’s ramblings to her classmates. Such disorganized thinking is often reflected in the person’s speech (Badcock & others, 2011). Ideas, words, and images are sometimes strung together in ways that seem nonsensical to the listener.
NEGATIVE SYMPTOMS
FLAT AFFECT, ALOGIA, AND AVOLITION
Negative symptoms consist of marked deficits or decreases in behavioral or emotional functioning. One commonly seen negative symptom is referred to as diminished emotional expression or flat affect. Regardless of the situation, the person responds in an emotionally “flat” way, showing a dramatic reduction in emotional responsiveness and facial expressions. Speech is slow and monotonous, lacking normal vocal inflections. A closely related negative symptom is alogia, or greatly reduced production of speech. In alogia, verbal responses are limited to brief, empty comments.
Finally, avolition refers to the inability to initiate or persist in even simple forms of goal-
Schizophrenia Symptoms and Culture
Symptoms of schizophrenia often vary across cultures. For example, there can be cultural variations in delusional themes and the content of hallucinations (Bauer & others, 2011).
Delusions are a prime example of a symptom often rooted in culture. Indeed, some themes that would be considered to be delusional in one culture might be widely held beliefs in another culture. The International Study on Psychotic Symptoms examined data from over 1,000 people with schizophrenia in seven countries: Austria, Georgia, Ghana, Lithuania, Nigeria, Pakistan, and Poland (Stompe & others, 2006). Among the delusions experienced by the people in this sample, 16.8 percent of the content was culturally specific. For example, in Nigeria and Ghana there were relatively high rates of delusions that involved “being an angel or a prophet,” concepts that are integral parts of these cultures.
Even within a single culture, the content of delusions changes as the culture shifts. A study of delusions in U.S. inpatient psychiatric patients found that delusions have changed over time. During World War II, delusions tended to center on Nazi soldiers. Recently, delusions are more likely to involve technology (Cannon & Kramer, 2012). Joel Gold and Ian Gold (2012) describe a common type of delusion involving technology—
The Prevalence and Course of Schizophrenia
Every year, about 200,000 new cases of schizophrenia are diagnosed in the United States, and annually, approximately 1 million Americans are treated for schizophrenia. All told, about 1 percent of the U.S. population will experience at least one episode of schizophrenia at some point in life (Rado & Janicak, 2009). Worldwide, no society or culture is immune to this mental disorder. Researchers have long believed that most cultures correspond very closely to the 1 percent rate of schizophrenia seen in the United States (Minzenberg & others, 2011). However, a comprehensive review of almost 200 studies concluded that global rates of schizophrenia were closer to 4 percent, meaning that schizophrenia may be far more widespread than once believed (Saha & others, 2005).

The onset of schizophrenia typically occurs during young adulthood, as it did with Elyn (Gogtay & others, 2011). However, the course of schizophrenia is marked by enormous individual variability. Even so, a few global generalizations are possible (Malla & Payne, 2005; Walker & others, 2004). The good news is that about one-
Now the bad news. For the rest of those who have experienced an episode of schizophrenia—
Cultural factors also seem to affect the outcome of schizophrenia. Despite less access to mental health care, people with schizophrenia often have a better outcome in the developing world than in the developed world (Haro & others, 2011; World Health Organization, 1998). For example, the World Health Organization (WHO) found that full recovery after a single episode of psychosis occurred in just 3 percent of cases in the United States but in 54 percent of cases in India. WHO (1998) suggests that people in the developing world might be more accepting of mental illness, and are more likely to have extended family support systems than people in the developed world.
Other studies have qualified these findings. For example, Josep Haro and others (2011) found that people with schizophrenia living in the developing world tended to experience a greater decline in their symptoms over time than those with schizophrenia living in the developed world. But they also fared worse in terms of life skills, such as holding a job and living independently. The decline in symptoms did not coincide with improved life functioning. Clearly, culture is an important factor in the experience and course of schizophrenia.
Explaining Schizophrenia
Schizophrenia is an extremely complex disorder. There is enormous individual variability in the onset, symptoms, and duration of and recovery from schizophrenia. So it shouldn’t come as a surprise that the causes of schizophrenia seem to be equally complex. In this section, we’ll survey some of the factors that have been implicated in the development of schizophrenia.
GENETIC FACTORS
FAMILY, TWIN, ADOPTION, AND GENE STUDIES
Studies of families, twins, and adopted individuals have firmly established that genetic factors play a significant role in many cases of schizophrenia (Pogue-
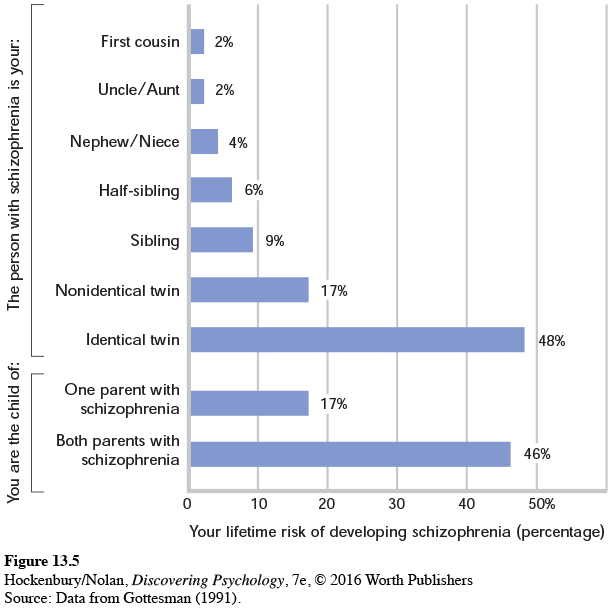
Ironically, some of the best evidence that points to genetic involvement in schizophrenia—
Nevertheless, scientists are getting closer to identifying some of the specific genetic patterns that are associated with an increased risk of developing schizophrenia. New research using sophisticated gene analysis techniques confirms the incredibly complex role that genes play in the development of schizophrenia (Gilman & others, 2012; Rapoport & others, 2012). For example, one study of people with schizophrenia with no family history of the disease found that genetic mutations were much higher in the schizophrenic patients than in individuals without schizophrenia (Girard & others, 2011). These mutations were present in many different genes, including genes that had not previously been associated with schizophrenia.
In another large-
Collectively, the studies found that schizophrenia was associated with literally thousands of common gene variations. Some of the specific variants were quite rare, while others were quite common. Taken individually, none of the gene variants is capable of “causing” schizophrenia. Even in combination, the genetic variants are only associated with an increased risk of developing schizophrenia.
As yet, no specific pattern of genetic variation can be identified as the genetic “cause” of schizophrenia. However, three particularly interesting findings stand out. First, some of the same unique genetic patterns associated with schizophrenia have also been found in DNA samples from people with bipolar disorder (Purcell & others, 2009). This finding suggests that bipolar disorder and schizophrenia might share some common genetic origins. Second, also implicated were several chromosome locations that are associated with genes that influence brain development, memory, and cognition. Finally, a large number of the gene variants were found to occur on a specific chromosome that is also known to harbor genes involved in the immune response (Shi & others, 2009). Later in this section, we’ll discuss some intriguing links between viral infections and schizophrenia, which suggests that the immune system may be implicated in the development of schizophrenia.
PATERNAL AGE
OLDER FATHERS AND THE RISK OF SCHIZOPHRENIA
Despite the fact that family and twin studies point to the role of genetic factors in the risk of developing schizophrenia, no genetic model thus far explains all of the patterns of schizophrenia occurrence within families (Insel & Lehner, 2007). Adding to the complexity, schizophrenia often occurs in individuals with no family history of mental disorders. Elyn, for example, has an uncle who suffered from depression but no close relatives who suffered from schizophrenia or any other serious mental disorders (Saks, 2008).
One explanation for these anomalies is that for each generation, new cases of schizophrenia arise from genetic mutations carried in the sperm of the biological fathers, especially older fathers. As men age, their sperm cells continue to reproduce by dividing. By the time a male is 20, his sperm cells have undergone about 200 divisions; by the time he is 40, there have been about 660 divisions. As the number of divisions increases over time, the sperm cells accumulate genetic mutations that can then be passed on to that man’s offspring. Hence, the theory goes, as paternal age increases, the risk of offspring developing schizophrenia also increases (Bajwa & others, 2011). While paternal age is a potential risk factor, it’s important to keep in mind that three-
THE IMMUNE SYSTEM
THE VIRAL INFECTION THEORY
Another provocative theory is that schizophrenia might be caused by exposure to an influenza virus or other viral infection during prenatal development or shortly after birth (Carter, 2008; Yudofsky, 2009). A virus might seem an unlikely cause of a serious mental disorder, but viruses can spread to the brain and spinal cord by traveling along nerves. According to this theory, exposure to a viral infection during prenatal development or early infancy affects the developing brain, producing changes that make the individual more vulnerable to schizophrenia later in life.
There is growing evidence to support the viral infection theory. In one compelling study, psychiatrist Alan S. Brown and his colleagues (2004) compared stored blood samples of 64 mothers of people who later developed schizophrenia with a matched set of blood samples from women whose children did not develop schizophrenia. Both sets of blood samples had been collected years earlier during the women’s pregnancies. After analyzing the blood samples for the presence of influenza antibodies, Brown and his colleagues (2004) found that women who had been exposed to the flu virus during the first trimester had a sevenfold increased risk of bearing a child who later developed schizophrenia. A related finding is that schizophrenia occurs more often in people who were born in the winter and spring months, when upper respiratory infections are most common (Disanto & others, 2012; Torrey & others, 1996).
ABNORMAL BRAIN STRUCTURES
LOSS OF GRAY MATTER
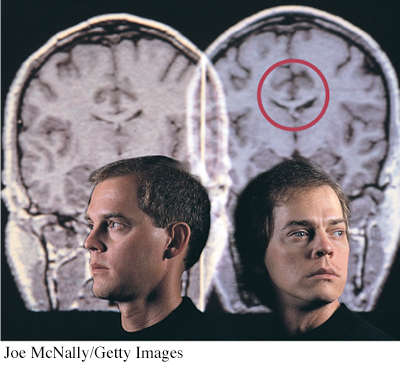
Researchers have found that about half of the people with schizophrenia show some type of brain structure abnormality. The most consistent finding has been the enlargement of the fluid-
Other differences that have been found are a loss of gray matter tissue and lower overall volume of the brain (Olabi & others, 2011; Vita & others, 2012). As we discussed in Chapter 2, gray matter refers to the glial cells, neuron cell bodies, and unmyelinated axons that make up the quarter-
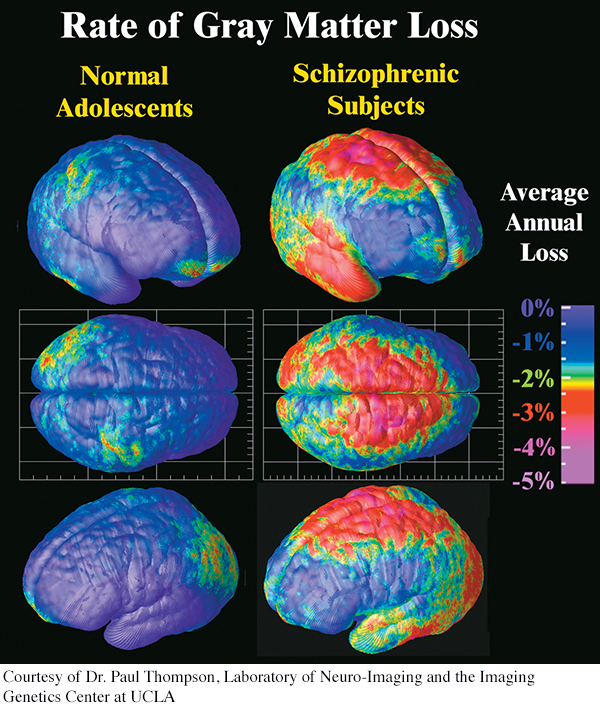
To investigate the neurological development of schizophrenia, neuroscientist Paul M. Thompson and his colleagues (2001) undertook a prospective study of brain structure changes in 12 adolescents with early-
Each of the 12 adolescents was scanned repeatedly with high-
Although there is evidence that brain abnormalities are found in schizophrenia, such findings do not prove that brain abnormalities are the sole cause of schizophrenia. First, some people with schizophrenia do not show brain structure abnormalities. Second, the evidence is correlational. Researchers are still investigating whether differences in brain structures and activity are the cause or the consequence of schizophrenia. Third, the kinds of brain abnormalities seen in schizophrenia are also seen in other mental disorders. Rather than specifically causing schizophrenia, it’s quite possible that brain abnormalities might contribute to psychological disorders in general.
ABNORMAL BRAIN CHEMISTRY
HYPOTHESES RELATED TO NEUROTRANSMITTERS
There are several hypotheses that attribute schizophrenia to imbalances in neurotransmitters. The oldest of these is the dopamine hypothesis, which attributes schizophrenia to excessive activity of the neurotransmitter dopamine in the brain. Two pieces of indirect evidence support this notion. First, antipsychotic drugs, such as Haldol, Thorazine, and Stelazine, reduce or block dopamine activity in the brain. These drugs reduce schizophrenic symptoms, especially positive symptoms, in many people. Second, drugs that enhance dopamine activity in the brain, such as amphetamines and cocaine, can produce schizophrenia-

FOCUS ON NEUROSCIENCE
Schizophrenia: A Wildfire in the Brain
In a five-
But in sharp contrast to the normal teens, the teenagers with schizophrenia showed a severe loss of gray matter that developed in a specific, wavelike pattern. The loss began in the parietal lobes and, over the five years of the study, progressively spread forward to the temporal and frontal regions. As Thompson (2001) noted, “We were stunned to see a spreading wave of tissue loss that began in a small region of the brain. It moved across the brain like a forest fire, destroying more tissue as the disease progressed.”
The brain images show the average rate of gray matter loss over the five-
Also, the pattern of loss mirrored the progression of neurological and cognitive deficits associated with schizophrenia. For example, more rapid gray matter loss in the temporal lobes was associated with more severe positive symptoms, such as hallucinations and delusions. More rapid loss of gray matter in the frontal lobes was strongly correlated with the severity of negative symptoms, including flat affect and poverty of speech. When the participants were 18 to 19 years old and the final brain scans were taken, the patterns of gray matter loss were similar to those found in the brains of adult patients with schizophrenia.
Despite the wealth of information generated by Thompson’s study, the critical question remains unanswered: What sparks the cerebral forest fire in the schizophrenic brain?
However, there is also evidence that contradicts the dopamine hypothesis (Jucaite & Nyberg, 2012). For example, not all individuals who have schizophrenia experience a reduction of symptoms in response to the antipsychotic drugs that reduce dopamine activity in the brain. And for many patients, these drugs reduce some but not all schizophrenic symptoms, and tend to reduce positive symptoms more than negative symptoms (Kendler & Schaffner, 2011). One new theory is that some parts of the brain, such as the limbic system, may have too much dopamine, while other parts of the brain, such as the cortex, may have too little (Combs & Mueser, 2007; Kendler & Schaffner, 2011). There also is increasing evidence that imbalances in other neurotransmitters—
PSYCHOLOGICAL FACTORS
UNHEALTHY FAMILIES
Researchers have investigated such factors as dysfunctional parenting, disturbed family communication styles, and critical or guilt-
Strong support for this view comes from a landmark study conducted by Finnish psychiatrist Pekka Tienari and his colleagues (1987, 1994). In the Finnish Adoptive Family Study of Schizophrenia, researchers followed about 150 adopted individuals whose biological mothers had schizophrenia. As part of their study, the researchers assessed the adoptive family’s degree of psychological adjustment, including the mental health of the adoptive parents. The study also included a control group of about 180 adopted individuals whose biological mothers did not have schizophrenia.
Tienari and his colleagues (1994, 2006; Wynne & others, 2006) found that adopted children with a schizophrenic biological mother had a much higher rate of schizophrenia than did the children in the control group. However, this was true only when the children were raised in a psychologically disturbed adoptive home. As you can see in Figure 13.6, when children with a genetic background of schizophrenia were raised in a psychologically healthy adoptive family, they were no more likely than the control-
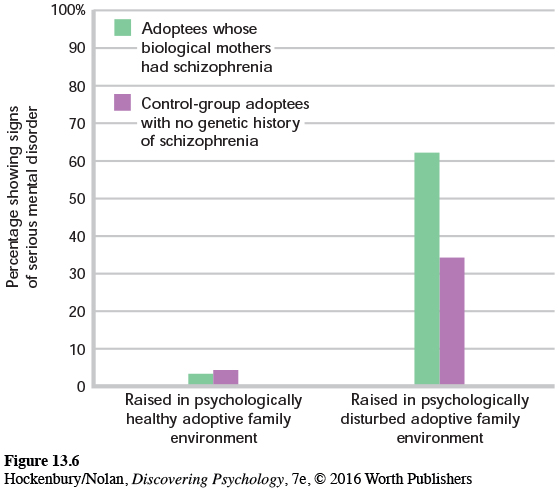
Although adopted children with no genetic history of schizophrenia were less vulnerable to the psychological stresses of a disturbed family environment, they were by no means completely immune to such influences. As Figure 13.6 shows, one-
Tienari’s study underscores the complex interaction of genetic and environmental factors. Clearly, children who were genetically at risk to develop schizophrenia benefited from being raised in a healthy psychological environment. Put simply, a healthy psychological environment may counteract a person’s inherited vulnerability for schizophrenia. Conversely, a psychologically unhealthy family environment can act as a catalyst for the onset of schizophrenia, especially for those individuals with a genetic history of schizophrenia (Tienari & Wahlberg, 2008).
After more than a century of intensive research, schizophrenia remains a baffling disorder. Thus far, no single biological, psychological, or social factor has emerged as the causal agent in schizophrenia. And it’s virtually impossible to know what caused schizophrenia in any single individual like Elyn. Nevertheless, researchers are expressing greater confidence that the pieces of the schizophrenia puzzle are beginning to form a more coherent picture.
Even if the exact causes of schizophrenia remain elusive, there is still reason for optimism. In the past few years, new antipsychotic drugs, such as those that Elyn takes, have been developed that are much more effective in treating both the positive and negative symptoms of schizophrenia (Sharif & others, 2007). In the next chapter, we’ll take a detailed look at the different treatments and therapies for schizophrenia and other psychological disorders.
Test your understanding of Schizophrenia with  .
.