Behavior Therapy
KEY THEME
Behavior therapy uses learning principles to directly change problem behaviors.
KEY QUESTIONS
What are the key assumptions of behavior therapy?
What therapeutic techniques are based on classical conditioning, and how are they used to treat psychological disorders and problems?
What therapy treatments are based on operant conditioning, and how are they used to treat psychological disorders and problems?
Psychoanalysis, client-

However, gaining insight into the source of problems does not necessarily result in desirable changes in behavior and emotions. Even though you fully understand why you are behaving in counterproductive ways, your maladaptive or self-
In sharp contrast to the insight-
Behavior therapists assume that maladaptive behaviors are learned, just as adaptive behaviors are. Thus, the basic strategy in behavior therapy involves unlearning maladaptive behaviors and learning more adaptive behaviors in their place. Behavior therapists employ techniques that are based on the learning principles of classical conditioning, operant conditioning, and observational learning to modify the problem behavior.
Techniques Based on Classical Conditioning
Just as Pavlov’s dogs learned to salivate to a ringing bell that had become associated with food, learned associations can be at the core of some maladaptive behaviors, including strong negative emotional reactions. In the 1920s, psychologist John Watson demonstrated this phenomenon with his famous “Little Albert” study. In Chapter 5, we described how Watson classically conditioned an infant known as Little Albert to fear a tame lab rat by repeatedly pairing the rat with a loud clanging sound. Over time, Albert’s conditioned fear generalized to other furry objects, including a fur coat, cotton, and a Santa Claus mask (Watson & Rayner, 1920).
MARY COVER JONES
THE FIRST BEHAVIOR THERAPIST
Watson himself never tried to eliminate Little Albert’s fears. But Watson’s research inspired one of his students, Mary Cover Jones, to explore ways of reversing conditioned fears. With Watson acting as a consultant, Jones (1924a) treated a 3-
Jones’s procedure was very simple ( Jones, 1924b; Watson, 1924). The caged rabbit was brought into Peter’s view but kept far enough away to avoid eliciting fear (the original conditioned response). With the rabbit visible at a tolerable distance, Peter sat in a high chair and happily munched his favorite snack, milk and crackers. Peter’s favorite food was used because, presumably, the enjoyment of eating would naturally elicit a positive response (the desired conditioned response). Such a positive response would be incompatible with the negative response of fear.
Every day for almost two months, the rabbit was inched closer and closer to Peter as he ate his milk and crackers. As Peter’s tolerance for the rabbit’s presence gradually increased, he was eventually able to hold the rabbit in his lap, petting it with one hand while happily eating with his other hand ( Jones, 1924a, 1924b). Not only was Peter’s fear of the rabbit eliminated, but he also stopped being afraid of other furry objects, including the rat, cotton, and the fur coat (Watson, 1924).
For her pioneering efforts in the treatment of children’s fears, Jones is widely regarded as the first behavior therapist (Gieser, 1993; Rutherford, 2006).
SYSTEMATIC DESENSITIZATION AND EXPOSURE THERAPIES
Mary Cover Jones’s pioneering studies in treating children’s fears laid the ground-
One widely used type of exposure therapy, called systematic desensitization, was developed by South African psychiatrist Joseph Wolpe in the 1950s (Wolpe, 1958, 1982). Based on the same premise as counterconditioning, systematic desensitization involves learning a new conditioned response (relaxation) that is incompatible with or inhibits the old conditioned response (fear and anxiety).
Three basic steps are involved in systematic desensitization. First, the patient learns progressive relaxation, which involves successively relaxing one muscle group after another until a deep state of relaxation is achieved. Second, the behavior therapist helps the patient construct an anxiety hierarchy, sometimes called an exposure hierarchy, which is a list of anxiety-
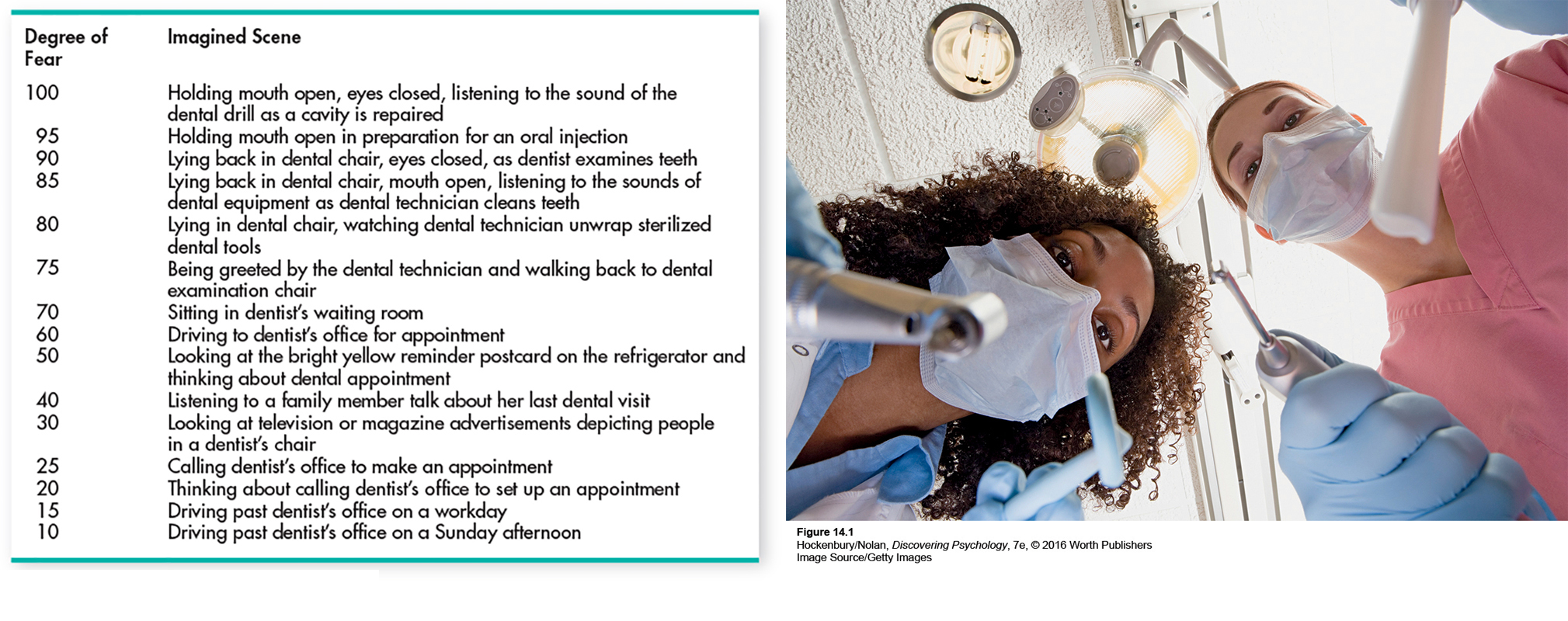
The third step involves the actual process of desensitization through exposure to feared experiences. While deeply relaxed, the patient imagines the least-
Over several sessions, the patient gradually and systematically works his way up the hierarchy, imagining each scene while maintaining complete relaxation. Once mastered with mental images, the desensitization procedure may be continued with exposure to the actual feared situation, which is called in vivo systematic desensitization. If the technique is successful, the feared situation no longer produces a conditioned response of fear and anxiety. The In Focus box “Using Virtual Reality to Treat Phobia and Posttraumatic Stress Disorder,” below, describes systematic desensitization using a “virtual reality” version of the actual feared situation.


To observe the type of exposure therapy used with OCD, watch Video Activity: Treating OCD: Exposure and Response Prevention.
In practice, systematic desensitization is often combined with other techniques, such as observational learning (Bandura, 2004b). Let’s consider a clinical example that combines systematic desensitization and observational learning. The client is Santiago, a 60-
Santiago is able to move through the hierarchy by experiencing relaxation in conjunction with exposure to each consecutive stimulus that might have produced anxiety. Because relaxation and anxiety are incompatible, the relaxation essentially “blocks” Santiago’s anxiety about flying, just as Peter’s enjoyment of his milk and cookies blocked his anxiety about the rabbit. Another important aspect of the behavior therapist’s treatment of Santiago involves observational learning: She shows Santiago videos of people calmly boarding and riding on planes. Together, systematic desensitization and observational learning help Santiago overcome his phobia, and he is ultimately able to fly with minimal discomfort.

IN FOCUS
Using Virtual Reality to Treat Phobia and Posttraumatic Stress Disorder
Virtual reality (VR) therapy consists of computer-
VR technology was first used in the treatment of specific phobias, including fear of flying, heights, spiders, driving, and enclosed places (Côté & Bouchard, 2008). In the virtual reality scene, patients are progressively exposed to the feared object or situation. For example, psychologist Ralph Lamson used virtual reality as a form of computer-
Although computer-
Once experimental, virtual reality therapy has become an accepted treatment for specific phobias and is now being extended to other disorders, such as social anxiety disorder, panic disorder, and acrophobia (Meyerbröker & Emmelkamp, 2010; Opriş others, 2012). One innovative application of VR therapy is in the treatment of posttraumatic stress disorder (PTSD) in veterans of the wars in Vietnam, Iraq, and Afghanistan (McLay & others, 2011). Many PTSD patients are unable or unwilling to mentally re-
For example, a young woman who suffered from severe PTSD after witnessing and barely escaping the 9/11 attack on the World Trade Center was finally able to relive the events of the day through controlled, graduated exposure to a virtual reenactment of the events. Similarly, war veterans can be exposed to the sights and sounds of combat in a way that could not be accomplished in the “real world” of a therapist’s office or a busy downtown street. Marine veteran Joshua Musser was treated with virtual reality therapy after fighting in Iraq and developing PTSD. Musser told CNN (2011), “It put you back in Iraq where you kind of have one foot here and one foot there. The only thing outside of Iraq that you hear is [the clinical psychologist’s] voice, and so when she sees that I’m really starting to stress out . . . she would be in my ear and be pulling me back.”
VR therapy is easier and less expensive to administer than graduated exposure to the actual feared object or situation. Another advantage is that the availability of VR may make people who are extremely phobic more willing to seek treatment. In one survey of people who were phobic of spiders, more than 80 percent preferred virtual reality treatment over graduated exposure to real spiders (Garcia-

A newer form of exposure therapy for people suffering from traumatic memories has received a great deal of attention. Eye movement desensitization reprocessing, abbreviated EMDR, involves patients visually following the waving finger of a therapist while simultaneously holding a mental image of disturbing memories, events, or situations. Early research by its founder, psychologist Francine Shapiro, found that most patients experienced significant relief from their symptoms after just one EMDR therapy session (Shapiro, 1989a, 1989b, 2007). This was the beginning of what was to become one of the fastest-

Yet, many elements of EMDR are similar to other treatment techniques, some of them well established and based on well-
AVERSIVE CONDITIONING
The psychologist John Garcia first demonstrated how taste aversions could be classically conditioned (see Chapter 5). After rats drank a sweet-
Aversive conditioning techniques have been applied to a wide variety of problem behaviors (Cain & LeDoux, 2008). However, mental health professionals are typically very cautious about the use of such techniques, partly because of their potential to harm or produce discomfort for clients (C. B. Fisher, 2009; Francis, 2009). In addition, aversive techniques are generally not very effective (Emmelkamp, 2004).
Techniques Based on Operant Conditioning
B. F. Skinner’s operant conditioning model of learning is based on the simple principle that behavior is shaped and maintained by its consequences (see Chapter 5). Behavior therapists have developed several treatment techniques that are derived from operant conditioning. Shaping involves reinforcing successive approximations of a desired behavior. Shaping is often used to teach appropriate behaviors to patients who are mentally disabled by autism spectrum disorder, intellectual disability, or severe mental illness. For example, shaping has been used to increase the attention span of hospitalized patients with severe schizophrenia (Combs & others, 2011; Mueser & others, 2013).
Other operant conditioning techniques involve controlling the consequences that follow behaviors. Positive and negative reinforcement are used to increase the incidence of desired behaviors. Extinction, or the absence of reinforcement, is used to reduce the occurrence of undesired behaviors.
Let’s illustrate how operant techniques are used in therapy by describing a behavioral program to treat a 4-
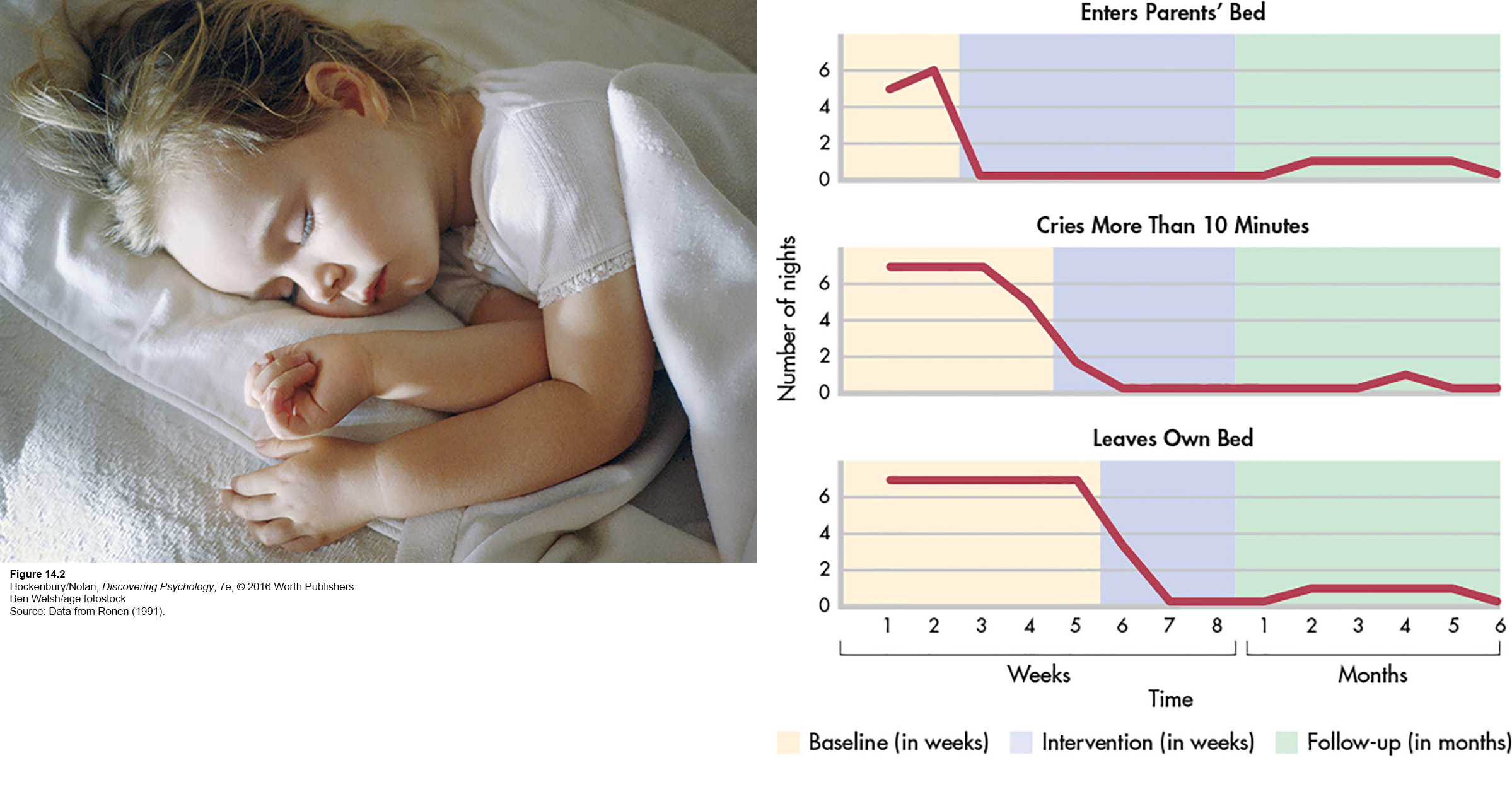
The parents were taught operant techniques to decrease the undesirable behaviors and increase desirable ones. For example, to extinguish the girl’s screaming and crying, the parents were taught to ignore the behavior rather than continue to reinforce it with parental attention. In contrast, desirable behaviors were to be positively reinforced with abundant praise, encouragement, social attention, and other rewards. Figure 14.2 shows the little girl’s progress for three specific problem behaviors.
Operant conditioning techniques have been applied to many different kinds of psychological problems, from habit and weight control to helping autistic children learn to speak and behave more adaptively.
The token economy is another example of the use of operant conditioning techniques to modify behavior. A token economy is a system for strengthening desired behaviors through positive reinforcement in a very structured environment. Basically, tokens or points are awarded as positive reinforcers for desirable behaviors and withheld or taken away for undesirable behaviors. The tokens can be exchanged for other reinforcers, such as special privileges.
Token economies have been most successful in controlled environments in which the behavior of the client is under ongoing surveillance or supervision. Thus, token economies have been used in classrooms, inpatient psychiatric units, and group homes (Field & others, 2004; Kamps & others, 2011; Kokaridas & others, 2013). Although effective, token economies are difficult to implement, especially in community-
A modified version of the token economy has been used with outpatients in treatment programs called contingency management. Like the token economy, a contingency management intervention involves carefully specified behaviors that “earn” the individual concrete rewards. Unlike token economies, which cover many behaviors, contingency management strategies are typically more narrowly focused on one or a small number of specific behaviors (Prochaska & Norcross, 2014). Contingency management interventions have proved to be especially effective in the outpatient treatment of people who are dependent on heroin, cocaine, alcohol, or multiple drugs (Higgins & others, 2011; Tuten & others, 2012).
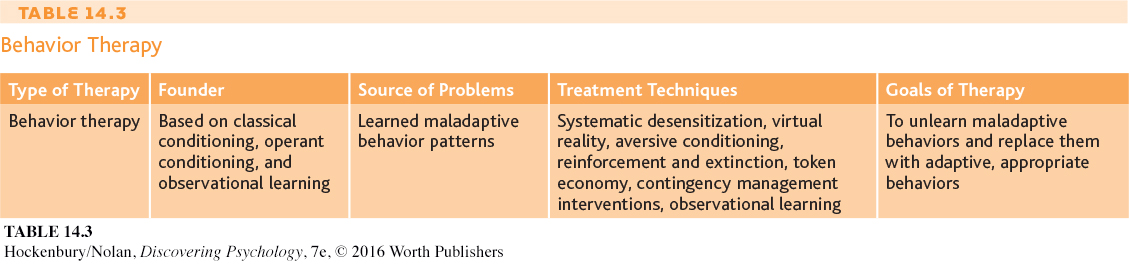
Table 14.3 summarizes key points about behavior therapy.