40.2 Classifying Disorders—and Labeling People
40-
In biology, classification creates order. To classify an animal as a “mammal” says a great deal—
But diagnostic classification gives more than a thumbnail sketch of a person’s disordered behavior, thoughts, or feelings. In psychiatry and psychology, classification also attempts to
predict a disorder’s future course.
suggest appropriate treatment.
prompt research into a disorder’s causes.
DSM-5 the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; a widely used system for classifying psychological disorders.
The most common tool for describing disorders and estimating how often they occur is the American Psychiatric Association’s 2013 Diagnostic and Statistical Manual of Mental Disorders, now in its fifth edition (DSM-5). Physicians and mental health workers use the DSM-
Insomnia Disorder (American Psychiatric Association, 2013)
|
|
|
|
|
|
|
|
In the new DSM-
Real-
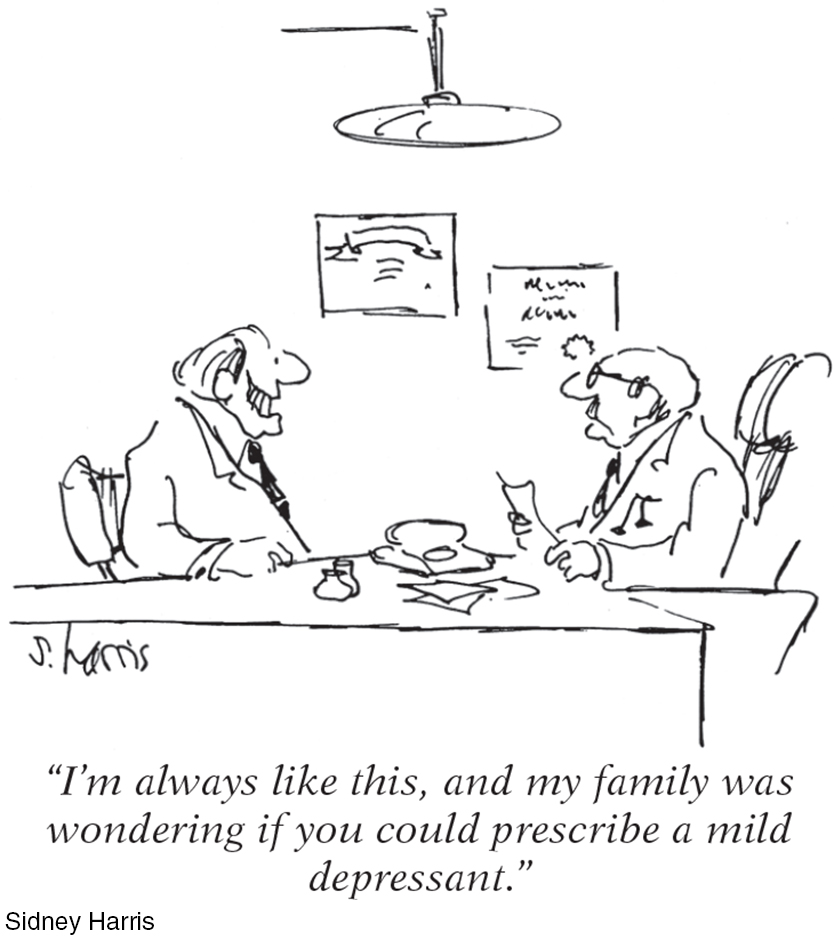
Critics have long faulted the DSM for casting too wide a net, and for bringing “almost any kind of behavior within the compass of psychiatry” (Eysenck et al., 1983). Some now worry that the DSM-
THINKING CRITICALLY ABOUT
ADHD—
40-
Eight-
attention-deficit/hyperactivity disorder (ADHD) a psychological disorder marked by extreme inattention and/or hyperactivity and impulsivity.
If taken for a psychological evaluation, Todd may be diagnosed with attention-deficit/hyperactivity disorder (ADHD). Some 11 percent of American 4-
To skeptics, being distractible, fidgety, and impulsive sounds like a “disorder” caused by a single genetic variation: a Y chromosome (the male sex chromosome). And sure enough, ADHD is diagnosed three times more often in boys than in girls. Does energetic child + boring school = ADHD overdiagnosis? Is the label being applied to healthy schoolchildren who, in more natural outdoor environments, would seem perfectly normal? Is ADHD a disease that is marketed by companies offering drugs that treat it (Thomas, 2015)?
Skeptics think so. In the decade after 1987, they note, the proportion of American children being treated for ADHD nearly quadrupled (Olfson et al., 2003). Minority youth less often receive an ADHD diagnosis than do White youth, but this difference has shrunk as minority ADHD diagnoses have increased (Genahun at al., 2013). How commonplace the diagnosis is depends in part on teacher referrals. Some teachers refer lots of kids for ADHD assessment, others none. ADHD rates have varied by a factor of 10 in different counties of New York State (Carlson, 2000). Depending on where they live, children who are “a persistent pain in the neck in school” are often diagnosed with ADHD and given powerful prescription drugs, notes Peter Gray (2010). But the problem may reside less in the child than in today’s abnormal environment, which forces children to do what evolution has not prepared them to do—
Not everyone agrees that ADHD is being overdiagnosed. Some argue that today’s more frequent diagnoses of ADHD reflect increased awareness of the disorder, especially in those areas where rates are highest. They acknowledge that diagnoses can be inconsistent—
What, then, is known about ADHD’s causes? It is not caused by too much sugar or poor schools. ADHD often coexists with a learning disorder or with defiant and temper-
The bottom line: Extreme inattention, hyperactivity, and impulsivity can derail social, academic, and vocational achievements, and these symptoms can be treated with medication and other therapies (Hinshaw & Scheffler, 2014). But the debate continues over whether normal high energy is too often diagnosed as a psychiatric disorder, and whether there is a cost to the long-
Other critics register a more basic complaint—
The biasing power of labels was clear in a classic study. David Rosenhan (1973) and seven others went to hospital admissions offices, complaining (falsely) of “hearing voices” saying empty, hollow, and thud. Apart from this complaint and giving false names and occupations, they answered questions truthfully. All eight healthy people were misdiagnosed with disorders.

Should we be surprised? Surely not. As one psychiatrist noted, if someone swallowed blood, went to an emergency room, and spat it up, would we blame a doctor for diagnosing a bleeding ulcer? But what followed the Rosenhan study diagnoses was startling. Until being released an average of 19 days later, these eight “patients” showed no other symptoms. Yet after analyzing their (quite normal) life histories, clinicians were able to “discover” the causes of their disorders, such as having mixed emotions about a parent. Even the patients’ routine note-
In another study, people watched videotaped interviews. If told the interviewees were job applicants, the viewers perceived them as normal (Langer & Abelson, 1974, 1980). Other viewers who were told they were watching psychiatric or cancer patients perceived the same interviewees as “different from most people.” Therapists who thought they were watching an interview of a psychiatric patient perceived him as “frightened of his own aggressive impulses,” a “passive, dependent type,” and so forth. As Rosenhan discovered, a label can have “a life and an influence of its own.” Labels matter.
Labels also have power outside the laboratory. Getting a job or finding a place to rent can be a challenge for people recently released from a mental hospital. Label someone as “mentally ill” and people may fear them as potentially violent (see Thinking Critically About: Are People With Psychological Disorders Dangerous?). Such negative reactions may fade as people better understand that many psychological disorders involve diseases of the brain, not failures of character (Solomon, 1996). Public figures have helped foster this understanding by speaking openly about their own struggles with disorders such as depression and substance abuse. The more contact we have with people with disorders, the more accepting our attitudes become (Kolodziej & Johnson, 1996).
THINKING CRITICALLY ABOUT
Are People With Psychological Disorders Dangerous?
40-
September 16, 2013, started like any other Monday at Washington, DC’s, Navy Yard, with people arriving early to begin work. Then government contractor Aaron Alexis parked his car, entered the building, and began shooting people. An hour later, 13 people were dead, including Alexis. Reports later confirmed that Alexis had a history of mental illness. Before the shooting, he had stated that an “ultra low frequency attack is what I’ve been subject to for the last three months. And to be perfectly honest, that is what has driven me to this.” After a horrifying mass shooting in a Connecticut elementary school in 2012, New York’s governor declared, “People who have mental issues should not have guns” (Kaplan & Hakim, 2013). These devastating mass shootings, like many others since then, reinforced public perceptions that people with psychological disorders pose a threat (Barry et al., 2013; Jorm et al., 2012). So did an incident in March of 2015, when Germanwings co-
Does scientific evidence support the governor’s statement? If disorders actually increase the risk of violence, then denying people with psychological disorders the right to bear arms might reduce violent crimes. But real life tells a different story. Most people with mental disorders commit no violent crimes, and the vast majority of violent crimes are committed by people with no diagnosed disorder (Fazel & Grann, 2006; Skeem et al., 2015; Walkup & Rubin, 2013).
People with disorders are more likely to be victims than perpetrators of violence (Marley & Bulia, 2001). According to the U.S. Surgeon General’s Office (1999, p. 7), “There is very little risk of violence or harm to a stranger from casual contact with an individual who has a mental disorder.” The bottom line: Psychological disorders only rarely lead to violent acts, and focusing gun restrictions only on mentally ill people will likely not reduce gun violence (Friedman, 2012).

If mental illness is not a good predictor of violence, what is? Better predictors are a history of violence, use of alcohol or drugs, and access to a gun. The mass-
Mental disorders seldom lead to violence, and clinical prediction of violence is unreliable. What, then, are the triggers for the few people with psychological disorders who do commit violent acts? For some, the trigger is substance abuse. For others, like the Navy Yard shooter, it’s threatening delusions and hallucinated voices that command them to act (Douglas et al., 2009; Elbogen & Johnson, 2009; Fazel et al., 2009, 2010). Whether people with mental disorders who turn violent should be held responsible for their behavior remains controversial. U.S. President Ronald Reagan’s near-
Which decision was correct? The first two, which blamed Loughner’s “madness” for clouding his judgment? Or the final one, which decided that he should be held responsible for the acts he committed? As we come to better understand the biological and environmental bases for all human behavior, from generosity to vandalism, when should we—

“What’s the use of their having names,” the Gnat said, “if they won’t answer to them?”
“No use to them,” said Alice; “but it’s useful to the people that name them, I suppose.”
Lewis Carroll, Through the Looking-
Despite their risks, diagnostic labels have benefits. They help mental health professionals communicate about their cases and study the causes and treatments of disorder. Clients are often relieved to learn that the nature of their suffering has a name, and that they are not alone in experiencing their symptoms.
 To test your ability to form diagnoses, visit LaunchPad’s PsychSim 6: Classifying Disorders.
To test your ability to form diagnoses, visit LaunchPad’s PsychSim 6: Classifying Disorders.
RETRIEVE IT
Question
What is the value, and what are the dangers, of labeling individuals with disorders?