44.7 Evaluating Psychotherapies
Many Americans have great confidence in psychotherapy’s effectiveness. “Seek counseling” or “Ask your mate to find a therapist,” advice columnists often advise. Before 1950, psychiatrists were the primary providers of mental health care. Today’s providers include clinical and counseling psychologists; clinical social workers; pastoral, marital, abuse, and school counselors; and psychiatric nurses. With such an enormous outlay of time as well as money and effort, it is important to ask: Are the millions of people worldwide justified in placing their hopes in psychotherapy?
Is Psychotherapy Effective?
44-
Asking whether psychotherapy has worked is not as simple as asking whether antibiotics have worked to treat an infection. So how can we assess psychotherapy’s effectiveness? By how we feel about our progress? By how our therapist feels about it? By how our friends and family feel about it? By how our behavior has changed?
CLIENTS’ PERCEPTIONS If clients’ testimonials were the only measuring stick, we could strongly assert psychotherapy’s effectiveness. Consider the 2900 Consumer Reports readers who reported on their experiences with mental health professionals (1995; Kotkin et al., 1996; Seligman, 1995). How many were at least “fairly well satisfied”? Almost 90 percent. Among those who recalled feeling fair or very poor when beginning therapy, 9 in 10 now were feeling very good, good, or at least so-
But client testimonials don’t persuade everyone. Critics note reasons for skepticism:
People often enter therapy in crisis. When, with the normal ebb and flow of events, the crisis passes, people may assume their improvement was a result of the therapy. Depressed people often get better no matter what they do.
Clients believe that treatment will be effective. The placebo effect is the healing power of positive expectations.
Clients generally speak kindly of their therapists. Even if the problems remain, clients “work hard to find something positive to say. The therapist had been very understanding, the client had gained a new perspective, he learned to communicate better, his mind was eased, anything at all so as not to have to say treatment was a failure” (Zilbergeld, 1983, p. 117).
Clients want to believe the therapy was worth the effort. People may feel the need to justify their investment of money, time, and hope.

CLINICIANS’ PERCEPTIONS If clinicians’ perceptions were proof of therapy’s effectiveness, we would have even more reason to celebrate. Case studies of successful treatment abound. Furthermore, therapists are like the rest of us. They treasure compliments from clients saying good-
OUTCOME RESEARCH How, then, can we objectively assess psychotherapy’s effectiveness? What outcomes can we expect—
 To test your own therapeutic listening skills, visit LaunchPad’s Assess Your Strengths self-
To test your own therapeutic listening skills, visit LaunchPad’s Assess Your Strengths self-
In search of answers, psychologists have turned to controlled research. This is a well-
In the twentieth century, psychology, with its many different therapy options, faced a similar challenge. British psychologist Hans Eysenck (1952) launched a spirited debate when he summarized 24 studies of psychotherapy outcomes. He found that two-
Why, then, are we still debating psychotherapy’s effectiveness? Because Eysenck also reported similar improvement among untreated persons, such as those who were on waiting lists for treatment. With or without psychotherapy, he said, roughly two-
An avalanche of criticism greeted Eysenck’s conclusions. Some pointed out errors in his analyses. Others noted that he based his ideas on only 24 studies. Now, more than a half-
Therapists welcomed the first meta-
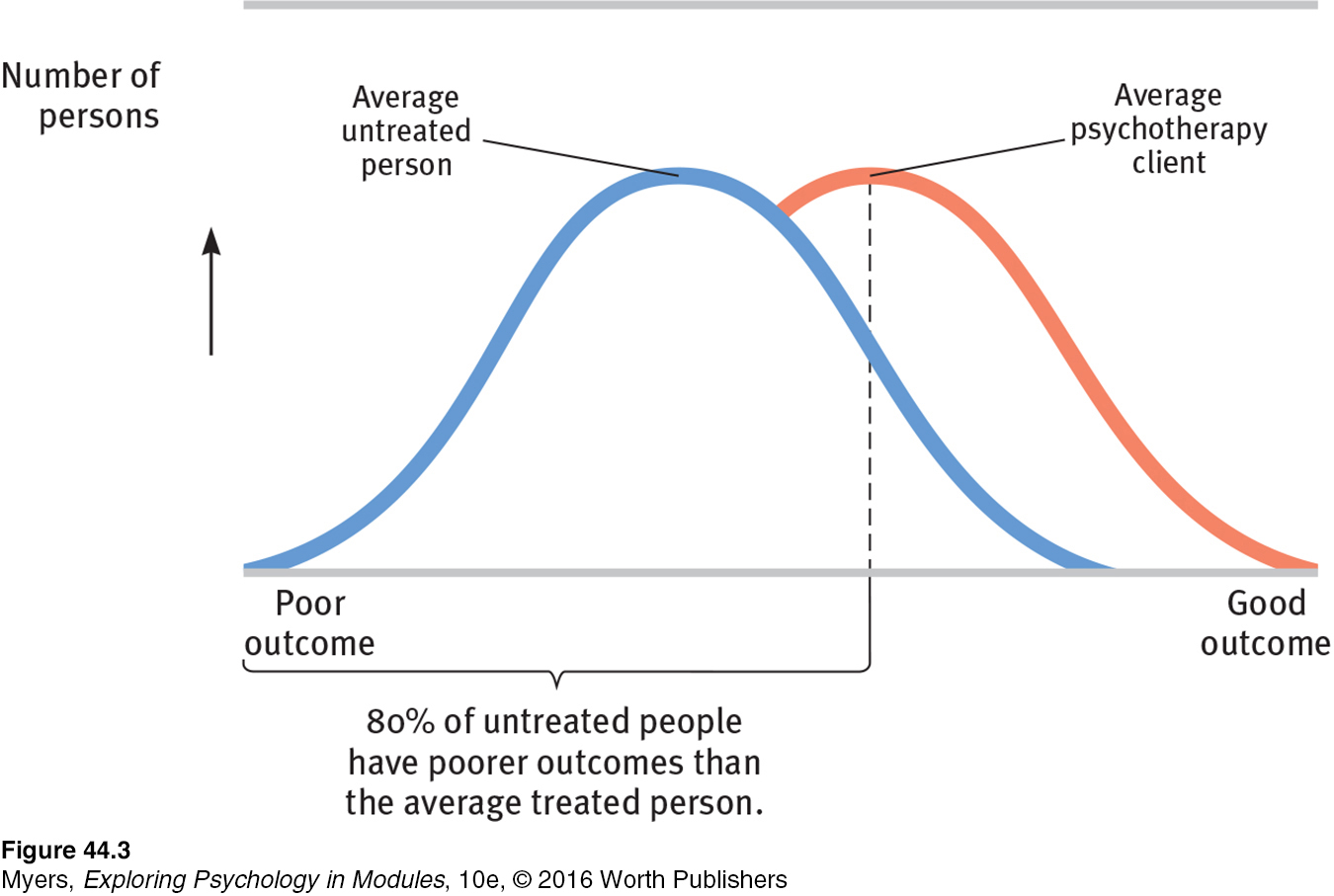
Dozens of subsequent summaries have now examined psychotherapy’s effectiveness. Their verdict echoes the results of the earlier outcome studies: Those not undergoing therapy often improve, but those undergoing therapy are more likely to improve, and to improve more quickly and with less risk of relapse. Moreover, between the treatment sessions for depression and anxiety, many people experience sudden symptom reductions. Those “sudden gains” bode well for long-
Is psychotherapy also cost-
But note that the claim—
RETRIEVE IT
Question
How might the placebo effect bias clients' and clinicians' appraisals of the effectiveness of psychotherapies?
Which Psychotherapies Work Best?
44-
The early statistical summaries and surveys did not find that any one type of psychotherapy is generally better than others (Smith et al., 1977, 1980). Later studies have similarly found little connection between clients’ outcomes and their clinicians’ experience, training, supervision, and licensing (Luborsky et al., 2002; Wampold, 2007). A Consumer Reports survey illustrated this point by asking: Were clients treated by a psychiatrist, psychologist, or social worker? Were they seen in a group or individual context? Did the therapist have extensive or relatively limited training and experience? It didn’t matter. Clients seemed equally satisfied (Seligman, 1995).
“Whatever differences in treatment efficacy exist, they appear to be extremely small, at best.”
Bruce Wampold et al. (1997)
So, was the dodo bird in Alice in Wonderland right: “Everyone has won and all must have prizes”? Not quite. Some forms of therapy get prizes for effectively treating particular problems. Behavioral conditioning therapies have had especially good results with specific behavior problems, such as bed-
Moreover, we can say that therapy is most effective when the problem is clear-
“Different sores have different salves.”
English proverb
But no prizes—
As with some medical treatments, it’s possible for psychological treatments to be not only ineffective but also harmful—
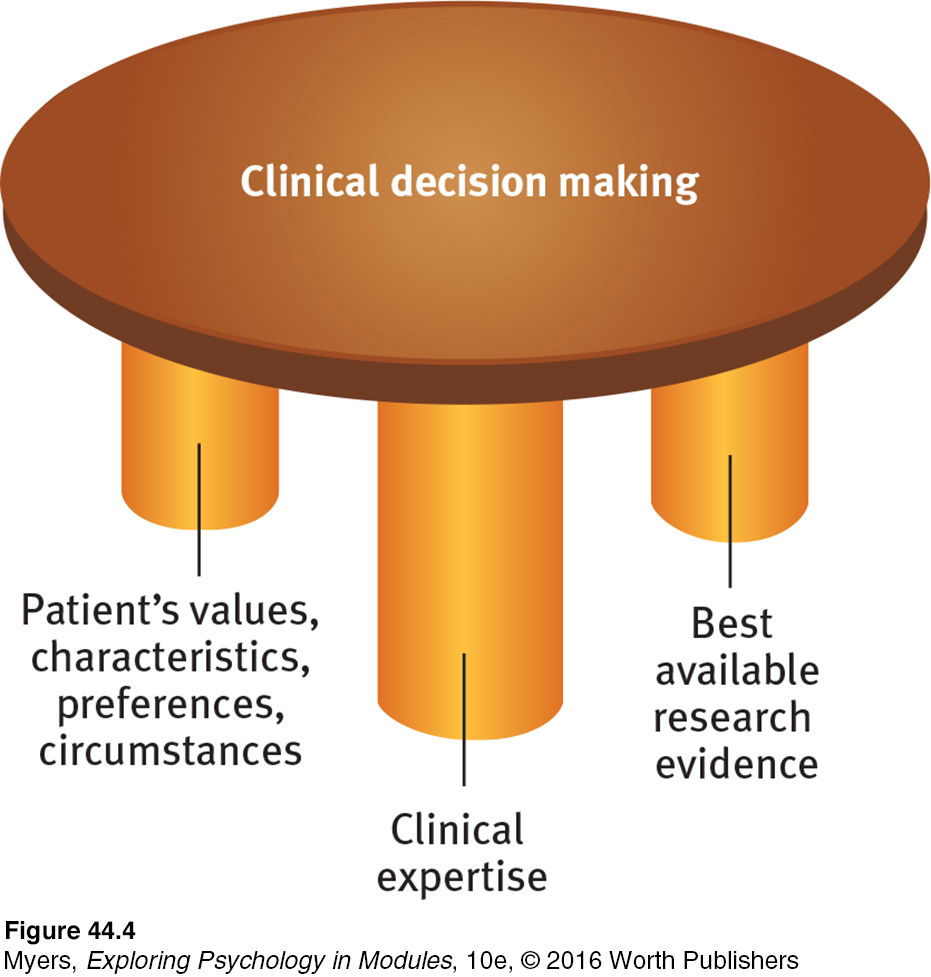
The evaluation question—
evidence-based practice clinical decision making that integrates the best available research with clinical expertise and patient characteristics and preferences.
Between these two factions stand the science-
RETRIEVE IT
Question
Therapy is most likely to be helpful for those with problems that
(are/are not) well-
Evaluating Alternative Therapies
44-
The tendency of many abnormal states of mind to return to normal, combined with the placebo effect (the healing power of mere belief in a treatment), creates fertile soil for pseudotherapies. Bolstered by anecdotes, boosted by the media, and broadcast on the Internet, alternative therapies—
Proponents of alternative therapies often feel that their personal testimonials are evidence enough. But how well do these therapies stand up to scientific scrutiny? There is little evidence for or against most of them. Some, however, have been the subject of controlled research. Let’s consider two. As we do, remember that sifting sense from nonsense requires the scientific attitude: being skeptical but not cynical, open to surprises but not gullible.
EYE MOVEMENT DESENSITIZATION AND REPROCESSING EMDR (eye movement desensitization and reprocessing) is a therapy adored by thousands and dismissed by thousands more as a sham—
Psychologist Francine Shapiro (1989, 2007, 2012) developed EMDR while walking in a park and observing that anxious thoughts vanished as her eyes spontaneously darted about. Back in the clinic, she had people imagine traumatic scenes while she triggered eye movements by waving her finger in front of their eyes, supposedly enabling them to unlock and reprocess previously frozen memories. Tens of thousands of mental health professionals from more than 75 countries have since undergone training (EMDR, 2011). No new therapy has attracted so many devotees so quickly since Franz Anton Mesmer introduced hypnosis (then called animal magnetism) more than two centuries ago (also after feeling inspired by an outdoor experience).
Does EMDR work? Shapiro believes it does, and she cites four studies in which it worked for 84 to 100 percent of single-
“Studies indicate that EMDR is just as effective with fixed eyes. If that conclusion is right, what’s useful in the therapy (chiefly behavioral desensitization) is not new, and what’s new is superfluous.”
Harvard Mental Health Letter, 2002
Why, wonder the skeptics, would rapidly moving one’s eyes while recalling traumas be therapeutic? Some argue that the eye movements relax or distract patients, thus allowing memory-
LIGHT EXPOSURE THERAPY Have you ever found yourself oversleeping, gaining weight, and feeling lethargic during the dark mornings and overcast days of winter? Slowing down and conserving energy during the cold, barren winters likely gave our distant ancestors a survival advantage. For people today, however—

Was light exposure a bright idea, or another dim-
RETRIEVE IT
Question
What is evidence-
Question
Which of the following alternative therapies HAS shown promise as an effective treatment?
| A. |
| B. |
| C. |
| D. |
How Do Psychotherapies Help People?
44-
How can it be that therapists’ training and experience do not seem to influence clients’ outcomes? The answer seems to be that all psychotherapies offer three basic benefits (Frank, 1982; Goldfried & Padawer, 1982; Strupp, 1986; Wampold 2001, 2007).
 To test your own levels of hopefulness, visit LaunchPad’s Assess Your Strengths self-
To test your own levels of hopefulness, visit LaunchPad’s Assess Your Strengths self-
HOPE FOR DEMORALIZED PEOPLE People seeking therapy typically feel anxious, depressed, self-
A NEW PERSPECTIVE LEADING TO NEW BEHAVIORS Every psychotherapy offers people an explanation of their symptoms. Therapy is a new experience that can help people change their behaviors and their views of themselves. Armed with a believable fresh perspective, they may approach life with new energy.
therapeutic alliance a bond of trust and mutual understanding between a therapist and client, who work together constructively to overcome the client’s problem.
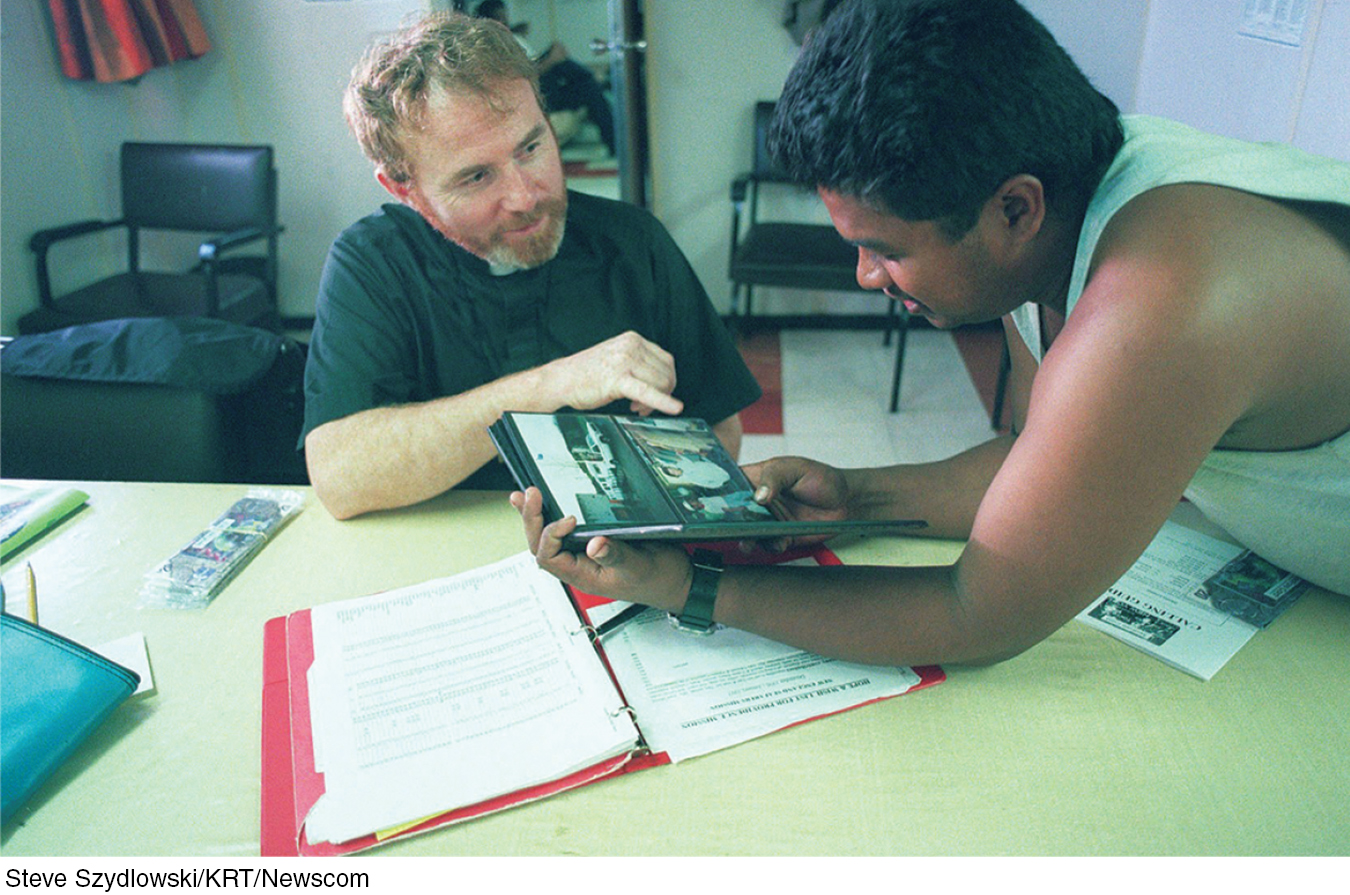
AN EMPATHIC, TRUSTING, CARING RELATIONSHIP No matter what technique they use, effective psychotherapists are empathic. They seek to understand people’s experience. They communicate care and concern. And they earn trust through respectful listening, reassurance, and guidance. These qualities were clear in recorded therapy sessions from 36 recognized master therapists (Goldfried et al., 1998). Some took a cognitive-
That all psychotherapies offer hope through a fresh perspective provided by a caring person is what also enables paraprofessionals (briefly trained caregivers) to assist so many troubled people so effectively (Christensen & Jacobson, 1994). These three common elements are also part of what the growing numbers of self-
* * *
To recap, people who seek help usually improve. So do many of those who do not undergo psychotherapy, and that is a tribute to our human resourcefulness and our capacity to care for one another. Nevertheless, though the therapist’s orientation and experience appear not to matter much, people who receive some psychotherapy usually improve more than those who do not. People with clear-
RETRIEVE IT
Question
Those who undergo psychotherapy are (more/less) likely to show improvement than those who do not undergo psychotherapy.
Culture and Values in Psychotherapy
44-
All psychotherapies offer hope. Nearly all psychotherapists attempt to enhance their clients’ sensitivity, openness, personal responsibility, and sense of purpose (Jensen & Bergin, 1988). But therapists also differ from one another and may differ from their clients (Delaney et al., 2007; Kelly, 1990).
These differences can create a mismatch when a therapist from one culture interacts with a client from another. In North America, Europe, and Australia, for example, many therapists reflect the majority culture’s individualism, which often gives priority to personal desires and identity. Clients with a collectivist perspective, as with many from Asian cultures, may assume people will be more mindful of others’ expectations. These clients may have trouble relating to therapies that require them to think only of their own well-
Such differences help explain minority populations’ reluctance to use mental health services, and their tendency to prematurely terminate therapy (Chen et al., 2009; Sue, 2006). In one experiment, Asian-
Therapist and client may also have differing religious perspectives. Highly religious people may prefer and benefit from religiously similar therapists (Masters, 2010; Smith et al., 2007; Wade et al., 2006). They may have trouble establishing an emotional bond with a therapist who does not share their values. People living in “cultures of honor”—which prize being strong and tough—
Finding a Mental Health Professional
44-
Life for everyone is marked by a mix of serenity and stress, blessing and bereavement, good moods and bad. So, when should we seek a mental health professional’s help? The American Psychological Association offers these common trouble signals:
Feelings of hopelessness
Deep and lasting depression
Self-
destructive behavior, such as substance abuse Disruptive fears
Sudden mood shifts
Thoughts of suicide
Compulsive rituals, such as hand washing
Sexual difficulties
Hearing voices or seeing things that others don’t experience
In looking for a therapist, you may want to have a preliminary consultation with two or three. College health centers are generally good starting points, and may offer some free services. You can describe your problem and learn each therapist’s treatment approach. You can ask questions about the therapist’s values, credentials (TABLE 44.3), and fees. And you can assess your own feelings about each of them. The emotional bond between therapist and client is perhaps the most important factor in effective therapy.
Therapists and Their Training
| Type | Description |
|---|---|
| Clinical psychologists | Most are psychologists with a Ph.D. (includes research training) or Psy.D. (focuses on therapy) supplemented by a supervised internship and, often, postdoctoral training. About half work in agencies and institutions, half in private practice. |
| Psychiatrists | Psychiatrists are physicians who specialize in the treatment of psychological disorders. Not all psychiatrists have had extensive training in psychotherapy, but as M.D.s or D.O.s they can prescribe medications. Thus, they tend to see those with the most serious problems. Many have their own private practice. |
| Clinical or psychiatric social workers | A two- |
| Counselors | Marriage and family counselors specialize in problems arising from family relations. Clergy provide counseling to countless people. Abuse counselors work with substance abusers and with spouse and child abusers and their victims. Mental health and other counselors may be required to have a two- |