Chapter 1. CARDIOVASCULAR SYSTEM
Objectives
After completing this unit, you should be able to:
- Describe the functions of the cardiovascular system. Trace the pathway of blood through the heart and around the pulmonary circulation and systemic circulation.
- Name the four chambers of the heart and identify the great vessels associated with each chamber. Name the major branches of the coronary arteries and describe their distribution. Define the fibrous endoskeleton of the heart. Identify the heart valves and describe their location, function, and how they operate.
- Describe the structural and functional properties of cardiac muscle. Name the components of the conduction system of the heart, and trace the conduction pathway of the electrical activity. Identify the individual waves and intervals of the electrocardiogram (EKG) and indicate what each represents.
- Explain the factors involved in control of stroke volume and heart rate. Describe normal heart sounds and their sources, and explain how heart murmurs differ from normal sounds.
- Describe the structure and function of an artery and a vein. Describe the function of each of the three layers that form the wall of a blood vessel. Describe the function of the three types of arterial blood vessels (elastic artery, muscular artery, and arteriole).
- Define blood pressure, blood flow, and resistance. Explain the relationship between these three factors. Define vasoconstriction and vasodilation, and list factors that influence arteriole diameter.
- Define systolic and diastolic blood pressure. Explain how blood pressure is measured and the mean arterial pressure is calculated. Describe the factors that influence arterial blood pressure (heart rate, stroke volume, cardiac output, blood volume, peripheral resistance, viscosity). Describe how blood pressure is regulated.
- Describe the factors that facilitate venous return of blood to the heart (venous valves, skeletal muscle, ventilation, and capacitance).
- Identify the vessels of the microcirculation and explain the function of the arteriole, capillary, and venule. Identify the types of capillary networks on the basis of permeability. Describe the factors involved with filtration and reabsorption.
Introduction
The cardiovascular system consists of a muscular pump, the heart, and a series of interconnected tubes called blood vessels. The heart pumps blood throughout the blood vessels or vasculature to provide O2 and nutrients to metabolically active tissue and remove CO2 and other metabolic wastes. In addition, circulation of blood assists with thermoregulation so that if the body is too warm, blood flow increases to the skin for evaporative cooling. If the body is too cool, blood is shunted away from surface blood vessels to conserve heat in the torso. The heart is centrally located in the thoracic cavity beneath the sternum. It is surrounded by a fibrous connective tissue capsule, the pericardium, which serves to loosely anchor the heart in the thoracic cavity. The inner surface of the pericardium is lined by a serous membrane which secretes serous fluid to act as a lubricant to reduce friction at the surface of the beating heart. Inflammation of the serous membrane leads to pericarditis and excess fluid surrounding the heart. In severe cases of pericarditis or if superficial blood vessels of the heart are damaged and leak blood, the heart may be limited in its contraction due to compression by the excess fluid leading to cardiac tamponade.
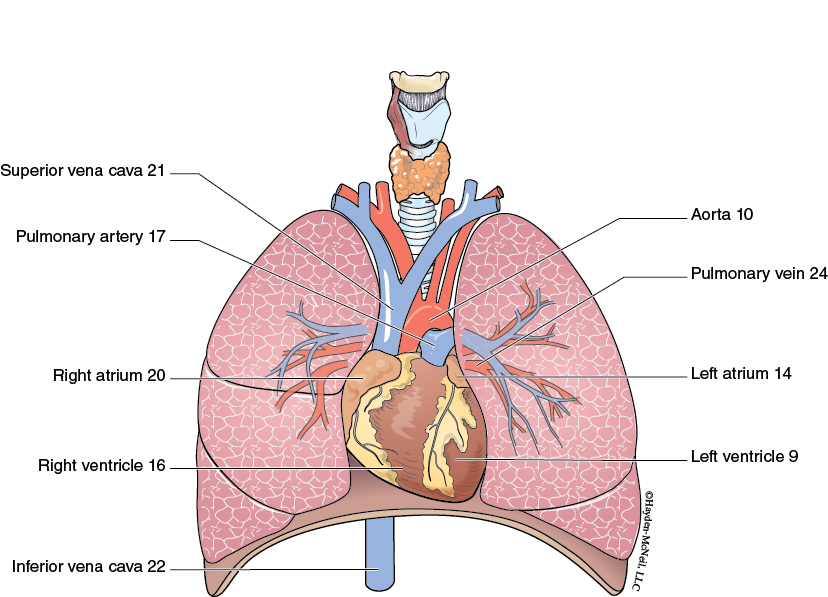
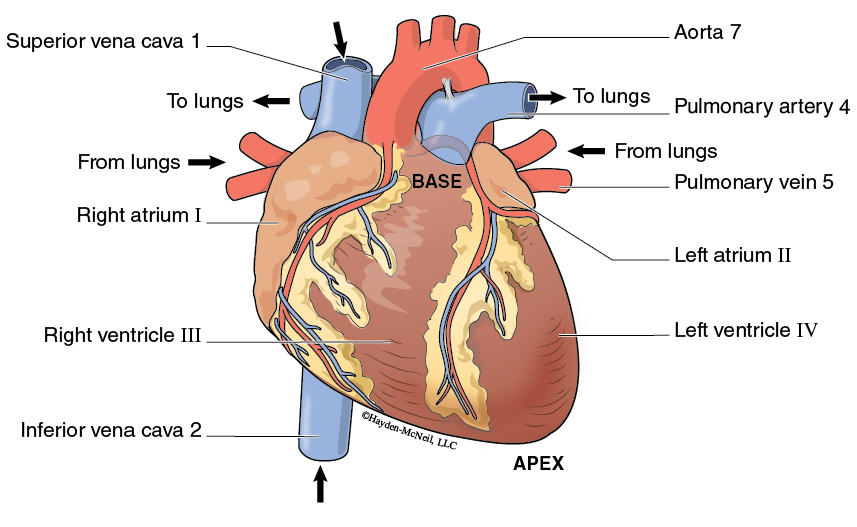
The heart is internally separated into four chambers associated with the major blood vessels of the body. The upper chambers, considered the base of the heart, are the thinner walled atria which receive blood from the lower pressure venous system. The lower chambers, considered the apex of the heart, are the thicker walled ventricles and they pump blood into the higher pressure arterial system. Blood vessels are classified as arteries if they transport blood away from the heart and veins if they transport blood to the heart. The definition of arteries and veins does not depend on whether the blood is oxygenated and bright red in color, or deoxygenated and brick red in color.
Blood Pressure
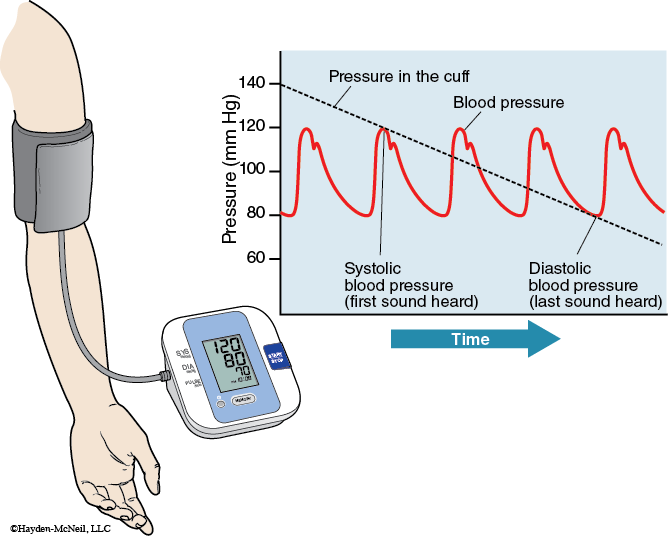
Blood pressure can be measured with a blood pressure cuff (sphygmomanometer) that occludes the brachial artery or radial artery while listening for characteristic Korotkoff sounds with a stethoscope as the pressure is released. Normal unrestricted blood flow has a smooth laminar arrangement in the artery and would be silent. Restricted blood flow through narrow openings causes turbulent flow and vibrates the artery to generate sound. The blood pressure cuff is inflated above the systolic pressure, the highest arterial pressure, and collapses the artery. As the cuff is subsequently deflated to the systolic pressure, blood can squirt through the constricted artery in a turbulent manner generating a snapping sound. This first sound corresponds to the systolic pressure. As the cuff is further deflated, the snapping sound becomes louder and longer as the vessel allows turbulent blood flow for a longer period of time. As the diastolic pressure, the lowest arterial pressure, is approached, the sound becomes muffled to silent as the blood flow returns to a laminar flow in the unrestricted artery. This quieting of the Korotkoff sound corresponds to the diastolic pressure.
Hypertension is an abnormally high blood pressure measured consistently in the individual. Hypertension contributes to the thickening of blood vessels called atherosclerosis. The higher pressure than normal may also contribute to development of an aneurysm or weakening of the blood vessel wall. Also, hypertension puts a greater demand on heart muscle to forcefully contract to pump blood out of the ventricle which increases the risk for a myocardial infarction or heart attack. Hypotension is an abnormally low blood pressure. This is problematic if the low blood pressure is insufficient to force blood to the brain against the force of gravity and the individual becomes dizzy or faints.
Heart Chambers
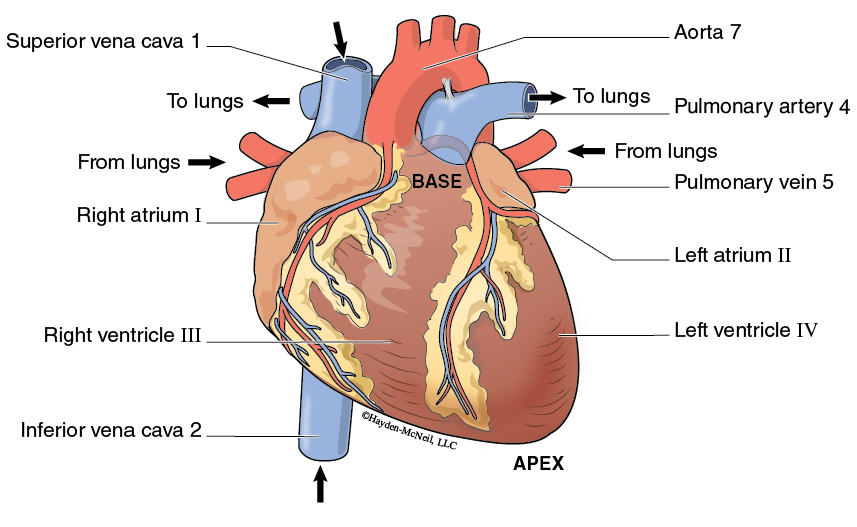
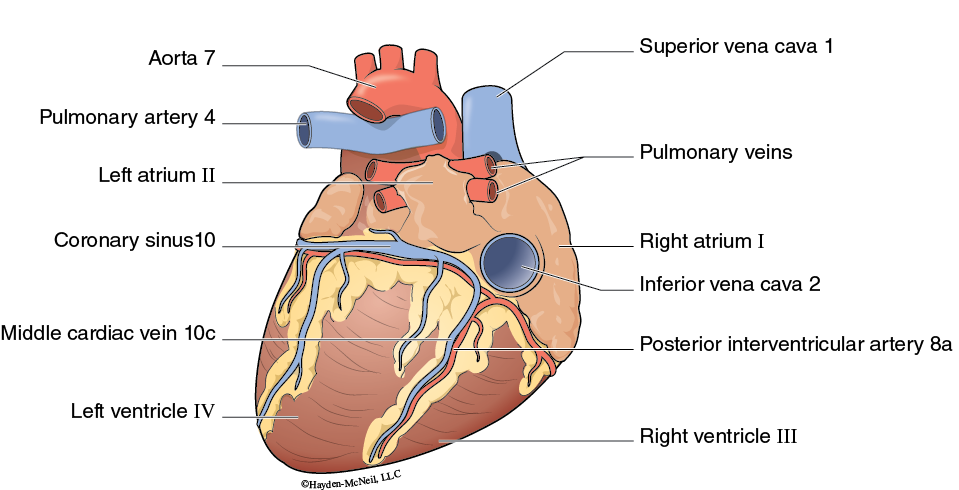
Examining the chambers of the heart reveals the thinner walled atria located at the base of the heart. The right atrium receives blood from the tissues of the body through two large veins. The superior vena cava drains the body superior to the diaphragm and the inferior vena cava drains blood from the body inferior to the diaphragm. The left atrium receives blood returning from the lungs through the pulmonary veins. The pulmonary veins will appear red in color due to the blood returning from the lungs being well oxygenated. The ventricles are thicker walled chambers associated with the apex of the heart. The right ventricle pumps blood out through the pulmonary artery to the lungs for oxygenation and removal of CO2. The pulmonary artery will appear blue in color due to the blood being deoxygenated. The left ventricle is the thickest walled chamber and pumps blood out through the aorta to provide oxygen and nutrients throughout the body in the systemic circulation.
Coronary Circulation
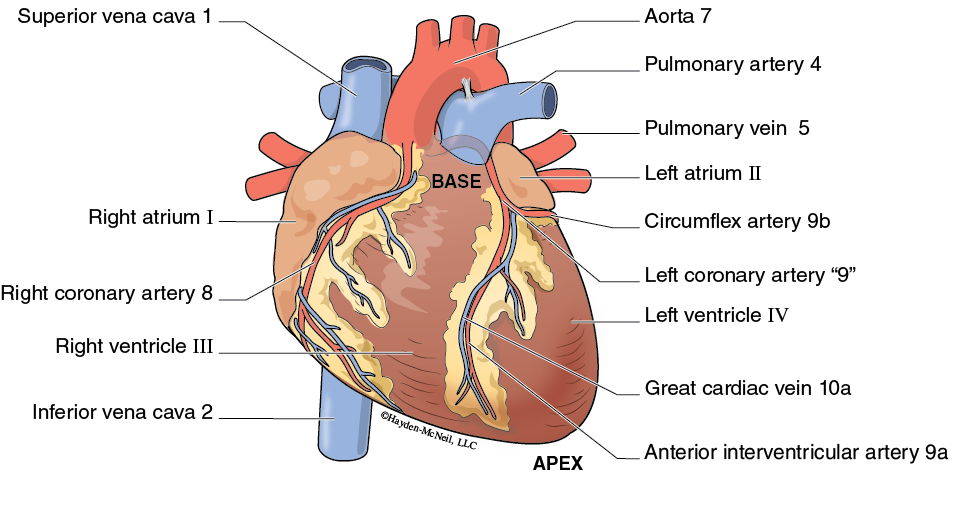
Cardiac muscle is very metabolically active and requires aerobic metabolism to generate ATP at a level to maintain rhythmic muscular contractions. The coronary circulation is the blood vessels associated with providing oxygen and nutrients to the cardiac muscle of the heart. Both the right and left coronary arteries branch off the aorta early, just distal to the aortic valve. The right coronary artery continues along the atrial margin between the right atrium and right ventricle to the posterior surface. At the posterior surface, the posterior interventricular artery branches off toward the apex. On the left side, the left coronary artery branches early with the anterior interventricular artery proceeding inferiorly between the right and left ventricles and the circumflex artery coursing between the left atrium and left ventricle. Two of the largest cardiac veins providing venous return from cardiac muscle are the great cardiac vein draining the anterior surface and the middle cardiac vein draining the posterior surface. They converge at the coronary sinus. Most cardiac veins drain into the coronary sinus which returns blood to the right atrium.
Coronary artery disease is an inadequate O2 supply to the heart due to vascular spasm or development of vessel blockage. Temporary reduction in blood flow is manifested as angina pectoris, chest pains associated with inadequate oxygen for the metabolic demands of the heart. This occurs most often during increased physical activity like weekend sports, doing yard work, or shoveling snow. Severe deprivation of blood flow results in a myocardial infarction, commonly known as a heart attack. The cardiac muscle dies and is replaced by scar tissue which is not electrically responsive and does not contract. Diagnostic tests for coronary artery disease include a holter monitor for recording the electrical activity over 24 hours and an exercise stress test to measure the electrical activity and blood pressure during various levels of exercise. Indications of coronary disease may be further investigated with a coronary angiogram. This involves the insertion of a flexible catheter into the femoral artery which is threaded up into the coronary arteries. A radiopaque substance is injected and a series of x-ray images are obtained as the substance flows through the coronary vessels to reveal any narrowing or blockage. Depending on the extent of the narrowing or blockage, transluminal angioplasty may restore circulation by inflating a balloon to compress the blockage. Generally, a flexible stent is inserted to help maintain an open coronary artery. If the blockage is too extensive or not easily reached by a catheter, coronary bypass surgery may be utilized. This procedure involves removing the great saphenous vein and suturing sections of it from the aorta to sites distal to the blockage on the coronary vessel. Quadruple bypass surgery means four blockage sites had to be bypassed by separate pieces of blood vessel.
Coronary Circulation
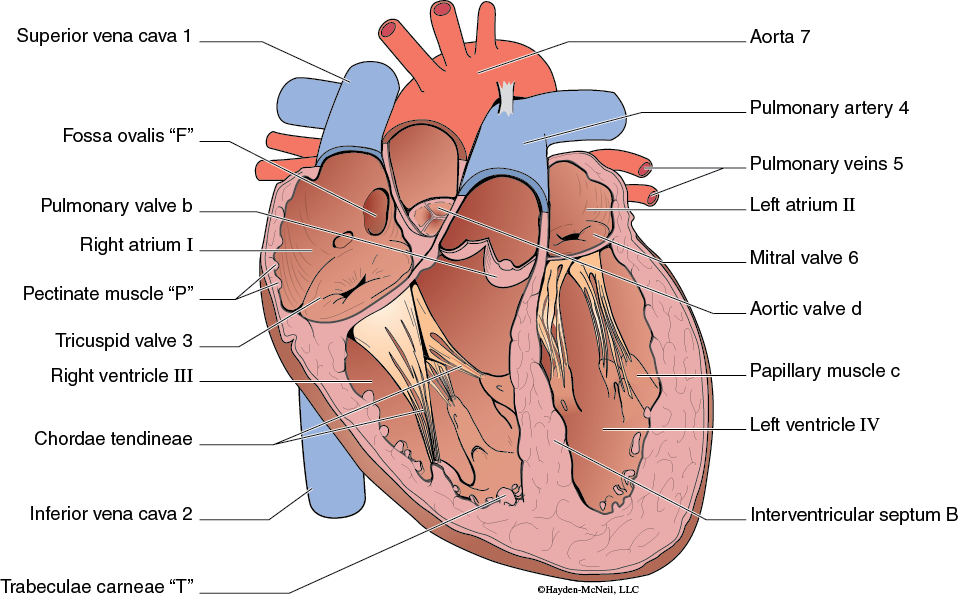
The fibrous endoskeleton is the dense connective tissue framework of four interconnected rings within the heart. This structure physically and electrically separates the atria from the ventricles. The cardiac muscle attaches to the fibrous endoskeleton so that the atria contract inferiorly toward the endoskeleton and the ventricles contract superiorly toward the endoskeleton. The four heart valves attach to the individual rings of the fibrous endoskeleton to allow for the one way flow of blood through the heart.
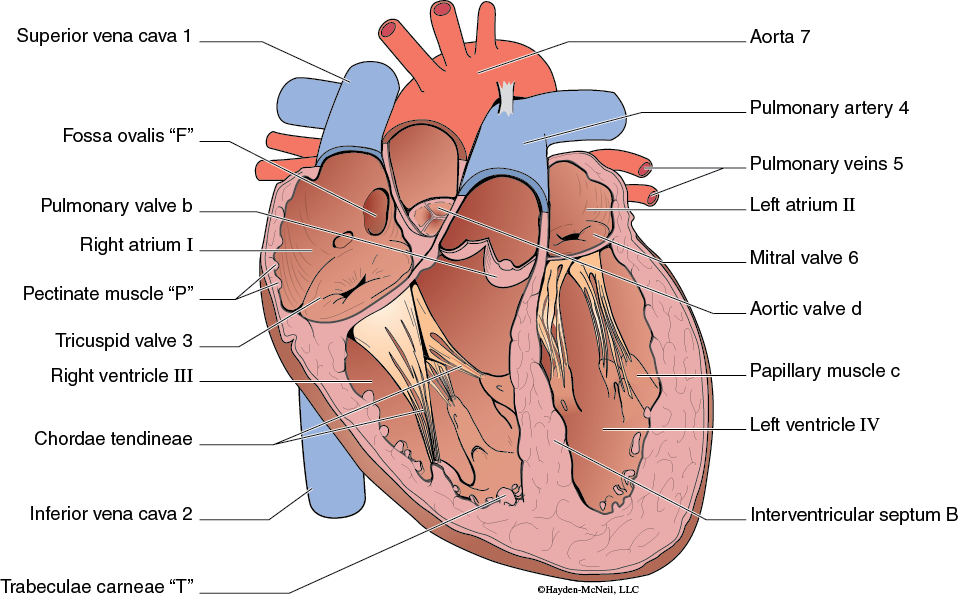
A frontal section exposes the internal structure of the heart for examination. The wall of the atria contains ridges of cardiac muscle called pectinate muscle. This muscle allows the atria to more easily distend before an atrial contraction. The fossa ovalis represents the remnants of a hole between the right and left atria that is present during fetal development. A connective tissue flap seals this opening during the first few weeks of life after birth. The much thicker ventricles also exhibit ridges of cardiac muscle called trabeculae carneae allowing for greater contraction strength without enormously thick walls. The interventricular septum is the muscular wall separating the two ventricles and is more associated with generating pressure in the left ventricle.
Coronary Circulation
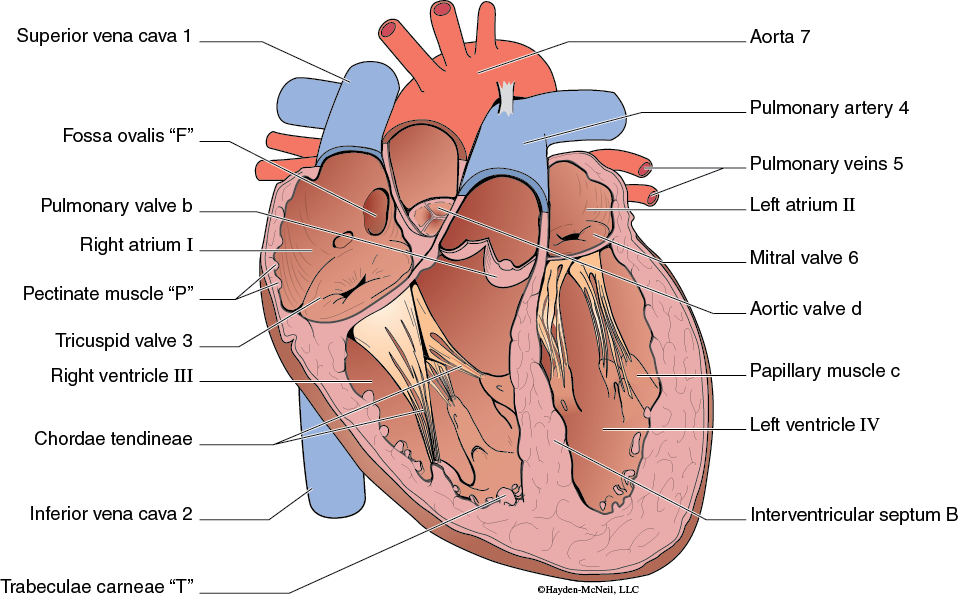
The heart has two sets of valves to assist with directing blood flow in the appropriate direction through the heart. The atrioventricular valves are the one way valves separating the atria from their corresponding ventricle. The tricuspid valve allows blood flow from the right atrium to the right ventricle but prevents blood flow back into the right atrium when the right ventricle contracts. Similarly on the left side of the heart, the mitral valve allows blood flow from the left atrium into the left ventricle but prevents the retrograde flow during ventricular contraction. Both of the atrioventricular valves have papillary muscle attached to the valve cusps by chordae tendineae. During ventricular contraction, the papillary muscle also contracts to help to keep the atrioventricular valves closed as pressure rises within the ventricle. The semilunar valves are located between the ventricles and their corresponding arteries. The pulmonary valve prevents blood flow back into the right ventricle from the pulmonary artery as the right ventricle relaxes. The aortic valve prevents the return of blood from the aorta when the left ventricle relaxes. In both cases, the semilunar valve closes due to blood filling the pouch-like valve cusps causing them to seal in the middle.
Coronary Circulation
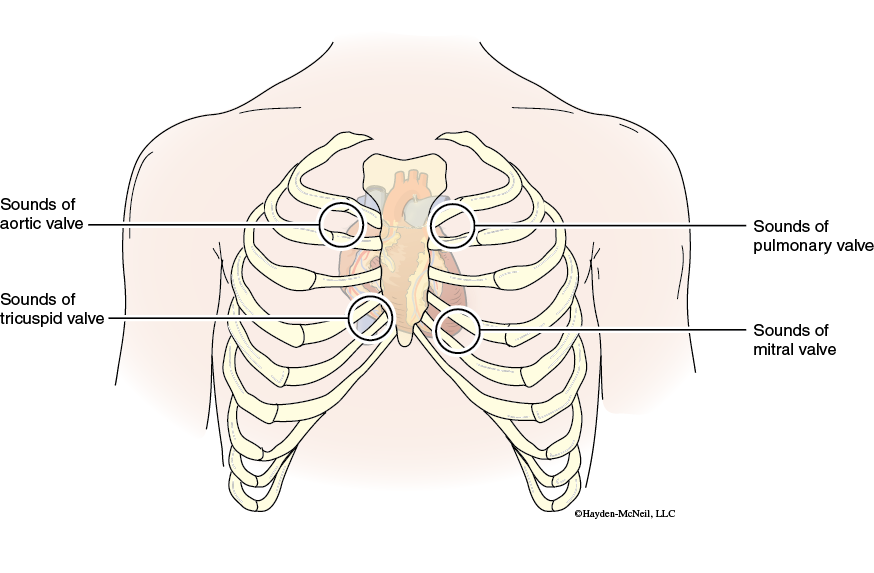
Closure of the atrioventricular valves and the semilunar valves can be assessed by listening to the lubb-dupp heart sounds with a stethoscope. The first heart sound (lubb) occurs with the closing of the atrioventricular valves. The second heart sound (dupp) corresponds to closing of the semilunar valves. A heart murmur, a swishing or gurgling sound, can occur with a defective heart valve that does not close and seal tightly. The regurgitation of blood in the opposite direction occurring with incompetent valves is detected as a muffled sound. Narrowed valve openings (valve stenosis) and septal defects altering normal blood flow can also produce heart murmurs. Echocardiography is an ultrasound technique that can map blood flow through the heart to determine the cause of a heart murmur and assess the extent of the inappropriate blood flow.
Exercise: Heart Sounds
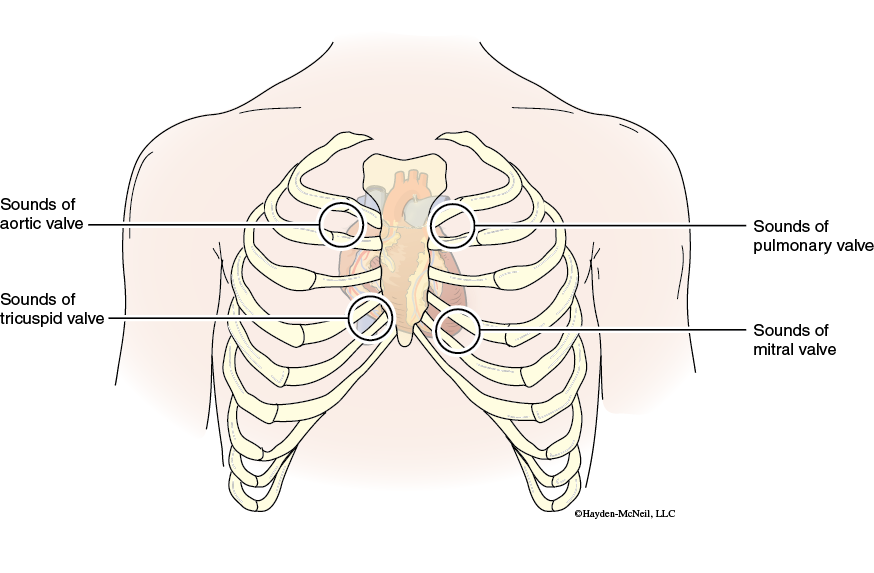
- Using a clean, disinfected stethoscope, listen to your first (lubb) sound by placing the diaphragm on the 5th intercostals space on the edge of the sternum.
- Listen to your second (dupp) sound by placing the diaphragm on the 2nd intercostals space on the edge of the sternum. Note the difference in the second sound compared to the first sound.
1.1 Circulation
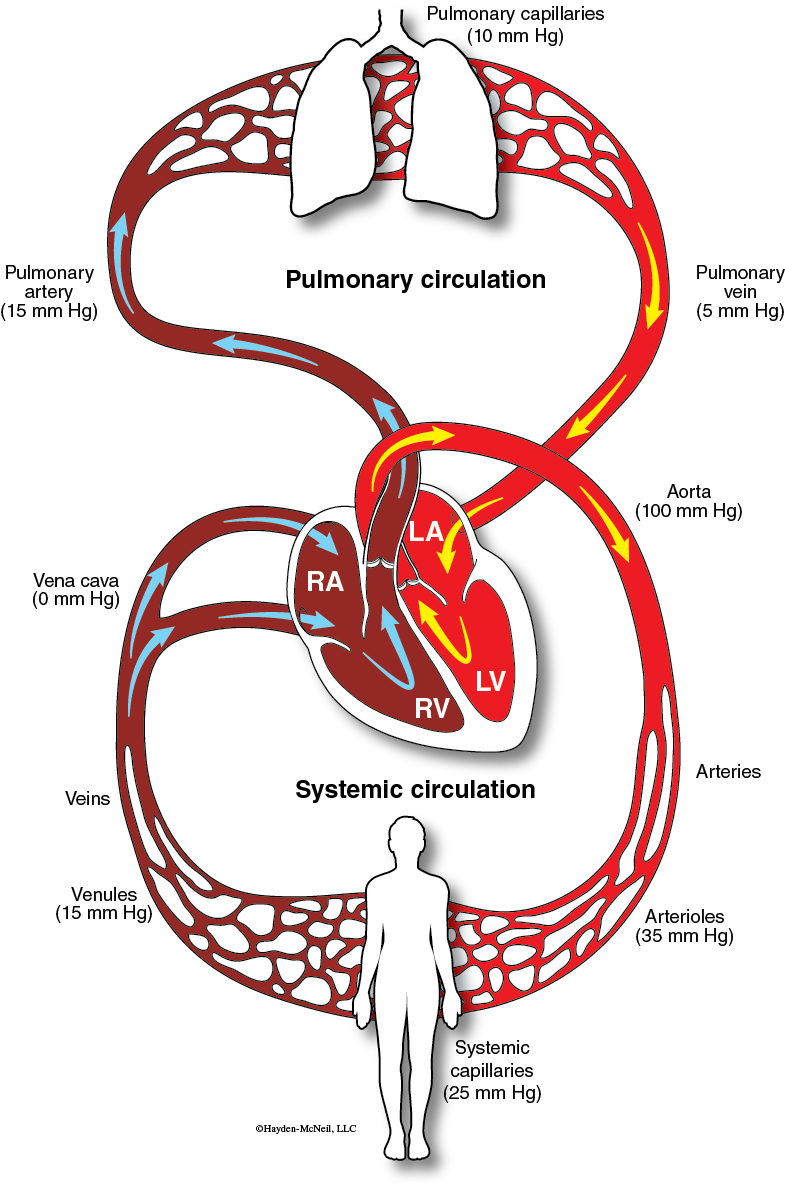
The heart subdivides the cardiovascular system into two separate but interconnected circulatory pathways. The pulmonary circulation is a lower pressure system between the right ventricle, pulmonary arteries, pulmonary veins, and left atrium. The systemic circulation is a higher pressure system that circulates blood from the left ventricle, out the aorta to distribute oxygen and nutrients to the tissues of the body. Blood is returned to the heart through the superior vena cava or inferior vena cava where it enters the right atrium.
Circulation of blood involves the heart pumping blood through a closed system of continuous blood vessels. If we begin with a quantity of blood in the right atrium, when the atria contract, this blood will be pumped past the tricuspid valve into the right ventricle to further top off the blood already there. The ventricles then contract and pressure in the right ventricle will close the tricuspid valve and open the pulmonary valve. The blood will flow into the pulmonary artery to the lungs where oxygen will be picked up and carbon dioxide is removed. When the right ventricle relaxes, the pulmonary valve will close and pressure will lower to the diastolic value. The blood returns from the lungs to the left atrium through the pulmonary veins. This may take several minutes from when we started to traverse through the pulmonary circulation. Now, when the atria again contract, the quantity of blood in the left atrium will be pumped past the mitral valve into the left ventricle to further top off the blood already there. The ventricles then contract and pressure in the left ventricle rapidly rises to close the mitral valve and open the aortic valve. The blood will flow into the aorta where it will be distributed throughout the body to provide oxygen and nutrients to the metabolically active tissue. When the left ventricle relaxes, the aortic valve will close and pressure will lower to the diastolic value. The blood returns to the right atrium through either the superior vena cava or inferior vena cava carrying carbon dioxide and other metabolic wastes from the tissues. This may take several minutes from when we started to traverse through the systemic circulation. The quantity of blood is now back again in the right atrium and we can follow the circulation again at the start of this paragraph.
Heart Electrical Activity
The heart is composed primarily of cardiac muscle forming the bulk of the atrial and ventricular wall (myocardium), epithelial tissue forming the smooth surface of the endocardium and serous membrane of the epicardium, and fibrous connective tissue forming the fibrous endoskeleton and heart valves. Most of the cardiac muscle exhibits striations and generate force through contractions of the myosin with actin like in skeletal muscle. A difference occurs with the source of the calcium ions to bind with troponin during excitation contraction coupling. In skeletal muscle, the calcium ions were released from the sarcoplasmic reticulum during an electrical impulse. Since cardiac muscle has a much smaller diameter than skeletal muscle, calcium ions involved in the contraction is not only released from a less developed sarcoplasmic reticulum, but also enters in from the interstitial fluid during an electrical impulse. In addition, cardiac cells are generally interconnected through specialized connections called intercalated discs. These discs physically and electrically connect adjacent cardiac cells so that the heart acts as a functional syncytium; it acts as a single unit. Either the cardiac muscle is excited and contracting or the cardiac muscle is not depolarizing and it is relaxed.
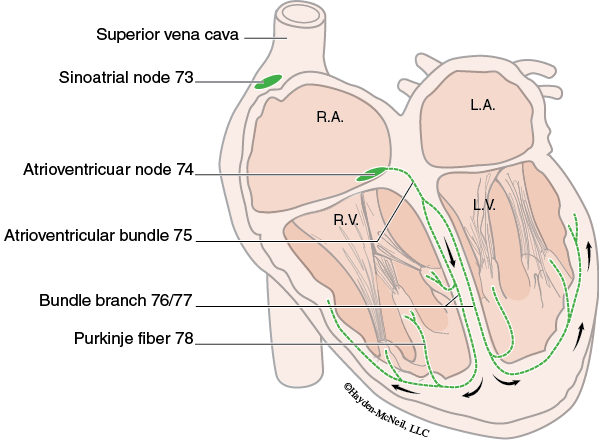
However, not all of the cardiac muscle has striations and is contractile myocardium. Approximately 1% of the cardiac muscle is specialized to form an electrical conduction system. This allows the heart to generate and conduct electrical impulses independent of the nervous system. This is quite different from skeletal muscle that requires motor neurons to generate electrical impulses in the muscle fiber. The specialized conduction system consists of the SA node, AV node, AV bundle, bundle branches, and purkinje fibers. The SA node is a collection of specialized myocardium located at the junction of the superior vena cava and right atrium. These cells exhibit a pacemaker potential showing spontaneous depolarization in a rhythmic manner. Consequently, the SA node is the primary pacemaker of the heart and serves to set the heart rhythm and rate. Electrical activity spreads through the right and left atrial cells due to intercalated discs. However, the fibrous endoskeleton prevents electrical activity from spreading directly from the atria to the ventricles. Instead, the AV node located in the inferior portion of the interatrial septum serves as the electrical connection between the atria and the ventricles. Activity through the AV node is relatively slow and adds a delay between excitation of the atria and subsequent excitation of the ventricles. This allows contraction of the atria to finish filling the ventricles before the ventricles are stimulated to contract. In addition, the AV node also exhibits diastolic depolarization but at a slower rate than the SA node. Therefore, the AV node acts as a secondary pacemaker for the heart if the SA node is unable to establish the heart rate. From electrical activity of the AV node, depolarization quickly spreads along the AV bundle and bundle branches through the interventricular septum. Purkinje fibers distributed extensively in the left and right ventricle finish the distribution of electrical activity throughout the ventricles to assist with an almost synchronous depolarization of the thick walled ventricles. This simultaneous depolarization of the ventricles generates the forceful contraction to eject blood into the aorta and pulmonary artery.
Even though the heart can beat and contract without nerve activity, neurons of the parasympathetic and sympathetic nervous system modify this intrinsic activity. The vagus nerve is the parasympathetic influence to the heart and it slows the heart rate and delays conduction through the AV node. The sympathetic nerves increase the heart rate and increase the contractility, the force of contraction at any muscle length.
Electrocardiogram (EKG)
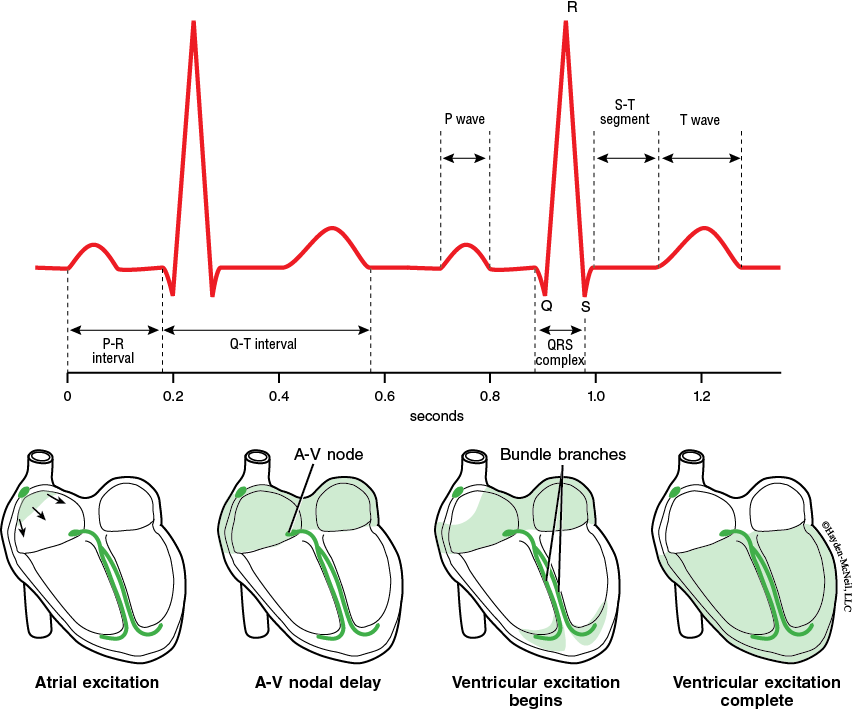
The electrical activity of the heart can be measured by placement of surface electrodes on the skin surrounding the heart in an electrocardiogram (EKG). Characteristic waves are labeled the P wave, QRS complex, and T wave and represent electrical activity of specific regions of the heart. The first wave is the P wave which represents depolarization of the atria. Generally, the right atrium is depolarized during the first portion of the P wave due to its proximity to the SA node and the left atrium is depolarized during the second portion of the P wave. The QRS complex measures depolarization of the ventricles and generally exhibits a high amplitude and short duration. This represents the activity of all the cardiac cells of the thick walled ventricles as well as the rapid spread through the ventricles because of the purkinje fibers. Because of the thickness of the ventricles, a T wave representing repolarization of the ventricles is also measured even though repolarization does not spread from cell to cell. Repolarization of the atria is not recorded in an EKG because the atria are thin walled with less cardiac cells, and the activity would occur during the QRS complex. The PR interval is the time delay between the onset of the P wave and the onset of the QRS complex. It measures the time required for the electrical activity to spread from the SA node to the ventricular cardiac cells, and generally lasts 0.16 s at rest. During exercise, a shorter PR interval will occur with a faster heart rate due to sympathetic activity accelerating conduction through the AV node. Heart block refers to a longer PR interval or even dropping a ventricular depolarization associated with the SA node. The ST segment occurs during the plateau phase of the electrical activity of the ventricles. Elevation or depression of the ST segment indicates ischemia of the ventricles occurring with coronary artery disease.
Electrocardiogram (EKG)
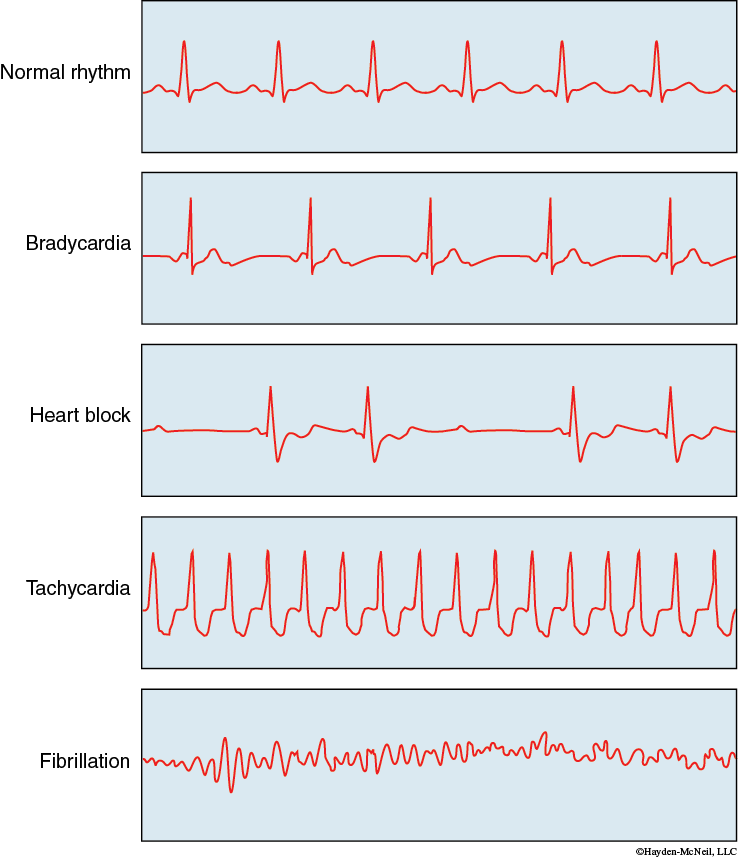
The EKG is a useful diagnostic tool in determining problems with electrical excitation and conduction of electrical activity in the heart. Cardiovascular disease remains the number one cause of death and the EKG represents a noninvasive means to measure heart function. Heart block occurs when the PR interval is prolonged or when every atrial depolarization does not result in a ventricular depolarization. Bradycardia is a resting heart rate slower than 50 bpm and may indicate a problem with activity of the SA node or even an AV node pacemaker. On the other hand, tachycardia is an extremely fast resting heart rate, generally greater than100 bpm. This may lead into ventricular fibrillation, an uncoordinated random activation of the ventricles leading to very weak contractions. Unless treated with electrical defibrillation, often by an automated external defibrillator (AED), death will occur rapidly because the ventricles are not generating pressure to maintain blood flow.
Blood vessels
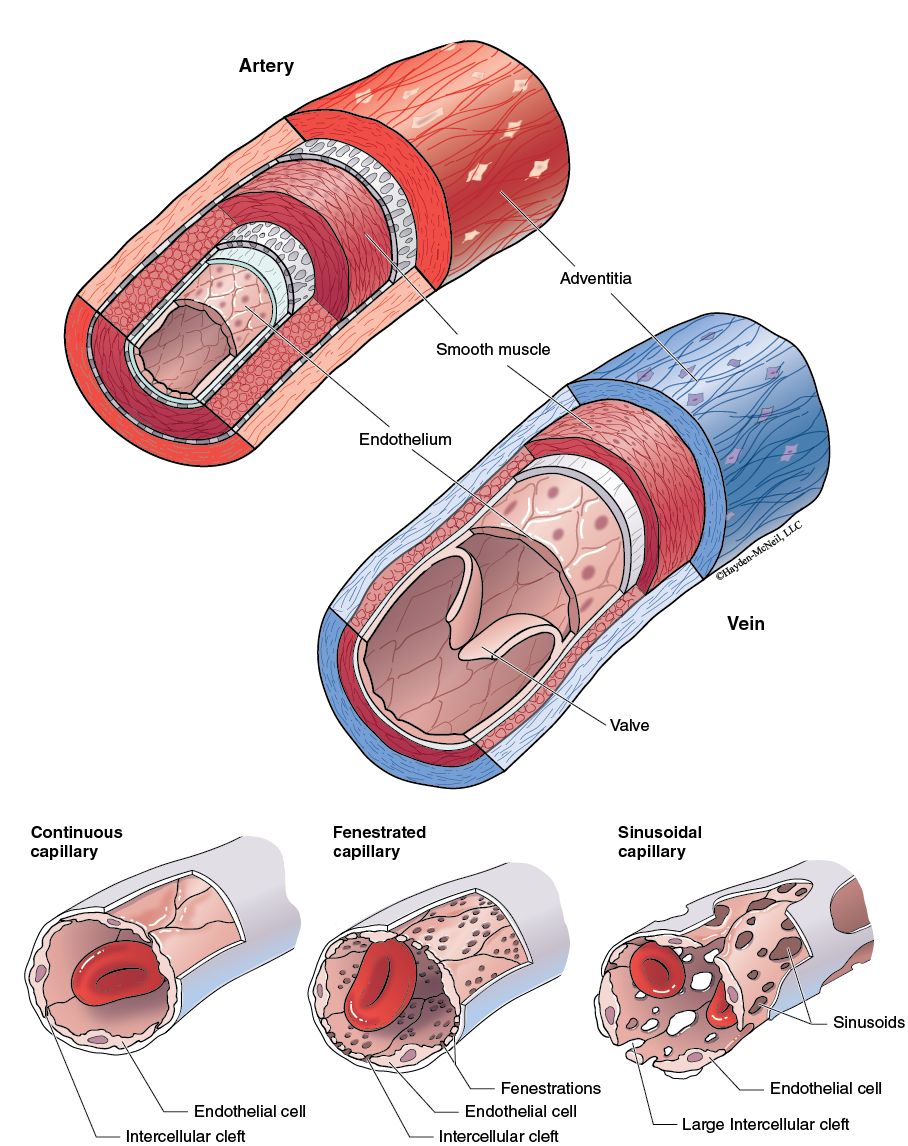
Blood vessels distribute blood flow to the lungs in the pulmonary circulation and throughout the body in the systemic circulation. The wall of arteries and veins consist of an adventitia with elastic connective tissue, smooth muscle in the middle layer, and a smooth endothelium because of simple squamous epithelium on the inner surfaces. Recall that a smooth endothelium helps prevent degranulation of platelets triggering development of a blood clot. The major blood vessels are classified as an artery if they carry blood away from the heart or a vein if they carry blood back to the heart. The vessel wall will be much thicker and contain more smooth muscle in an artery because of the high pressure of the blood within them generated by contraction of the ventricles. The aorta and its major branches are elastic arteries and have elastic connective tissue in the muscular layer and adventitia. During ventricular systole, the blood ejected from the heart will stretch the elastic tissue in these arteries. When the ventricles relax, the diastolic pressure does not drop as rapidly because elastic recoil of the elastic arteries will transmit pressure energy back to the blood to help maintain blood pressure between heart beats. Muscular arteries distribute blood flow to the general organs of the body. The smooth muscle of the tunica media helps maintain the vessel wall against the pressure within these arteries and they are much less distensible than elastic arteries or veins. Veins have thinner walls with more connective tissue and can distend or stretch more with the blood volume within them which keeps pressure much lower. Veins are called capacitance vessels because of their distensibility and retention of approximately 65% of the circulating blood volume. Veins have one way valves to facilitate venous return against the force of gravity in this low pressure system. Contraction of skeletal muscle compresses the deep veins to propel blood past the valve toward the heart and prevent blood movement in the opposite direction. Varicose veins develop when overstretching a vein creates more sluggish blood flow and pooling of blood in the superficial veins. Varicose veins of the rectum are hemorrhoids and often develop with prolonged sitting, pregnancy, or even straining on the toilet during defecation. Sluggish blood flow in deep veins may cause a buildup of clotting factors leading to deep vein thrombosis.
The microcirculation consists of the small unnamed blood vessels within the organs and tissues of the body. Arterioles are very small diameter muscular arteries that are the main site of resistance to blood flow. Their diameter alters with changes in smooth muscle contraction due to the sympathetic nervous system. Vasoconstriction refers to a decreased diameter which increases resistance and vasodilation is the increased diameter that lowers resistances. Capillaries are the thin walled blood vessels with the smallest diameter. They do not contribute much to vascular resistance because of a relatively large total cross sectional area due to an extensive network of capillaries. Capillaries are the exchange site between plasma and interstitial fluid owing to the thinness of the vessel wall composed of just a single layer of endothelium. The permeability of the capillary wall to different components of blood is dependent upon the type of endothelium. In a continuous capillary, only small solutes and gases are capable of diffusing between plasma and interstitial fluid because the endothelial cells are closely joined and may even have tight junctions. The capillaries of the brain, lung, and skeletal muscle are continuous capillaries with the brain capillaries being the least permeable and the skeletal muscle capillaries being more permeable. Fenestrated capillaries are formed by endothelial cells that have holes through them and wider intercellular clefts. These much leakier capillaries are found in the kidney and intestines. Sinusoid capillaries are sieve-like capillaries which have the greatest permeability. In fact, in the sinusoid capillaries of red bone marrow, liver, and spleen, the gaps are large enough to allow red blood cells to pass into and out from the tissue. The entrance to a capillary network is often guarded by a precapillary sphincter, a tuft of smooth muscle. The precapillary sphincter is either closed preventing blood flow through the capillary or open which allows capillary blood flow. Opening of a precapillary sphincter is generally dependent on local metabolism. The more metabolically active tissue will generate local metabolites which relax the smooth muscle to open the precapillary sphincter. Venules return blood from the capillary network to the veins. Reabsorption of interstitial fluid is associated with these vessels due to their low hydrostatic pressure.
Major Arteries of the Body
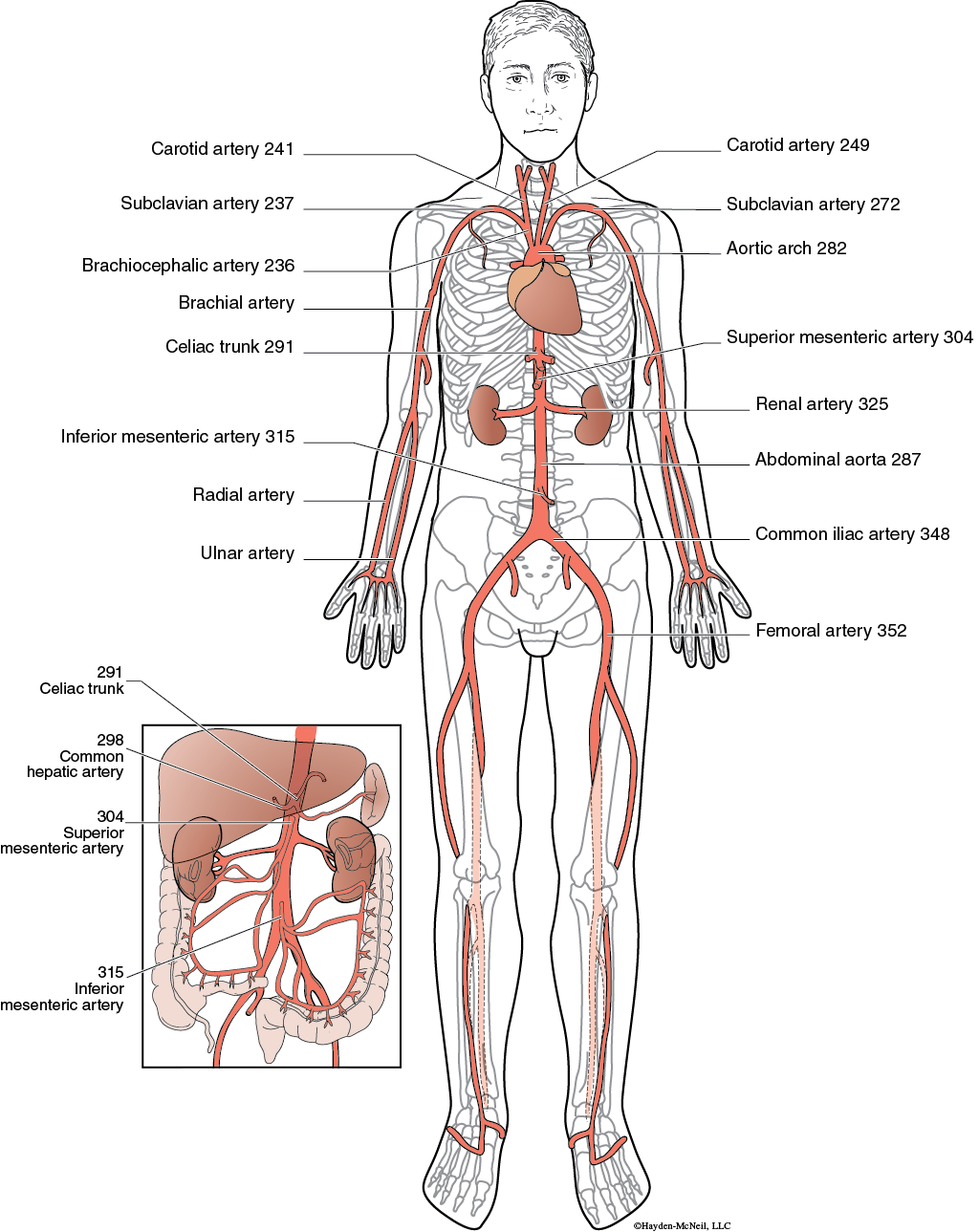
The major systemic arteries of the body branch off from the aorta, the large elastic artery which serves as a pressure reservoir to maintain blood pressure during diastole. Three blood vessels, the brachiocephalic, left common carotid and left subclavian, branch from the aortic arch. The brachiocephalic is only seen on the right side of the body and quickly subdivides into a right common carotid and left subclavian. The common carotid artery delivers blood to the head and the brain and the subclavian delivers blood to the arm where it continues as the brachial artery which subdivides into a radial artery and ulnar artery. The brachial artery is commonly used for measuring blood pressure and the radial artery is used to measure pulse rate to determine heart rate. The thoracic aorta is a continuation of the aorta through the thoracic cavity and mainly has small intercostal arteries that branch off from it. It is the second main site for aortic aneurysms. The abdominal aorta is the portion inferior to the diaphragm as it passes through the abdominal cavity. It is the leading region of aortic aneurysms. It bifurcates into a right and left common iliac artery. These will continue into the leg as the superficial femoral artery which branches in the thigh. Other branches of the abdominal aorta include the celiac trunk which leads to the common hepatic artery providing blood flow to the liver, the superior mesenteric artery providing blood flow to the small intestine and proximal portion of the colon, and the inferior mesenteric artery providing blood flow to the distal portion of the colon and rectum. The renal arteries provide blood flow to the kidneys and account for 20% of the resting cardiac output.
Major Veins of the Body
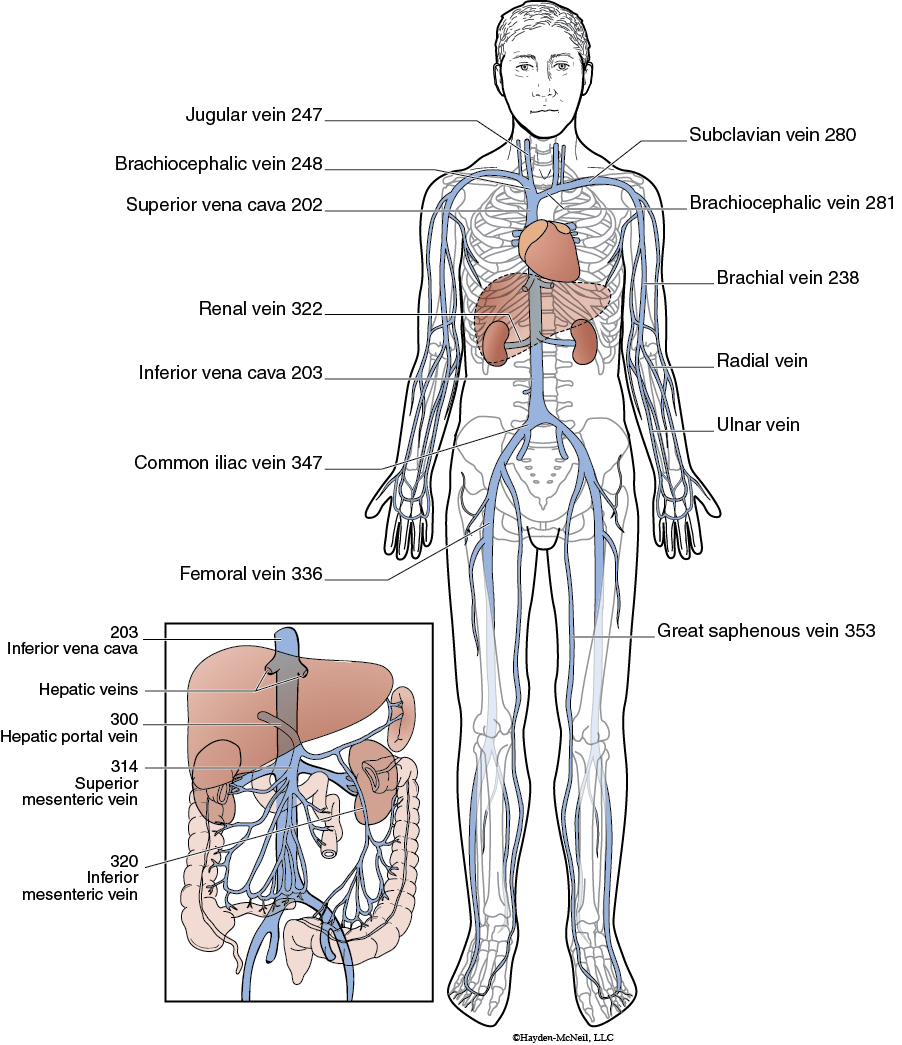
The major systemic veins return blood back to the right atrium through the superior vena cava, draining those structures above the diaphragm, and the inferior vena cava draining those portions below the diaphragm. Unlike the artery, the brachiocephalic vein is a paired vessel that joins the jugular vein draining the head and brain and the subclavian vein draining the arm. Venous return from the arm includes drainage from the radial and ulnar vein into the brachial vein that then enters the subclavian vein. In addition to these deep veins that travel with the corresponding arteries, venous return also involves superficial veins that are close to the skin surface. These superficial veins are used for obtaining blood samples, donating blood, and administering fluids with an intravenous line.
The inferior vena cava is responsible for venous return from structures below the diaphragm and is formed by joining the two common iliac veins. Each common iliac vein drains blood from the leg by way of the femoral vein. The great saphenous veins and other superficial veins provide additional drainage from the leg. Superficial vessels are the ones that engorge with slow moving blood when varicose veins develop. An interesting feature is the far less numbers of veins that directly drain into the inferior vena cava compared to the number of vessels that branch from the abdominal aorta. The renal veins drain the kidneys and the hepatic veins drain the liver directly into the inferior vena cava. However, venous return through the superior mesenteric and inferior mesenteric veins from the small intestines and colon does not directly connect to the inferior vena cava. Instead, these vessels drain first through the hepatic portal vein into the liver and then through the hepatic veins into the inferior vena cava. This blood flow enables the important metabolic functions of the liver which we will explore in Chapter 13. These functions include nutrient metabolism, plasma protein formation, and blood detoxification.
Blood Pressure
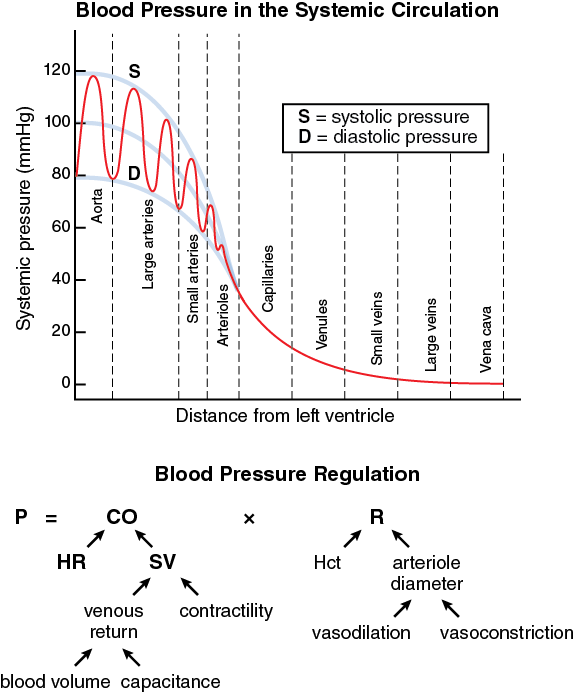
Blood pressure is dependent on the activity of the heart in terms of cardiac output and the aspects of the blood vessels in terms of resistance. The cardiac output is determined by the heart rate and the stroke volume or how much blood is pumped each time the heart contracts. The stroke volume is dependent on the amount of blood returning to the heart, venous return, and how forcefully the ventricle contracts, contractility. Both the blood volume and the capacitance of veins contribute to venous return. The resistance to blood flow depends on the arteriole diameter as the main source of resistance. The viscosity or thickness of blood as measured by the hematocrit also contributes to resistance. The body utilizes homeostasis to maintain a fairly constant blood pressure to ensure adequate flow to the brain and other highly metabolic organs. The autonomic nervous system exerts extrinsic control over heart rate, stroke volume, and arteriole resistance to maintain blood pressure. The sympathetic nervous system raises blood pressure by increasing heart rate and stroke volume. Sympathetic neurons increase heart rate by enhancing the rate of diastolic depolarization, shortening the duration of ventricular action potentials, and speeding conduction through the AV node. Changes in stroke volume are obtained by increasing venous return and contractility. Sympathetic neurons activate smooth muscle in the veins, making them less distensible to lower capacitance. This action prevents blood from pooling in the veins and encourages venous return. Sympathetic activity to the ventricles increases contractility, the force of contraction at any given muscle length. This increases the ejection fraction, the percentage of the end diastolic volume pumped out each time the ventricles contract. Lowering blood pressure is achieved by decreasing sympathetic influence to the heart and arterioles. The parasympathetic nervous system is involved in lowering blood pressure only by decreasing heart rate. At rest, your heart rate is lower than the 100 bpm intrinsic activity of the SA node because of vagal tone inhibiting diastolic depolarization and increasing the maximum diastolic potential.
Blood Pressure
Both neural control and hormonal control are involved with regulating blood pressure. Neural control involves activity of baroreceptors located in the aortic arch and carotid arteries. The baroreceptors monitor blood pressure and activate control centers in the medulla oblongata if blood pressure is too high. The fastest influence is on cardiac output with changes in heart rate rapidly elicited. Individuals exhibiting postural hypotension, low blood pressure while standing, often have a delayed or slower acting baroreceptor reflex in achieving a faster heart rate. The LAPD choke hold and the valsalva maneuver both cause a rapid decrease in heart rate and could even lead to cardiac arrest by over stimulating baroreceptors of the carotid arteries or aortic arch. Alterations in arteriole resistance involve the vasomotor center changing sympathetic influence to the smooth muscle of the arterioles. This includes vasoconstriction to increase blood pressure and vasodilation to decrease blood pressure. Not only does this change blood pressure, but arteriole resistance alters local blood flow to individual organs. Sympathetic neurons can also influence smooth muscle of veins to alter capacitance and affect venous return. Neural control is considered to be a short term influence and helps maintain blood pressure hour by hour.
Long term maintenance of blood pressure on a day by day basis involves hormonal control and changes in the blood volume through actions on the kidneys. Hormonal control is elicited by activating the juxtaglomerular apparatus (JGA) in the kidneys, osmoreceptors in the hypothalamus, and volume receptors in the atria. Because the kidneys are involved in long term maintenance of blood pressure, the hormonal influence will be explored in more detail with the urinary system. Suffice it to say at this point, activity of the JGA involves the renin-angiotensin system, osmoreceptors alter aldosterone and antidiuretic hormone (ADH) secretion, and volume receptors control secretion of atrial natriuretic peptide.
Exercise: Postural Effects on Blood Pressure
Blood Flow
Maintenance of adequate blood pressure allows for blood flow to the various organs of the body. At rest, the cardiac output is approximately 5 L/min and may raise to 25 L/min during strenuous exercise. This increased cardiac output is mostly achieved by a 280% increase in heart rate with some contribution by a 10% to 35% increase in stroke volume. The maximum heart rate can reach approximately 220 minus a person's age whereas stroke volume is maximal at 110 ml/beat. However, the circulating blood volume in an individual remains at approximately 5 L. Therefore, the blood is flowing five times more quickly through the body during exercise than at rest. This blood flow must be partitioned to the various organs with greater blood flow going to the more active tissue and shunted away from less active tissue. This is achieved by local control of the arteriole diameter through vasodilation or vasoconstriction.
Two types of control of blood flow are exhibited in the circulation, autoregulation and metabolic control. Autoregulation is the constant blood flow to an organ even with changes in blood pressure. This is accomplished by arteriole vasodilation to lower resistance if pressure falls and vasoconstriction to increase resistance if pressure rises. Autoregulation maintains a relatively constant blood flow to the kidneys for filtering metabolic wastes and other substances from the blood. Blood flow to the brain is also maintained relatively constant at a high perfusion rate to ensure nervous tissue is well oxygenated and supplied with nutrients. On the other hand, metabolic control adjusts blood flow to an organ depending on the tissue metabolism. The levels of various chemical factors induce arteriole vasodilation if they accumulate in the tissue and arteriole vasoconstriction if they wash away faster than they are generated. The chemical factors leading to vasodilation include decreased oxygen, increased carbon dioxide, decreased pH, and increased potassium ions (K+). Exercise hyperemia is the increased blood flow to skeletal muscle and cardiac muscle during their increased metabolism. Reactive hyperemia occurs in skin and other tissues in which blood flow has been reduced or even stopped due to compression. Metabolic factors will accumulate in the tissue so that blood flow is greatly increased when the compression is removed. The reddening of the skin of the buttocks when you get up from sitting is a classic example of reactive hyperemia.
Capillary Exchange
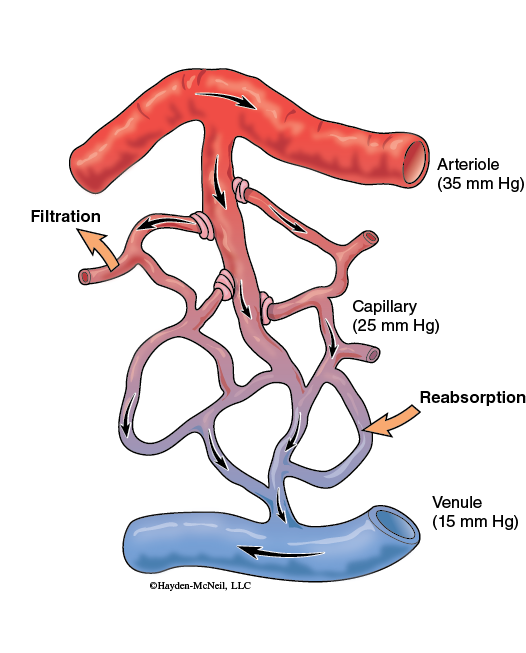
Blood flow through the microcirculation of an organ allows for delivery of oxygen and nutrients and removal of carbon dioxide and other metabolic wastes at the capillaries. Capillary exchange occurs through simple diffusion in which substances move from areas of high concentration to areas of low concentration. Therefore, oxygen and nutrients diffuse from the plasma into the interstitial fluid where the cells can utilize them and carbon dioxide and metabolic wastes diffuse from the interstitial fluid into the plasma where blood flow will remove them. The precapillary sphincter and capillary permeability help determine the extent of diffusion. In addition, fluid may move between the plasma and interstitial fluid due to bulk flow. Filtration is the movement of fluid from the plasma into the interstitial fluid and reabsorption is fluid movement from the interstitial fluid into the plasma. Fluid movement across the capillary depends on the capillary permeability, blood pressure and colloid osmotic pressure. Capillary permeability ranges from the least permeable which are continuous capillaries, through fenestrated capillaries, to the most permeable which are sinusoid capillaries. Filtration depends on a greater blood pressure compared to the interstitial fluid. Reabsorption depends on a higher concentration of plasma proteins compared to the interstitial fluid. If filtration far exceeds reabsorption, the accumulation of interstitial fluid leads to edema. Factors contributing to edema include hypertension, venous congestion, increased capillary permeability, liver disease, and lymphatic vessel obstruction.
Exercise: Heart Dissection
Dissect a preserved heart working in a group of three or four students.
- You will need one heart, a dissecting tray, and a dissecting kit for your group of laboratory partners. Each laboratory partner will need gloves and goggles.
- Notice the thick membrane surrounding the heart. This is the pericardium and must be removed to more clearly see the superficial anatomy. Using forceps, grasp the pericardium near the apex and cut it with scissors. Continue cutting the pericardium toward the base and remove it to expose the heart.
- Place the heart with the anterior surface facing up and the apex pointing toward you and examine the external anatomy. Identify the right atrium, left atrium, right ventricle, and left ventricle.
- Locate the pulmonary artery and aorta. Compare the thickness of these two vessels. Place a metal probe into the pulmonary artery and gently insert it past the pulmonary semilunar valve into the chamber of the right ventricle. Note how the probe glides to the right and appears as a slight bulge beneath the surface. Remove the probe and carefully insert it into the aorta past the aortic semilunar valve. The probe will glide straight down into the left ventricle and be deep within the heart.
- Locate the superior vena cava associated with the right atrium. Insert the probe straight through the superior vena cava and slightly lateral. The probe should exit through the remains of the inferior vena cava. Turn the heart so the posterior surface is facing up. The pulmonary veins associated with the left atrium are often damaged and not seen in these hearts.
- Using your scalpel, make a transverse cut completely through the lower third of the heart. Notice the thickness of the right ventricle and left ventricle. Using the scissors, cut through the right ventricle free wall into the right atrium to expose the tricuspid valve. Notice the papillary muscle and chordae tendineae associated with atrioventricular valves and the thinness of the valve leaflets. Identify the trabeculae carnae of the ventricle and the pectinate muscle of the atrium. Expose and examine the mitral valve between the left ventricle and the left atrium in a similar manner.
- Cut longitudinally along the pulmonary artery toward the right ventricle to expose the pulmonary semilunar valve. Notice the three pouch-like flaps. Expose the aortic semilunar valve in a similar manner by cutting longitudinally along the aorta toward the left ventricle. This valve also consists of three pouch-like flaps. Notice two orifices just distal to the aortic semilunar valve. These openings lead to the right and left coronary arteries.
- Dispose of all heart tissue into the white waste bucket. Wash and towel dry the dissecting tray. Wash, dry and return the dissecting instruments to the kit. Wipe down your table with a disinfecting wipe. Dispose of your gloves and return your goggles to the sterilization storage unit.