3.4 The Chemical and Body Senses
SMELL, TASTE, TOUCH, AND POSITION

The same is not true of all languages, however. Two hunter-gatherer groups, the Jahai in Malaysia and the Mani in Thailand, have rich odor vocabularies, with specific terms to describe precise odor categories (Majid & Burenhult, 2014; Wnuk & Majid, 2014). For example, the Jahai word p?us (pronounced pa-OOS) is used to describe the smell of old huts, day-old food, and cabbage (Majid, 2014). Given an odor identification test, the Jahai easily outscored English-speaking participants. Psychologist Asifa Majid, who has studied both tribes, believes that their olfactory expertise reflects the importance of smells in their culture and environment.
KEY THEME
Chemical stimuli produce the sensations of smell and taste, while pressure and other stimuli are involved in touch, pain, position, and balance sensations.
KEY QUESTIONS
How do airborne molecules result in the sensation of an odor?
What are the primary tastes, and how does the sensation of taste arise?
How do fast and slow pain systems differ, and what is the gate-control theory of pain?
How are body sensations of movement, position, and balance produced?
The senses of smell and taste are closely linked. If you’ve ever temporarily lost your sense of smell because of a bad cold, you’ve probably noticed that your sense of taste was also disrupted. Even a hot fudge sundae tastes bland.
Smell and taste are linked in other ways, too. Unlike vision and hearing, which involve sensitivity to different forms of energy, the sensory receptors for taste and smell are specialized to respond to different types of chemical substances. That’s why smell, or olfaction, and taste, or gustation, are sometimes called the “chemical senses” (Travers & Travers, 2009).
olfaction
Technical name for the sense of smell.
gustation
Technical name for the sense of taste.
People can get along quite well without a sense of smell. A surprisingly large number of people are unable to smell specific odors or lack a sense of smell completely, a condition called anosmia. Fortunately, humans gather most of their information about the world through vision and hearing. However, many animal species depend on chemical signals as their primary source of information.
Even for humans, smell and taste can provide important information about the environment. Tastes help us determine whether a particular substance is to be savored or spat out. Smells, such as the odor of a smoldering fire, leaking gas, or spoiled food, alert us to potential dangers.
How We Smell (Don’t Answer That!)
The sensory stimuli that produce our sensation of an odor are molecules in the air. These airborne molecules are emitted by the substance we are smelling. We inhale them through the nose and through the opening in the palate at the back of the throat. In the nose, the molecules encounter millions of olfactory receptor cells located high in the nasal cavity. Many species use airborne chemical signals, called pheromones, to communicate information about territory, mating strategies, and so forth. What about humans? The In Focus box “Do Pheromones Influence Human Behavior?” explores this question.
Unlike the sensory receptors for hearing and vision, the olfactory receptors are constantly being replaced. Each cell lasts for only about 30 to 60 days. Neuroscientists Linda Buck and Richard Axel won the 2004 Nobel Prize for their identification of the odor receptors that are present on the hair-like fibers of the olfactory neurons. Like synaptic receptors, each odor receptor seems to be specialized to respond to molecules of a different chemical structure. When these olfactory receptor cells are stimulated by the airborne molecules, the stimulation is converted into neural messages that pass along their axons, bundles of which make up the olfactory nerve.
IN FOCUS
Do Pheromones Influence Human Behavior?
Many animals communicate by releasing pheromones, chemical signals that provide information about social and sexual status to other members of the same species (Swaney & Keverne, 2009; Tirindelli & others, 2009). Pheromones may mark territories and serve as warning signals to other members of the same species. From insects to mammals, pheromones are used to communicate aggression, alarm, and fearful states (Radulescu & Mujica-Parodi, 2013). Pheromones are also extremely important in regulating sexual attraction, mating, and reproductive behavior in many animals (Wyatt, 2009). A lusty male cabbage moth, for example, can detect pheromones released from a sexually receptive female cabbage moth that is several miles away.
pheromones
Chemical signals released by an animal that communicate information and affect the behavior of other animals of the same species.
Do humans produce pheromones as other animals do? Early evidence for the existence of human pheromones comes from studies of the female menstrual cycle by University of Chicago biopsychologist Martha McClintock (1992). While still a college student, McClintock (1971) set out to scientifically investigate the folk notion that women who live in the same dorm eventually develop synchronized menstrual periods. McClintock was able to show that the more time women spent together, the more likely their cycles were to be in sync.

Later research showed that smelling an unknown chemical substance in underarm sweat from female donors synchronized the recipients’ menstrual cycles with the donors’ cycles (Preti & others, 1986; Stern & McClintock, 1998).
Since this finding, McClintock and her co-researchers have made a number of discoveries in their quest to identify human pheromones, which they prefer to call human chemosignals. Their search has narrowed to chemicals found in steroid compounds that are naturally produced by the human body and found in sweat, armpit hair, blood, and semen. One study in McClintock’s lab showed that exposure to a chemical compound in the perspiration of breast-feeding mothers significantly increased sexual motivation in other non-breastfeeding women (Spencer & others, 2004). The study’s authors speculate that the presence of breast-feeding women acts as a social signal—an indicator that the social and physical environment is one in which pregnancy and breast-feeding will be supported.
There is evidence that human chemosignals are also involved in communicating emotional states, including stress, anxiety, and fear (see Radulescu & Mujica-Parodi, 2013). Consider a recent study by Jasper de Groot and his colleagues (2012). Sweat was collected from men while they watched either a scary film or a disgusting film. Women watching a neutral video were then exposed to either the “fear sweat” or the “disgust sweat.” Although the women could not consciously perceive any odor, the women who were exposed to the “disgust sweat” produced more disgusted facial expressions and the women exposed to the “fear sweat” produced more fearful facial expressions (de Groot & others, 2012).
MYTH  SCIENCE
SCIENCE
Is it true that pheromones can make some people irresistible to members of the preferred sex?
In another study, women watched either a frightening video or a neutral video while being exposed to either “neutral sweat” or “fear sweat.” Regardless of which video the women watched, women who were exposed to the “fear sweat” were more likely to react with fearful expressions than the women who were exposed to the neutral sweat (de Groot & others, 2014).
Pheromones may not make people irresistible to the preferred sex, as they do in other animal species. Instead, it may be that these consciously undetectable chemosignals play an important role in communicating and synchronizing emotional states among people in groups (de Groot & others, 2014).
So far, hundreds of different odor receptors have been identified (Gottfried, 2010). We don’t have a separate receptor for each of the estimated 10,000 different odors that we can detect, however. Rather, each receptor is like a letter in an olfactory alphabet. Just as different combinations of letters in the alphabet are used to produce recognizable words, different combinations of olfactory receptors produce the sensation of distinct odors. Thus, the airborne molecules activate specific combinations of receptors. In turn, the brain identifies an odor by interpreting the pattern of olfactory receptors that are stimulated (Shepherd, 2006).
As shown in FIGURE 3.9, the olfactory nerves directly connect to the olfactory bulb in the brain, which is actually the enlarged ending of the olfactory cortex at the front of the brain. Axons from the olfactory bulb form the olfactory tract. These neural pathways project to different brain areas, including the temporal lobe and structures in the limbic system (Gottfried, 2010; Shepherd, 2006). The projections to the temporal lobe are thought to be part of the neural pathway involved in our conscious recognition of smells. The projections to the limbic system are thought to regulate our emotional response to odors.
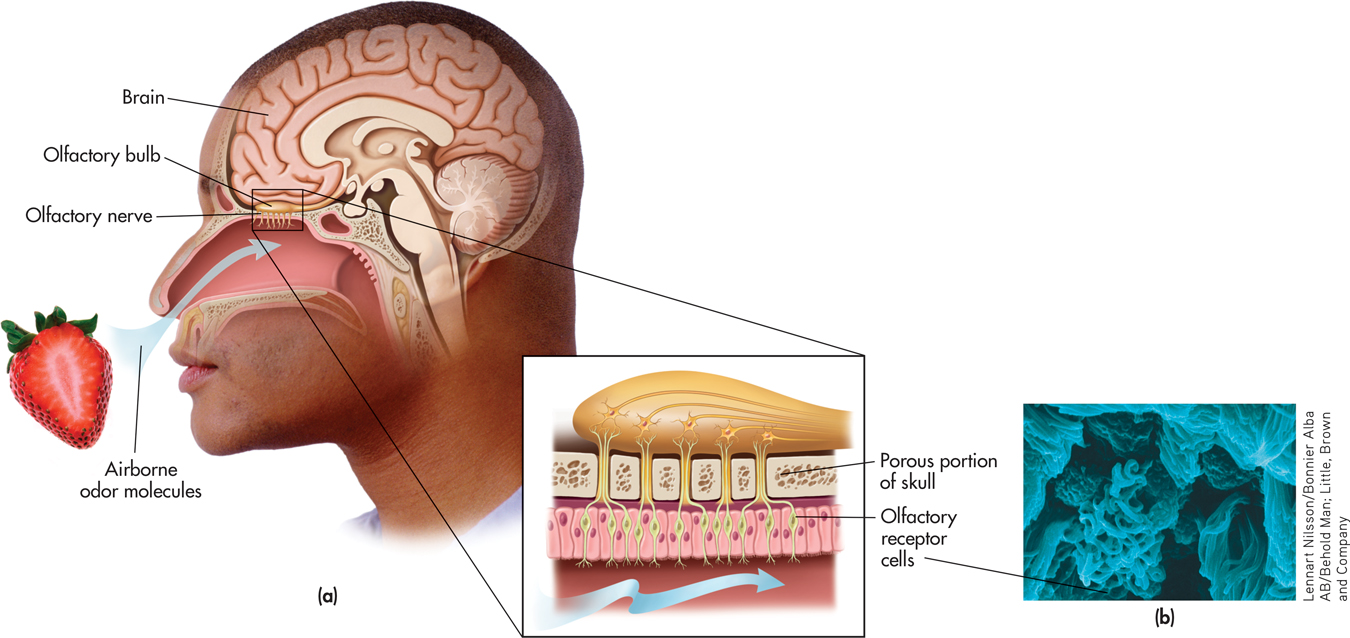
(b) The Olfactory Receptor Cells More than 5 million olfactory neurons make up the moist, mucus-bathed tissue at the back of the nose. Projecting from the olfactory neurons are the fiberlike olfactory hairs, which can be clearly seen in this photograph. Olfactory neurons are replaced every month or two.
olfactory bulb
(ole-FACK-tuh-ree) The enlarged ending of the olfactory cortex at the front of the brain where the sensation of smell is registered.

The direct connection of olfactory receptor cells to areas of the cortex and limbic system is unique to our sense of smell. As discussed in Chapter 2, all other bodily sensations are first processed in the thalamus before being relayed to the higher brain centers in the cortex. Olfactory neurons are unique in another way, too. They are the only neurons that directly link the brain and the outside world. The axons of the sensory neurons that are located in your nose extend directly into your brain!
As with the other senses, we experience sensory adaptation to odors when exposed to them for a period of time. In general, we reach maximum adaptation to an odor in less than a minute. We continue to smell the odor, but we have become about 70 percent less sensitive to it.
Olfactory function tends to decline with age. About half of those aged 65 to 80 have a significant loss of olfactory function, a number that increases to two-thirds of people aged 80 and above (Lafreniere & Mann, 2009; Rawson, 2006). At any age, air pollution, smoking, and exposure to some industrial chemicals can decrease the ability to smell. Loss of olfactory function is also associated with several diseases—including Parkinson’s disease, schizophrenia, and multiple sclerosis—and may be an early marker of Alzheimer’s disease (J. Wang & others, 2010; R. Wilson & others, 2009).
Although humans are highly sensitive to odors, many animals display even greater sensitivity. Dogs, for example, have about 200 million olfactory receptor cells, compared with the approximately 12 million receptors that humans have (Sela & Sobel, 2010). However, humans are more sensitive to smell than most people realize (Shepherd, 2004).
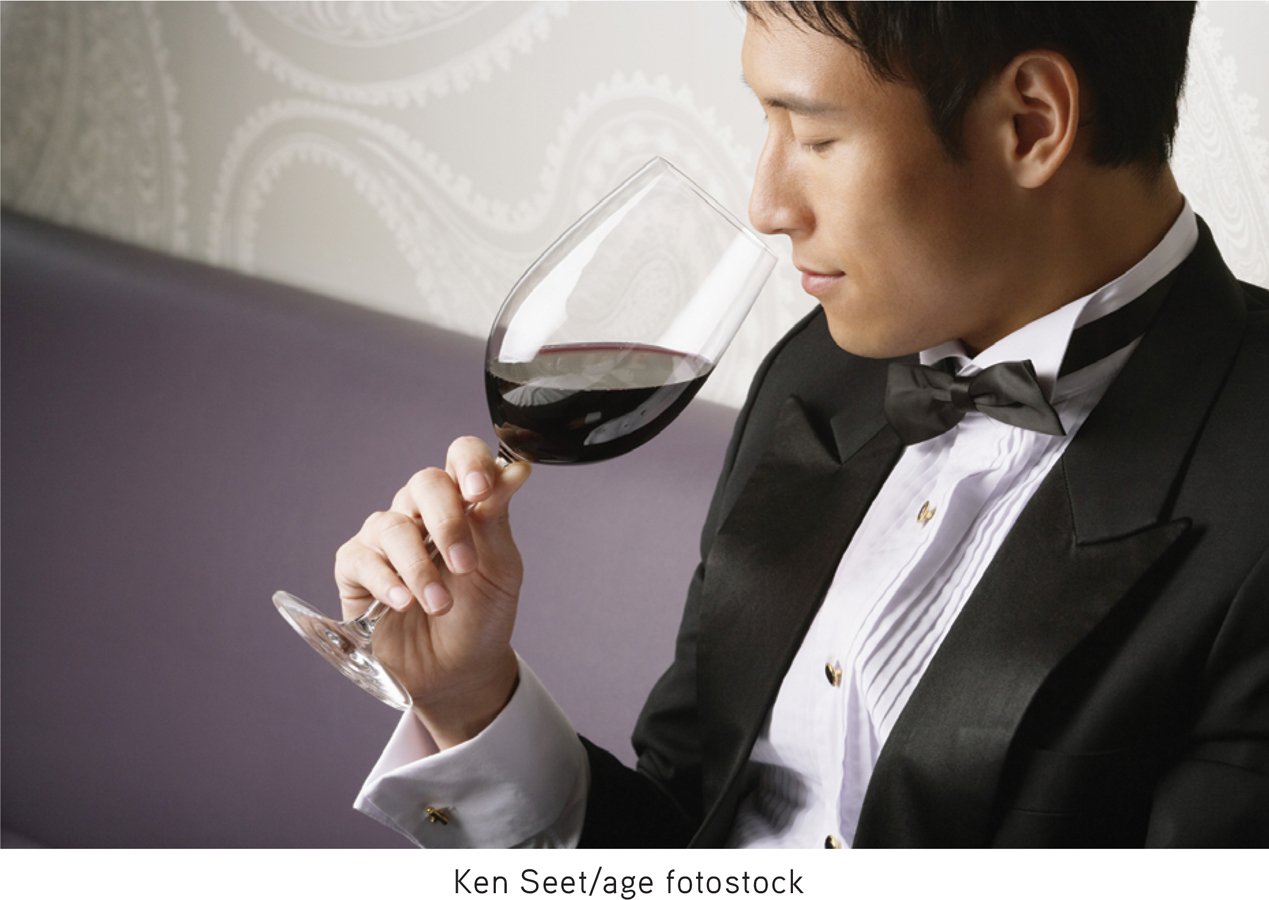
In fact, people can train their sense of smell (see photo). In a fascinating study, Wen Li and her colleagues (2006) showed that with repeated exposure to a particular class of odors (floral or minty), participants improved in their ability to distinguish subtle differences among the different scents. They also became more sensitive to the odors. These behavioral changes were accompanied by changes in the brain: fMRI scans showed increased activation in the olfactory cortex. The moral? Stop and smell the flowers often enough, and you will improve your ability to discriminate a geranium from a marigold.
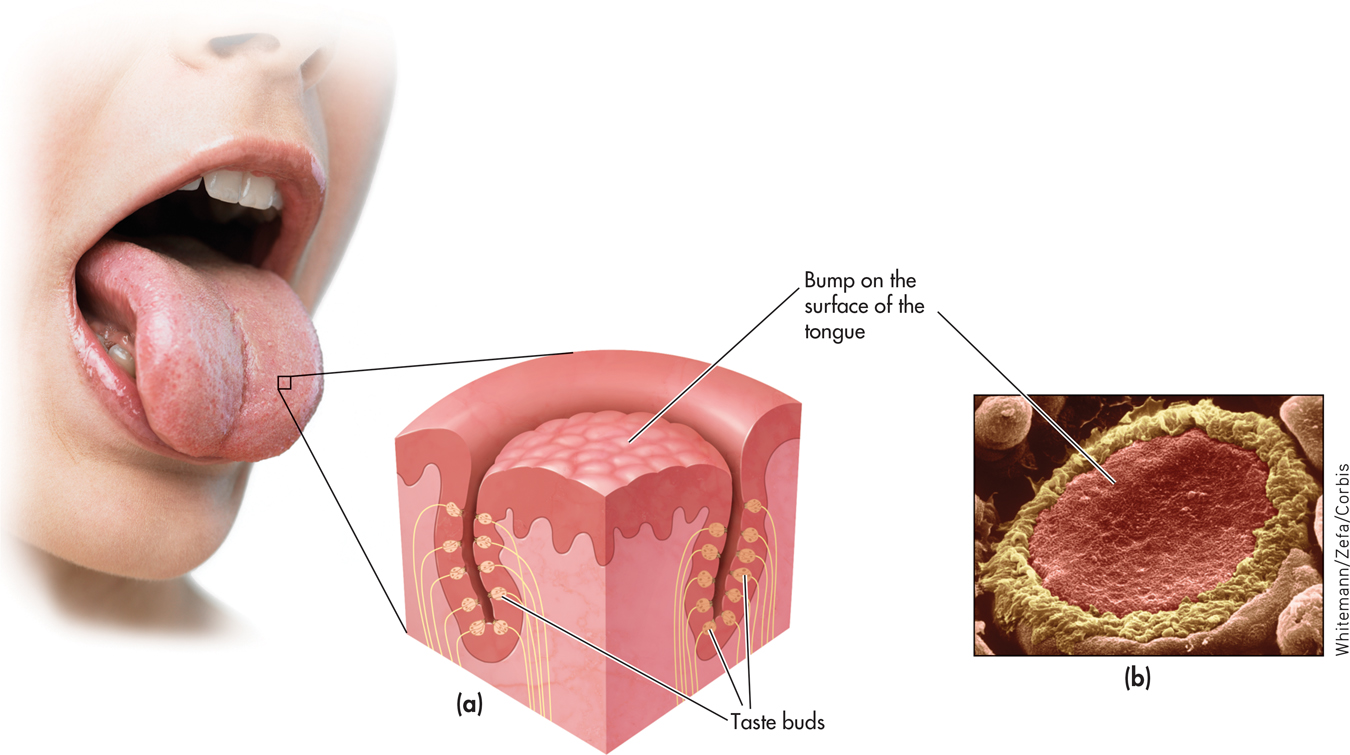
Taste
Our sense of taste, or gustation, results from the stimulation of special receptors in the mouth. The stimuli that produce the sensation of taste are chemical substances in whatever you eat or drink. These substances are dissolved by saliva, allowing the chemicals to activate the taste buds. Each taste bud contains about 50 receptor cells that are specialized for taste.
taste buds
The specialized sensory receptors for taste that are located on the tongue and inside the mouth and throat.
The surface of the tongue is covered with thousands of little bumps with grooves in between (see FIGURE 3.10). These grooves are lined with the taste buds. Taste buds are also located on the insides of your cheeks, on the roof of your mouth, and in your throat. Contrary to popular belief, there is no “tongue map” in which different regions of the tongue are specialized to respond to sweet, sour, salty, and bitter tastes. Instead, responsiveness to the five basic tastes is present in all tongue areas (Chandrashekar & others, 2006). Each taste bud shows maximum sensitivity to one particular taste and lesser sensitivity to other tastes (Chandrashekar & others, 2006). When activated, special receptor cells in the taste buds send neural messages along pathways to the thalamus in the brain. In turn, the thalamus directs the information to several regions in the cortex (Shepherd, 2006).
MYTH  SCIENCE
SCIENCE
Is it true that different tastes are detected on different parts of your tongue?
There were long thought to be four basic taste categories: sweet, salty, sour, and bitter. However, scientists identified the receptor cells for a fifth basic taste, umami (Chaudhari & others, 2000). Loosely translated, umami means “yummy” or “delicious” in Japanese. Umami is the distinctive taste of monosodium glutamate and is associated with meat and other protein-rich foods. It’s also responsible for the savory flavor of Parmesan and other aged cheeses, mushrooms, and seaweed.
From an evolutionary view, these five basic tastes supply the information we need to seek out nutrient-rich foods and avoid potentially hazardous substances (Chandrashekar & others, 2006; Eisenstein, 2010). Sweet tastes attract us to energy-rich foods, umami to protein-rich nutrients. Bitter or sour tastes warn us to avoid many toxic or poisonous substances (Peyrot des Gachons & others, 2011). Sensitivity to salty-tasting substances helps us regulate the balance of electrolytes in our diets.
Most tastes are complex and result from the activation of different combinations of basic taste receptors. Taste is just one aspect of flavor, which involves several sensations, including the aroma, temperature, texture, and appearance of food (Shepherd, 2006).
The Skin and Body Senses
While vision, hearing, smell, and taste provide you with important information about your environment, another group of senses provides you with information that comes from a source much closer to home: your own body. In this section, we’ll first consider the skin senses, which provide essential information about your physical status and your physical interaction with objects in your environment. We’ll next consider the body senses, which keep you informed as to your position and orientation in space.
TOUCH
We usually don’t think of our skin as a sense organ. But the skin is in fact the largest and heaviest sense organ. The skin of an average adult covers about 20 square feet of surface area and weighs about six pounds.
There are many different kinds of sensory receptors in the skin. Some of these sensory receptors are specialized to respond to just one kind of stimulus, such as pressure, warmth, or cold (McGlone & Reilly, 2010). Other skin receptors respond to more than one type of stimulus (Delmas & others, 2011).
One important receptor involved with the sense of touch, called the Pacinian corpuscle, is located beneath the skin. When stimulated by pressure, the Pacinian corpuscle converts the stimulation into a neural message that is relayed to the brain. If a pressure is constant, sensory adaptation takes place. The Pacinian corpuscle either reduces the number of signals sent or quits responding altogether (which is fortunate, or you’d be unable to forget the fact that you’re wearing underwear).
Sensory receptors are distributed unevenly among different areas of the body, which is why sensitivity to touch and temperature varies from one area of the body to another. Your hands, face, and lips, for example, are much more sensitive to touch than are your back, arms, and legs. That’s because your hands, face, and lips are much more densely packed with sensory receptors.
PAIN
From the sharp sting of a paper cut to the dull ache of a throbbing headache, a wide variety of stimuli can trigger pain. Pain can be defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage (Gatchel & others, 2011). As unpleasant as it can be, pain helps you survive. Pain warns you about potential or actual injury, prompting you to pay attention and stop what you are doing. Sudden pain can trigger the withdrawal reflex—you jerk back from the object or stimulus that is injuring you. (We discussed the withdrawal reflex and other spinal reflexes in Chapter 2.)
pain
The unpleasant sensation of physical discomfort or suffering that can occur in varying degrees of intensity.
Your body’s pain receptors are called nociceptors. Nociceptors are actually small sensory fibers, called free nerve endings, in the skin, muscles, or internal organs. You have millions of nociceptors throughout your body, mostly in your skin (see TABLE 3.3). For example, your fingertips may have as many as 1,200 nociceptors per square inch. Your muscles and joints have fewer nociceptors, and your internal organs have the smallest number of nociceptors.
nociceptors
Specialized sensory receptors for pain that are found in the skin, muscles, and internal organs.
Sensitivity of Different Body Areas to Pain
| Most Sensitive | Least Sensitive |
|---|---|
| Back of the knee | Tip of the nose |
| Neck region | Sole of the foot |
| Bend of the elbow | Ball of the thumb |
| Source: Information from Geldard (1972). | |
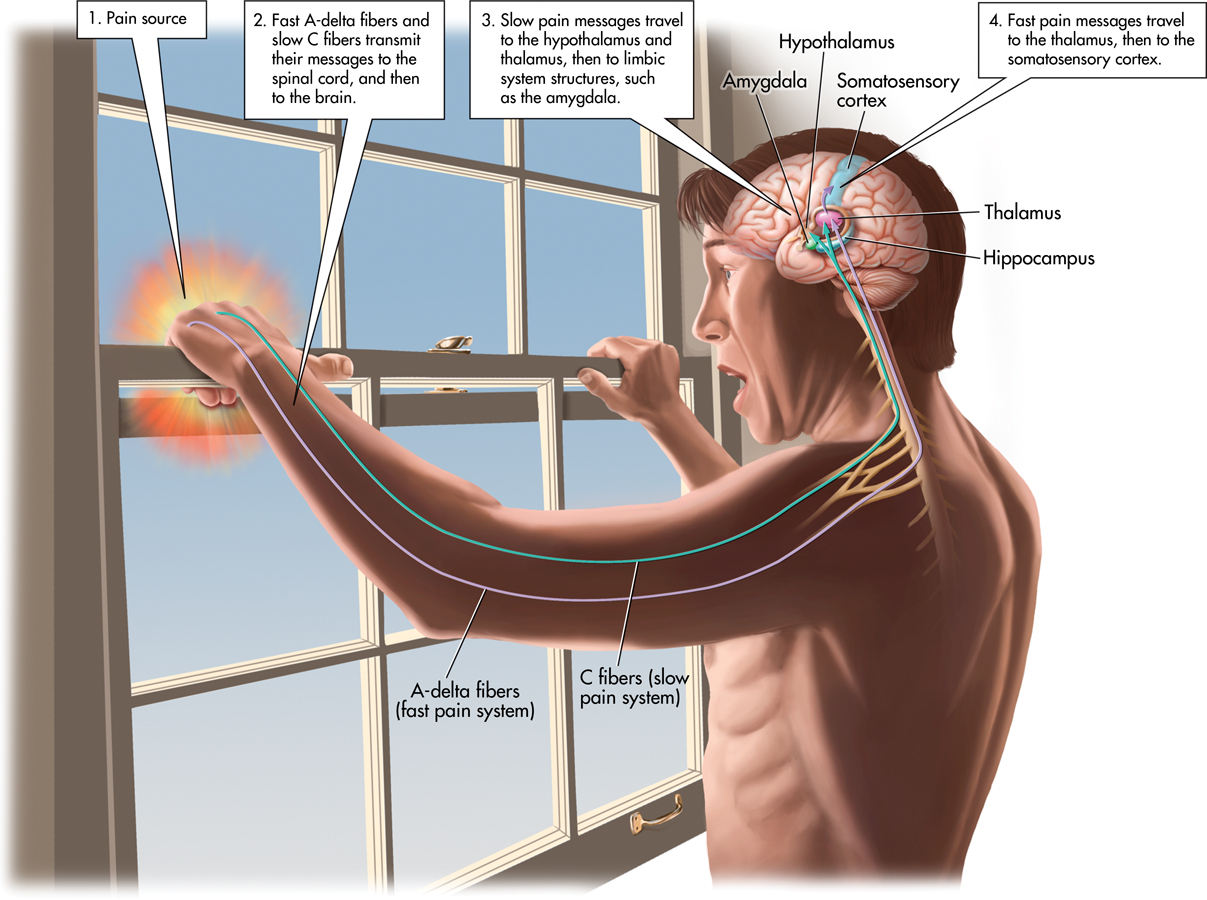
Fast and Slow Pain SystemsTo help illustrate pain pathways, imagine this scene: Your author Don was trying to close a stuck window in his office. As he wrapped his left hand on the top of the window and used his right hand to push down the lower edge, it suddenly came free and slammed shut, jamming his left fingertips between the upper and lower windows. As pain shot through him, he jerked the window back up to dislodge his mangled fingers and then headed to the kitchen for ice.
Don took little comfort in knowing that his injury had triggered two types of nociceptors: A-delta fibers and C fibers. The myelinated A-delta fibers represent the fast pain system. A-delta fibers transmit the sharp, intense, but short-lived pain of the immediate injury. The smaller, unmyelinated C fibers represent the slow pain system. As the sharp pain subsides, C fibers transmit the longer-lasting throbbing, burning pain of the injury (Guindon & Hohmann, 2009). The throbbing pain carried by the C fibers gradually diminishes as a wound heals over a period of days or weeks.
As shown in FIGURE 3.11, both the fast A-delta fibers and the slow C fibers transmit their messages to the spinal cord. Several neurotransmitters are involved in processing pain signals, but most C fibers produce a pain enhancer called substance P. Substance P stimulates free nerve endings at the site of the injury and also increases pain messages within the spinal cord (Linnman, 2013).
substance P
A neurotransmitter that is involved in the transmission of pain messages to the brain.
Most of these messages from C fibers and A-delta fibers cross to the other side of the spinal cord, then to the brain. The fast pain messages travel to the thalamus, then to the somatosensory cortex, where the sensory aspects of the pain message are interpreted, such as the location and intensity of the pain. Interestingly, morphine and other opiates have virtually no effect on the fast pain system.
!launch!
In contrast, slow pain messages follow a different route in the brain. From the spinal cord, the slow pain messages travel first to the hypothalamus and thalamus, and then to limbic system structures, such as the amygdala. Its connections to the limbic system suggest that the slow pain system is more involved in the emotional aspects of pain. Morphine and other opiates very effectively block painful sensations in the slow pain system (Guindon & Hohmann, 2009).
Factors That Influence Pain “Gates”There is considerable individual variation in the experience of pain (Edwards & others, 2009). When sensory pain signals reach the brain, the sensory information is integrated with psychological and situational information. According to the gate-control theory of pain, depending on how the brain interprets the pain experience, it regulates pain by sending signals down the spinal cord that either open or close pain “gates,” or pathways (Melzack & Wall, 1965, 1996). If, because of psychological, social, or situational factors, the brain signals the gates to open, pain is experienced or intensified. If for any of the same reasons the brain signals the gates to close, pain is reduced.
gate-control theory of pain
The theory that pain is a product of both physiological and psychological factors that cause spinal gates to open and relay patterns of intense stimulation to the brain, which perceives them as pain.
Anxiety, fear, and a sense of helplessness are just a few of the psychological factors that can intensify the experience of pain (Edwards & others, 2009). So do feelings of depression and sadness (Berna & others, 2010). And, neuroscientists have found that manipulating people’s moods by exposing them to different odors can affect their experience of pain (Villemure & Bushnell, 2009). Pleasant smells, like violets, evoke a good mood and a reduced sense of pain. But unpleasant smells, like rotten food, put people in a bad mood and heighten their sense of pain.
Along with positive moods, a sense of control can reduce the perception of pain. As one example, consider the athlete who has conditioned himself to minimize pain during competition. The experience of pain is also influenced by social and situational factors, along with cultural beliefs about the meaning of pain and the appropriate response to pain (Bosch & Cano, 2013; Gatchel & others, 2011). We discuss some helpful strategies that you can use to minimize pain in the Psych for Your Life section at the end of the chapter.
Psychological factors can also influence the release of endorphins and enkephalins, the body’s natural painkillers (see Chapter 2). Endorphins and enkephalins are produced in the brain and spinal cord. They are released as part of the body’s overall response to physical pain or stress. In the brain and spinal cord, endorphins and enkephalins inhibit the transmission of pain signals, including the release of substance P.

Sensitization: Unwarranted PainOne of the most frustrating aspects of pain management is that it can continue even after an injury has healed, such as after recovering from a spinal cord injury or severe burns. A striking example of this phenomenon is phantom limb pain, in which a person continues to experience intense painful sensations in a limb that has been amputated (Wolff & others, 2011).
How can phantom limb pain be explained? Basically, the neurons involved in processing the pain signals undergo sensitization. Earlier in the chapter, we discussed sensory adaptation, in which sensory receptors become gradually less responsive to steady stimulation over time. Sensitization is the opposite of adaptation. In sensitization, pain pathways in the brain become increasingly more responsive over time. It’s like a broken volume-control knob on your stereo that you can turn up but not down or off.
As the pain circuits undergo sensitization, pain begins to occur in the absence of any sensory input. The result can be the development of persistent, chronic pain that continues even after the injury has healed (Wolff & others, 2011). In the case of phantom limb pain, sensitization has occurred in the pain transmission pathways from the site of the amputation. The sensitized pathways produce painful sensations that mentally feel as though they are coming from a limb that is no longer there.
MOVEMENT, POSITION, AND BALANCE
The phone rings. Without looking up from your textbook, you reach for the phone, pick it up, and guide it to the side of your head. You have just demonstrated your kinesthetic sense—the sense that involves the location and position of body parts in relation to one another. (The word kinesthetics literally means “feelings of motion.”) The kinesthetic sense involves specialized sensory neurons, called proprioceptors, which are located in the muscles and joints. The proprioceptors constantly communicate information to the brain about changes in body position and muscle tension.
kinesthetic sense
(kin-ess-THET-ick) The technical name for the sense of location and position of body parts in relation to one another.
proprioceptors
(pro-pree-oh-SEP-terz) Sensory receptors, located in the muscles and joints, that provide information about body position and movement.
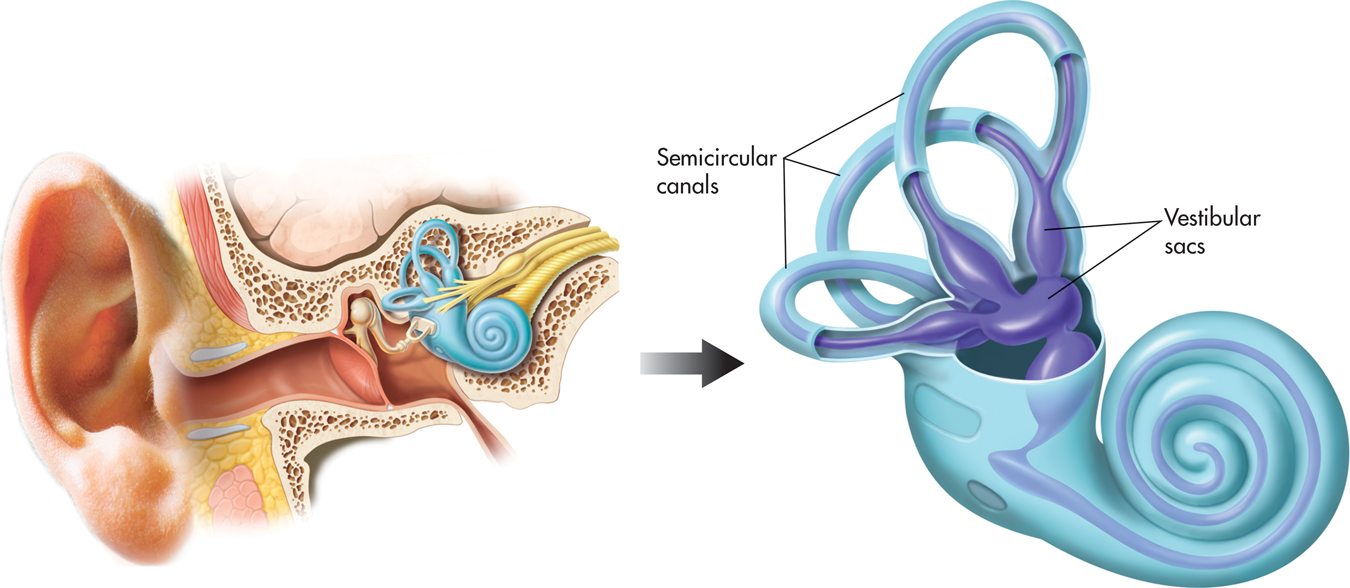
Closely related to the kinesthetic sense is the vestibular sense, which provides a sense of balance, or equilibrium, by responding to changes in gravity, motion, and body position. The two sources of vestibular sensory information, the semicircular canals and the vestibular sacs, are both located in the ear (see FIGURE 3.12). These structures are filled with fluid and lined with hair-like receptor cells that shift in response to motion, changes in body position, or changes in gravity (Eatock & Songer, 2011).
vestibular sense
(vess-TIB-you-ler) The technical name for the sense of balance, or equilibrium.
When you experience environmental motion, like the rocking of a boat in choppy water, the fluids in the semicircular canals and the vestibular sacs are affected. Changes in your body’s position, such as falling backward in a heroic attempt to return a volleyball serve, also affect the fluids. Your vestibular sense supplies the critical information that allows you to compensate for such changes and quickly reestablish your sense of balance.
Maintaining equilibrium also involves information from other senses, particularly vision. Under normal circumstances, this works to our advantage. However, when information from the eyes conflicts with information from the vestibular system, the result can be dizziness, disorientation, and nausea. These are the symptoms commonly experienced in motion sickness, the bane of many travelers in cars, on planes, on boats, and even in space. One strategy that can be used to combat motion sickness is to minimize sensory conflicts by focusing on a distant point or an object that is fixed, such as the horizon.
In the first part of this chapter, we’ve described how the body’s senses respond to stimuli in the environment. TABLE 3.4 summarizes these different sensory systems. To make use of this raw sensory data, the brain must organize and interpret the data and relate them to existing knowledge. Next, we’ll look at the process of perception—how we make sense out of the information that we receive from our environment. One long-standing question in psychology is whether information can be perceived without the involvement of normal sensory systems, a process called extrasensory perception, or ESP. We take a close look at this issue in the Critical Thinking box on pages 112-113, “ESP: Can Perception Occur Without Sensation?”
Summary Table of the Senses
| Sense | Stimulus | Sense Organ | Sensory Receptor Cells |
|---|---|---|---|
| Hearing (audition) | Sound waves | Ear | Hair cells in cochlea |
| Vision | Light waves | Eye | Rods and cones in retina |
| Color vision | Different wave-lengths of light | Eye | Cones in retina |
| Smell (olfaction) | Airborne odor molecules | Nose | Hair-like receptor cells at top of nasal cavity |
| Taste (gustation) | Chemicals dissolved in saliva | Mouth, tongue | Taste buds |
| Touch | Pressure | Skin | Pacinian corpuscle |
| Pain | Tissue injury or damage; varied | Skin, muscles, and organs | Nociceptors |
| Movement (kinesthetic sense) | Movement of the body | None; muscle and joint tissue | Proprioceptors in muscle and joint tissue |
| Balance (vestibular sense) | Changes in position, gravity | Semicircular canals and vestibular sacs | Hair-like receptor cells in semicircular canals and vestibular sacs |
CONCEPT REVIEW 3.2
The Nonvisual Senses
Fill in the blanks with the correct term.
Question 3.6
| 1. | The sensory receptors for hearing are embedded in the membrane in the . |
Question 3.7
| 2. | When activated, taste receptor cells send messages along neural pathways to the . |
Question 3.8
| 3. | The bundled axons of the olfactory receptors project to a brain structure called the . |
Question 3.9
| 4. | Hearing loss caused by damage to the bones of the middle ear is called . |
Question 3.10
| 5. | The neurotransmitter called plays an important role in the processing of pain signals. |
Question 3.11
| 6. | Because of your sense, you can touch your chin with your index finger even when your eyes are closed. |
Test your understanding of The Nonvisual Senses with
 .
.