Chapter 1. Jessie Smith
1.1 Introduction
Jessie Smith
By Justin Hines, Lafayette College and Marcy Osgood, University of New Mexico
Popup content goes in this box
New box content
Instructor's Note
This case is designed to help students understand the importance of fatty acid transport into mitochondria, the role of carnitine in this process, and the interconnections between carbohydrate and fat metabolism in humans. Students may work individually or in groups to complete this case study, however we suggest that for this case, students work independently to complete the assessment questions. Students should be allowed to freely utilize their textbook and the Internet to complete the case. The case will automatically keep track of student spending as a means to incentivize careful consideration of investigation options and discourage guessing. Assessment questions throughout the case study are automatically scored with a final open-ended assessment question to be evaluated by the instructor. The instructor may then decide how to weigh these three assessment components to determine a final score for each student or group.
Broad student learning goals for the case study:
By the time a student has finished this case study, he/she should have had the opportunity to:
- evaluate metabolic disorders using data provided by metabolite and enzyme tests.
- outline and explain the importance of carnitine-mediated fatty acid transport into mitochondria
- review fatty acid metabolism pathways and regulation
- describe and explain connections between carbohydrate and fat metabolism in humans.
You are missing vital information
You are missing vital information to sufficiently explain this incident. You may be overlooking factors related to Jesse’s physiological state at the time of the accident or your investigation may not be detailed enough. Review your options and try to select options that would provide more information relevant to Jess’s condition. Try to think about what details you still cannot fully explain.
You are missing vital information
You are missing vital information to sufficiently explain this incident. You may be overlooking factors related to Jesse’s physiological state at the time of the accident or your investigation may not be detailed enough. Review your options and try to select options that would provide more information relevant to Jess’s condition. Try to think about what details you still cannot fully explain.
I have reviewed my options and I still need help. I would like to hire an outside consultant (for $750) to review this case to provide guidance about what I might be missing
This person reviews your notes and gives you this helpful advice: In this case, it is important to consider the details that would cause abnormalities in Jesse’s physiological (metabolic) state at the time of the accident. You should completely examine her diet on the day of the event, her regular dietary habits, and her past medical history. You should also make sure that you continue as in depth as possible in these lines of investigation.
1.2 Jessie Smith
Jessie knew that she was late for the family reunion at Forest Lake Beach, probably too late for the big picnic lunch, and too early for the barbecue dinner. Too bad, she thought, because she had skipped breakfast as well, trying to get out of the city and on the road to the Lake. Perhaps there would be some leftovers; she hoped so, because she was beginning to get that slightly dizzy feeling that meant she was pushing her limits.
The whole extended family was here, sitting and talking on the beach, playing Frisbee golf, throwing a football, and some of the younger cousins were having swimming contests out from the floating raft at the periphery of the swimming area. Jessie watched the kids swimming, and smiled sadly. She had been a competitive swimmer as a teenager, and she still missed it. But, watching the group of splashing children, Jessie began to think that something wasn’t right with a little one off to the right of all the others. She put her hand up to shade her eyes from the sun and squinted; the kid was in trouble! He was throwing his arms around randomly, and thrashing the water into froth. None of the other children were close enough to notice, and there didn’t seem to be any other adults near enough to raise the alarm.
Without any further thought, Jessie ran into the lake, and after the first few lunges through the water, dove shallowly and began swimming towards the now sinking child. Her muscle memory kicked in and her strokes became fast, efficient, powerful. With each stroke she raised her head enough to keep the small head in sight; she was making progress, but he was going down! She pushed harder, picked up speed, and then she saw him, underwater, sinking quickly despite his frenzied paddling. Jessie took a breath and dove; she grabbed the little guy’s surfer swim shorts, and kicked hard back toward the surface. She began the one-sided stroke that allowed her to keep his head above the water, and swam toward the beach, which seemed, strangely, to be disappearing into a haze. Jessie felt exhausted, but kept swimming, breathing in short gasps. Her vision narrowed, and she barely felt the sand under her knees as reached the shallow water. As the little boy was taken from her arms, Jessie lost consciousness.
1.3 Jessie Smith (continued)
Jessie woke up in the hospital emergency room, very weak and confused. She tried to sit up, but her arms and legs felt heavy, completely without strength. She was dizzy, disoriented, and exhausted. A gray-haired woman in a short white coat came into view, as well as a much younger person dressed in scrubs.
"Hello, Jessie. Glad to see you’re finally awake. You were out for a pretty long time. I understand you are a hero; saved the day and your little cousin. Can you tell me what happened to make you faint? Did you hit your head, or swallow too much water? Everyone said that you were a really good swimmer, and so no one understood why you fainted."
Jessie took a deep and unsteady breath. “I haven’t tried to swim that hard since I had a head injury, 5 years ago." When the ER doctor asked Jessie if anything like this had happened to before, she looked sheepish and said yes, she had had similar episodes, all under similar circumstances--"pushing herself too hard".
1.4 What Happened to Jessie?
You are a biochemistry student who is shadowing the ER doctor.
What are you initial hypotheses about Jessie's fainting episode?
1.5 Investigation Options for Proceeding with the Case
Gathering Additional Information:
Below are a list of possible additional investigations that you and the ER doctor may conduct in order to determine the cause of Jessie’s incident and the appropriate treatment. Each investigation has a monetary cost. The goal of this exercise is to correctly solve the problem in the most cost-effective way. You will be scored on this exercise based on these criteria. What further lab tests or other investigations would you like to run on Jessie, based on the information gathered so far?
Possible Investigations:
Initial Investigations
Evaluate overall physical appearance including appearance of fingernails and presence of insect bites or other injuries ($50)
Results: Subject is a young adult female with a slim athletic frame but otherwise appears normal. No discoloration of the fingernails or abnormal ridges.
Conduct neurological evaluation ($150)
Results: No abnormalities in cognitive function were found.
Interview patient to determine dietary habits ($50)
Results: Jessie reported being a strict vegan for many years, however she claims to get a large amount of protein from plant sources. She reports eating a high calorie diet, despite her slim-build. She reports occasional moderate alcohol consumption. She is a non-smoker, does not report illicit drug use, and does not report eating anything unusual recently. She had not eaten anything the day of the fainting episode.
Investigate past medical history including current medications ($50)
Results: No heavy metals or narcotics were detected.
Test hair for common toxins (heavy metals and narcotics) ($100)
Results:: Jessie explained that she was on the verge of gaining a swimming scholarship to college when she had a rock-climbing accident and incurred a head injury, which led to epileptic episodes that were now controlled by regular administration of anticonvulsant drugs. Swimming was one of the activities she gave up, because of the fear of seizures. And, she said, she had found since the accident that she had less endurance, which she had always ascribed to the fact that she was no longer working out so much. She reported, “I take an anticonvulsant drug, valproic acid, to control seizures, and so I don’t swim, don’t really do much of anything in terms of hard exercise. I am just miserably out of shape, I guess.”
SPECIAL INVESTIGATION: The physiological side effects of valproic acid ($25)
Results:You quickly look up the side effects of Valproic acid on your smart phone; it can cause nausea and vomiting, anorexia, abnormal bleeding, and carnitine deficiency. You ask Jessie, and she claims that she has experienced none of these-- as far as she knows.
Fecal analysis – Look for blood, intestinal parasites, high levels of fat in stool. ($100)
Results: No blood or intestinal parasites were found. Levels of fat in the stool were normal considering the subject’s recent food intake.
Determine Blood Serum Concentrations
Common lipids: free fatty acids (FFAs) and triacylglycerols (TAGs) ($100)
Results: 500 mg/dL FFAs (normal range: 190-420 mg/dL); 250 mg/dL TAGs (normal range: 40-150 mg/dL)
SPECIAL INVESTIGATION: Conduct a fasting metabolism study ($150) to monitor subject’s Glc, FFAs, and ketone bodies in response to fasting
Results:As part of Jessie's follow-up evaluation, and based on her hypoglycemia at the time of the fainting episode, a 32-hr fasting study was performed. Refer to the exhibits below to see how her blood glucose, plasma triacylglycerols, fatty acids, and acetoacetate and β-hydroxybutyrate levels changed during the fasting study.
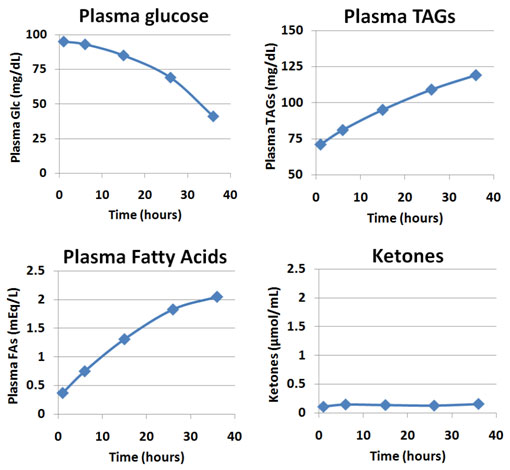
The physician who oversaw the study noted three things that were abnormal compared to a normal person who participates in the same fasting study:
- Although it is perfectly normal for plasma TAGs and fatty acids to rise, Jessie’s ending levels (at 36 hrs.) are higher than normal.
- Although it is perfectly normal for plasma glucose to fall, Jessie’s ending level (at 36 hrs.) is lower than normal.
- Normal people produce significant levels of ketone bodies by the end of the 36 hr. fast.
SPECIAL INVESTIGATION: Short-chain (12 carbons or less) fatty acid metabolism: Monitor ketone body formation in the blood
Results::Interestingly, when Jessie was fed a solution containing short-chain fatty acids and again fasted, plasma acetoacetate and β-hydroxybutyrate concentrations DID in this case increase.
Glucose ($100)
Results: [Glc] = 60 mg/dL (normal range: 70-110 mg/dL)
SPECIAL INVESTIGATION: Conduct a fasting metabolism study ($150) to monitor subject’s Glc, FFAs, and ketone bodies in response to fasting
Results:As part of Jessie's follow-up evaluation, and based on her hypoglycemia at the time of the fainting episode, a 32-hr fasting study was performed. Refer to the exhibits below to see how her blood glucose, plasma triacylglycerols, fatty acids, and acetoacetate and β-hydroxybutyrate levels changed during the fasting study.
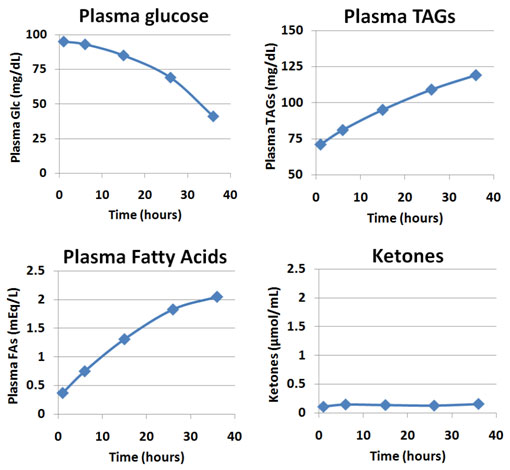
The physician who oversaw the study noted three things that were abnormal compared to a normal person who participates in the same fasting study:
- Although it is perfectly normal for plasma TAGs and fatty acids to rise, Jessie’s ending levels (at 36 hrs.) are higher than normal.
- Although it is perfectly normal for plasma glucose to fall, Jessie’s ending level (at 36 hrs.) is lower than normal.
- Normal people produce significant levels of ketone bodies by the end of the 36 hr. fast.
Ketone bodies: acetoacetate as a marker ($100)
Results: undetectable levels (normal range: undetectable)
H3O+ ions: blood pH ($50) )
Results: pH = 7.41 (normal range: 7.35 – 7.45)
Common electrolytes: Ca2+, K+, Na+, Cl-, PO43- ($100)
Results: All values are in normal ranges. (normal ranges: [Ca2+] = 8.5-10.5 gm/dL; [K+] = 3.5-5.0 meq/L; [Na+] = 135-145 meq/L; [Cl-] = 100-106 meq/L; total phosphorus = 2.6 – 4.5 mg/dL)
O2 and CO2 ($50)
Results: PO2 = 88 mmHg (normal range: 75-100mmHg); PCO2 = 41 mmHg (normal range: 35-45 mmHg)
Total protein (mostly albumin) ($50)
Results: [total protein] = 8.9 g/dL (normal range: 6.0-8.0 g/dL)
Lactate and pyruvate ($100)
Results: [lactate] = 1.0 meq/L (normal range: 0.5-2.2 meq/L); [pyruvate] = 0.05 meq/L (normal range: 0 – 0.11 meq/L)
NH4+ (total ammonia) ($50)
Results: [NH4+] = 45 mmol/L (normal range: 12-48mmol/L)
Branched amino acids (Leu as a marker) ($100)
Results: [Leu] = 1mg/dL (normal range: 0-4mg/dL)
Glycated Hemoglobin (HbA1c as a marker) ($100)
Results: HbA1c = 3.8 % (normal range: 4 - 6.5%)
Insulin ($100)
Results: [Insulin] = 10 mU/mL (normal range: 0-29 mU/mL)
Total cholesterol ($50)
Results: cholesterol = 140 mg/dL (normal range: 120-200 mg/dL)
Phenylalanine ($100)
Results: [Phe] = 0.5 mg/dL (normal range: 0-2.0 mg/dL)
Methionine ($100)
Results: [Met] = 0.2 mg/dL (normal range: 0-1.0 mg/dL)
Galactose ($100)
Results: [Gal] = 1.5 mg/dL (normal range: 0-6.0 mg/dL)
Carnitine ($100)
Results: [Carnitine] = 5 µmol/L (normal range: 24-64 µmol/L)
SPECIAL INVESTIGATION: Conduct a fasting metabolism study ($150) to monitor subject’s Glc, FFAs, and ketone bodies in response to fasting
Results:As part of Jessie's follow-up evaluation, and based on her hypoglycemia at the time of the fainting episode, a 32-hr fasting study was performed. Refer to the exhibits below to see how her blood glucose, plasma triacylglycerols, fatty acids, and acetoacetate and β-hydroxybutyrate levels changed during the fasting study.
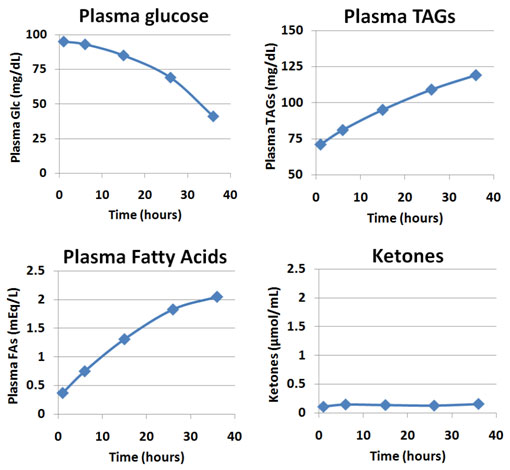
The physician who oversaw the study noted three things that were abnormal compared to a normal person who participates in the same fasting study:
- Although it is perfectly normal for plasma TAGs and fatty acids to rise, Jessie’s ending levels (at 36 hrs.) are higher than normal.
- Although it is perfectly normal for plasma glucose to fall, Jessie’s ending level (at 36 hrs.) is lower than normal.
- Normal people produce significant levels of ketone bodies by the end of the 36 hr. fast.
Common immunoglobins (IgG, IgA, IgM) ($150)
Results: [IgG] = 580 mg/dL; [IgM] = 50 mg/dL; [IgA] = 120 mg/dL (normal ranges: [IgG] = 560-1800 mg/dL; [IgM] = 45-250 mg/dL; [IgA] = 100-400 mg/dL)
Determine Urine Concentrations
Glucose ($100)
Results: [Glc] = 0.01 g/dL (normal range: 0-0.05 g/dL)
Ketone bodies (acetoacetate and acetone) ($100)
Results: undetectable levels (normal range: undetectable)
H3O+ ions: pH ($50)
Results: pH = 6.8 (normal range: 5.0 – 9.0)
phenyl-pyruvate (a phenylketone) ($200)
Results: undetectable levels (normal range: undetectable)
branched-chain α-keto acids ($200)
Results: undetectable levels (normal range: undetectable)
Specific Enzyme Tests
Asp amino-transaminases (AST) and Ala amino-transferase (ALT) ($250)
Results: Both enzymes are within normal range (normal range: 7-55 U/L)
Aldolase ($250)
Results: [Aldolase] = 1.0 U/mL (normal range: 0-7 U/mL)
Creatine kinase (CK) ($250)
Results: [CK] = 100 U/L (normal range: 40-150 U/L)
Glucose 6-phosphate dehydrogenase (G6PD) ($250)
Results: [G6PD] = 8 U/g Hb (normal range: 5-13 U/g Hb)
Pyruvate dehydrogenase (PDH) ($250)
Results: PDH complex activity= 2.5 nmol/min*mg (normal range: 2-2.5 nmol/min*mg)
Carnitine acyltransferases I & II (CAT I & CAT II) ($300)
Results: Activity of both transporters was measured in cultured fibroblasts, both were found to be within normal levels.
Lactate dehydrogenase (LDH) ($250)
Results: [LDH] = 150 U/L (normal range: 110-210 U/L)
Further Investigation Options
Conduct an MRI to determine liver fat levels. ($400)
Results: Concentrations of liver fat were found to be 12%. (normal range = 3-5.5%)
Conduct skin biopsy and send fibroblasts to center to test for Electron Transport Chain enzyme activities ($300)
Results: : ETC enzyme activities were normal.
1.6 Assessment
1.
What single problem in metabolism can explain all of Jessie's results: the muscle weakness, the hypoglycemia, increased concentration of circulating lipids, fat deposits in muscle and liver cells, and the lack of ketone body production under fasting conditions (except with administration of short-chain fatty acids)? Please be thorough in your description of the defect, and how it would explain each of the above.
ANSWER
Jessie was suffering from a deficiency of carnitine, caused by her long-term use of the anticonvulsant drug valproic acid, which decreases synthesis of carnitine. Synthesis occurs in the liver and kidney from amino acid precursors, especially lysine. Similar deficiencies can occur in patients undergoing regular renal hemodialysis (which increases excretion of carnitine), or other toxic insults to liver or kidneys due to treatment with drugs for AIDS or long-term bacterial infections.
Dietary sources of carnitine include meat and dairy products; Jessie, as a vegan, was taking in lower levels than normal of carnitine from her diet. So, her diet and her medication both contributed to the carnitine deficiency. That fateful day, she had also skipped breakfast and lunch, and so was hypoglycemic before she started her heroic swim.
There are also genetic conditions that can lead to carnitine deficiencies. The lack of a functional enzyme in the carnitine biosynthesis pathway, and defective transport proteins to allow entry of carnitine into the heart and muscle cells, and/or defective reabsorption of carnitine at the renal tubule, are examples of such genetic conditions. However, until her head injury and pharmacological intervention via valproic acid to prevent seizures, Jessie showed no symptoms, and was in fact a high-end athlete, making these less likely as the basis for her condition.
Lack of carnitine caused the inability of Jessie’s muscles to use fatty acids as substrates for beta-oxidation; without sufficient carnitine, the fatty acids cannot be converted from fatty acyl-CoA to fatty acyl-carnitine, which is the form of fatty acids that can enter the mitochondrial matrix, where the enzymes of beta oxidation are located. This causes a decrease in ATP made from oxidative metabolism. Short chain fatty acids (less than 12 Carbons long) do NOT need carnitine as a carrier of fatty acyl groups into the matrix, so such fatty acids can serve as beta oxidation substrates, and ketone bodies can be generated from the acetyl-CoA generated from this catabolic process.
The inability to use long-chain fatty acids as fuel leads to higher use of glucose. Secretion of glucagon, as glucose is depleted, causes triacylglycerol stores to be mobilized, leading to an increase in fatty acids in the blood (carried by serum albumin.)
In carnitine-deficient patients, ketones are not made from the breakdown of fatty acids, so there is no increase in ketones seen during the fasting; in normal patients, ketones increase as glucose is used up and fatty acids become the primary fuel for muscle. Finally, without the ATP generated from beta oxidation, there may be a lack of energy to generate glucose through the process of liver gluconeogenesis (though, of course, acetyl CoA or ketone bodies are not carbon sources for gluconeogenesis.) Lack of beta oxidation leads to fat deposits in the muscle and liver cells.
2.
How would you counsel Jessie about dealing with her recurring episodes? What kind of nutritional and lifestyle suggestions would you make? If she does not deal with her carnitine deficiency, what predictions do you have about future health problems for Jessie?
ANSWER
As long as she continues her valproic acid and stays a vegan, Jessie needs to adhere to a diet of frequent meals high in carbohydrates and low in fat, or the fat content should come from short-chain fatty acids only. She should also take oral carnitine supplements.
3.
Indicate whether the relative flux through the following metabolic pathways increases or decreases in a typical human after a meal balanced in carbohydrates, protein, and fat is consumed.
Liver glycogen synthesis
Liver glycogenolysis
Liver gluconeogenesis
4.
The citric acid cycle begins with the condensation of acetyl-CoA with oxaloacetate. Possible sources for acetyl-CoA in the muscle include:
| A. |
| B. |
| C. |
| D. |
| E. |
5.
Fatty acids (NOT complexed into TAGs or phospholipids) in the bloodstream are:
| A. |
| B. |
| C. |
| D. |
| E. |
6.
Which of the following statements are true about ketone bodies? (Check ALL that are true.)
A. One cause of ketone body formation is that oxaloacetate is being utilized for gluconeogenesis
B. The production of ketone bodies frees up molecules of CoA so that β-oxidation can continue
C. Ketone bodies provide an alternate substrate for glycolysis in the brain
D. Ketone bodies are formed in the brain when β-oxidation is interrupted
7.
Marasmus is the medical term for the condition that results from overall calorie starvation. In developed countries like the U.S., it is relatively uncommon. However, there is a common psychological illness, anorexia nervosa, which results in the same symptoms and problems as seen in marasmus. Both conditions result in high glucagon to insulin ratios. Jesse Smith would have also had a high glucagon to insulin ratio. Having a high glucagon to insulin ratio would do which of the following in most people?
| A. |
| B. |
| C. |
| D. |
| E. |
8.
Indicate whether the relative flux through the following metabolic pathways increases or decreases in a typical human after 12 hours of fasting.
Liver glycogen synthesis
Liver glycogenolysis
Liver gluconeogenesis
Liver fatty acid oxidation
Ketone body formation
9.
A deficiency of a particular protein in the liver causes an enlarged and fatty liver, and a reduction of ketone bodies in the blood. In the muscle, deficiency of this same protein causes recurrent muscle weakness, especially during fasting or exercise. This protein is normally found on the outside surface of the inner mitochondrial membrane. It normally releases free CoA-SH as one of its products. What is this protein?
| A. |
| B. |
| C. |
| D. |
| E. |
Activity results are being submitted...