The adrenal gland is two glands in one
An adrenal gland sits above each kidney, just below the middle of your back. Functionally and anatomically, each adrenal gland consists of a gland within a gland (Figure 40.16). The core, or adrenal medulla, produces epinephrine and, to a lesser degree, norepinephrine. The medulla develops from nervous tissue and is under the control of the nervous system. Surrounding the medulla is the adrenal cortex, which produces steroid hormones. The cortex is under hormonal control, largely by a tropic hormone produced by cells in the anterior pituitary.
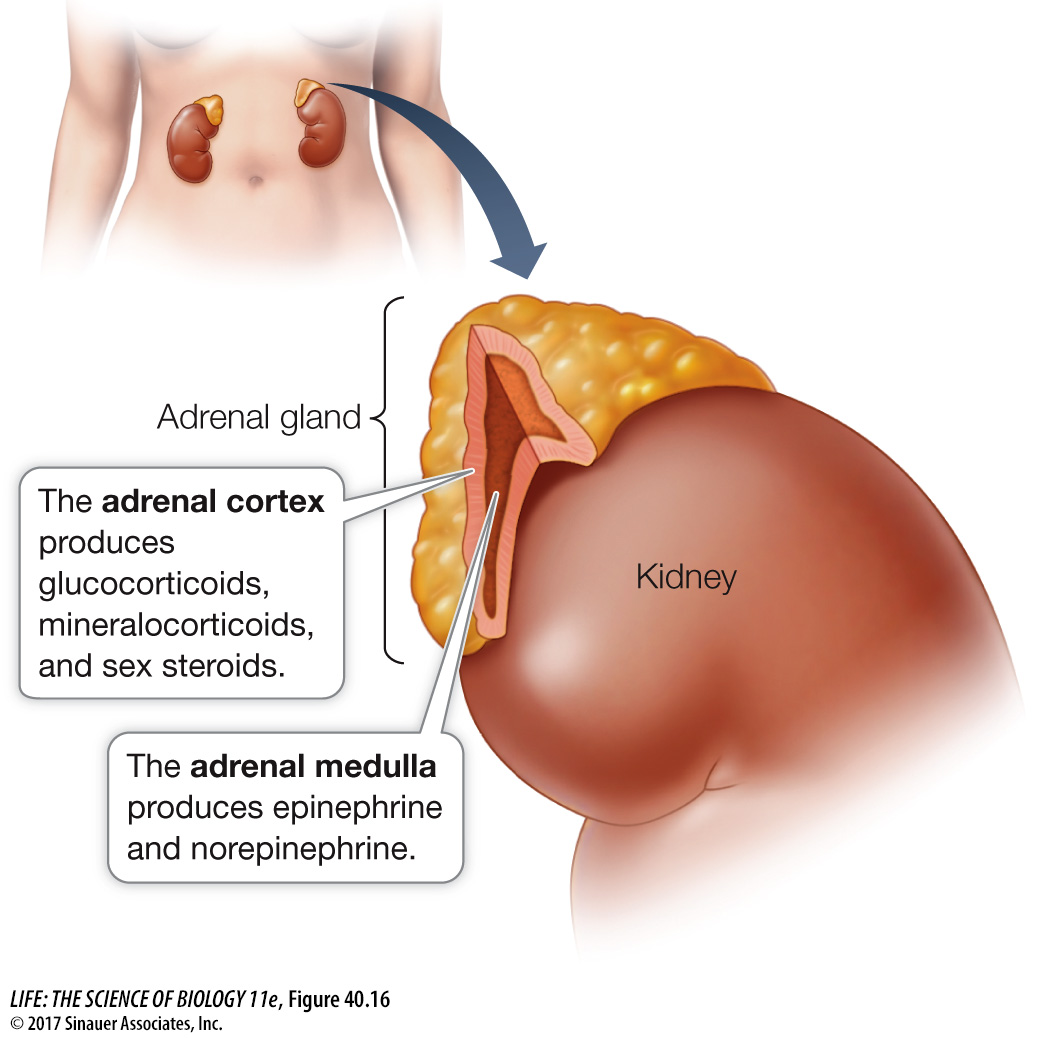
THE ADRENAL CORTEX The cells of the adrenal cortex use cholesterol to produce three classes of steroid hormones (see Figure 40.2B), collectively called corticosteroids:
Mineralocorticoids influence the salt and water balance of the extracellular fluid.
Glucocorticoids influence blood glucose concentrations as well as other aspects of fat, protein, and carbohydrate metabolism.
Sex steroids play roles in sexual development, sexual behavior, and anabolism (tissue building).
In adult humans, the adrenal cortex secretes only negligible amounts of sex steroids. The major producers of sex steroids are the gonads, as we saw in Key Concept 40.3.
Aldosterone, the primary mineralocorticoid, stimulates the kidneys to conserve sodium and excrete potassium, as we will discuss in Chapter 51. If the adrenal glands are removed from an animal, sodium must be added to its diet, or its sodium will be depleted and it will die.
The main glucocorticoid in humans is cortisol, which is critical for mediating the body’s metabolic responses to stress. Within minutes of a stressful stimulus (one provoking fear or anger, for example), blood cortisol levels begin to rise. This response is much slower than the neurally mediated epinephrine and norepinephrine response to stress, but it lasts longer. Whereas epinephrine and norepinephrine cause sudden increases in blood pressure, cortisol causes a sustained increase in blood pressure. Cortisol stimulates tissues that are not critical for escaping the danger or threat to switch from using blood glucose for energy to using fats and proteins. This action preserves circulating glucose to fuel the actions of the nervous system and skeletal muscles necessary to meet the threat. Cortisol also raises blood pressure, to increase delivery of oxygen to the muscles to prepare them for flight or fight, and inhibits the immune system. Dealing with the immediate stressor is more important than feeling sick, having allergic reactions, or healing wounds. This explains why cortisol and drugs that mimic its action are useful for reducing inflammation and allergic responses. Cortisol decreases activity of the gut and reproductive systems—
Cortisol release is controlled by adrenocorticotropic hormone (ACTH) from the anterior pituitary. ACTH release is controlled in turn by corticotropin-
Turning off the stress responses activated by cortisol is as important as turning them on. A study of stress in rats showed that old rats could turn on these stress responses as effectively as young rats, but they had lost the ability to turn them off as rapidly. As a result, they suffered from the well-
Loss of adrenal cortical function results in Addison’s disease, which is characterized by fatigue, muscle weakness, digestive problems, low blood sodium (hyponatremia), low blood pressure, and salt hunger. Without replacement hormone treatment, death is likely. An interesting symptom of Addison’s disease is darkening of many skin areas that normally are not exposed to the sun—
THE ADRENAL MEDULLA Stress causes the adrenal medulla to release epinephrine and norepinephrine that arouse the body to action. As we saw earlier in this chapter, epinephrine and norepinephrine increase heart rate and blood pressure and divert blood flow to active muscles and away from the gut and skin. Only about one-
Epinephrine and norepinephrine are both water-