Vertebrate endoskeletons consist of cartilage and bone
The endoskeleton of vertebrates is an internal scaffolding. Muscles are attached to it and pull against it. Endoskeletons are composed of rodlike, platelike, and tubelike bones connected to one another at a variety of joints that allow a wide range of movements. An advantage of endoskeletons over the exoskeletons of arthropods is that bones in the body can grow without the animal shedding its skeleton.
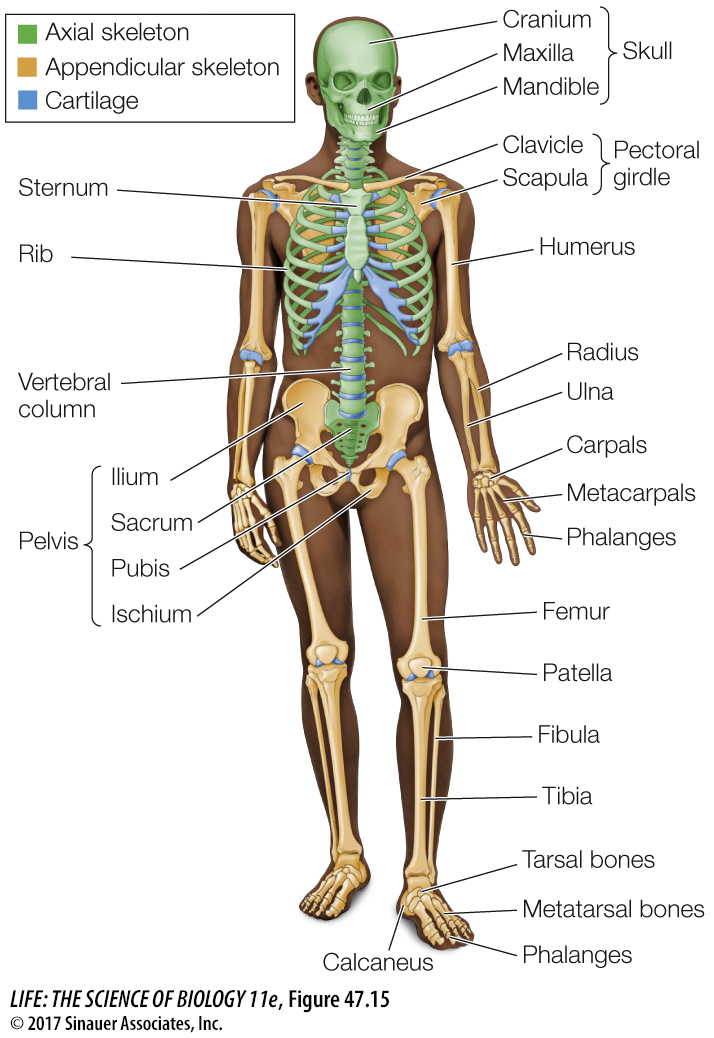
The adult human skeleton consists of 206 bones, some of which are shown in Figure 47.15. It can be divided into an axial skeleton, which includes the skull, vertebral column, sternum, and ribs; and an appendicular skeleton, which includes the pectoral girdle, pelvic girdle, and bones of the arms, legs, hands, and feet.
The vertebrate endoskeleton consists of two kinds of connective tissue, cartilage and bone, which are produced by two kinds of connective tissue cells that produce extensive extracellular matrices. Cartilage cells produce a matrix that is a tough, rubbery mixture of polysaccharides and proteins—
Bone also contains collagen fibers, but it gets its rigidity and hardness from an extracellular matrix of insoluble calcium phosphate crystals. Bone serves as a reservoir of calcium for the rest of the body and is in dynamic equilibrium with soluble calcium in the extracellular fluids of the body. This equilibrium is under the control of calcitonin and parathyroid hormone (see Figure 40.13). If too much calcium is taken from the skeleton, the bones are significantly weakened.
The living cells of bone—
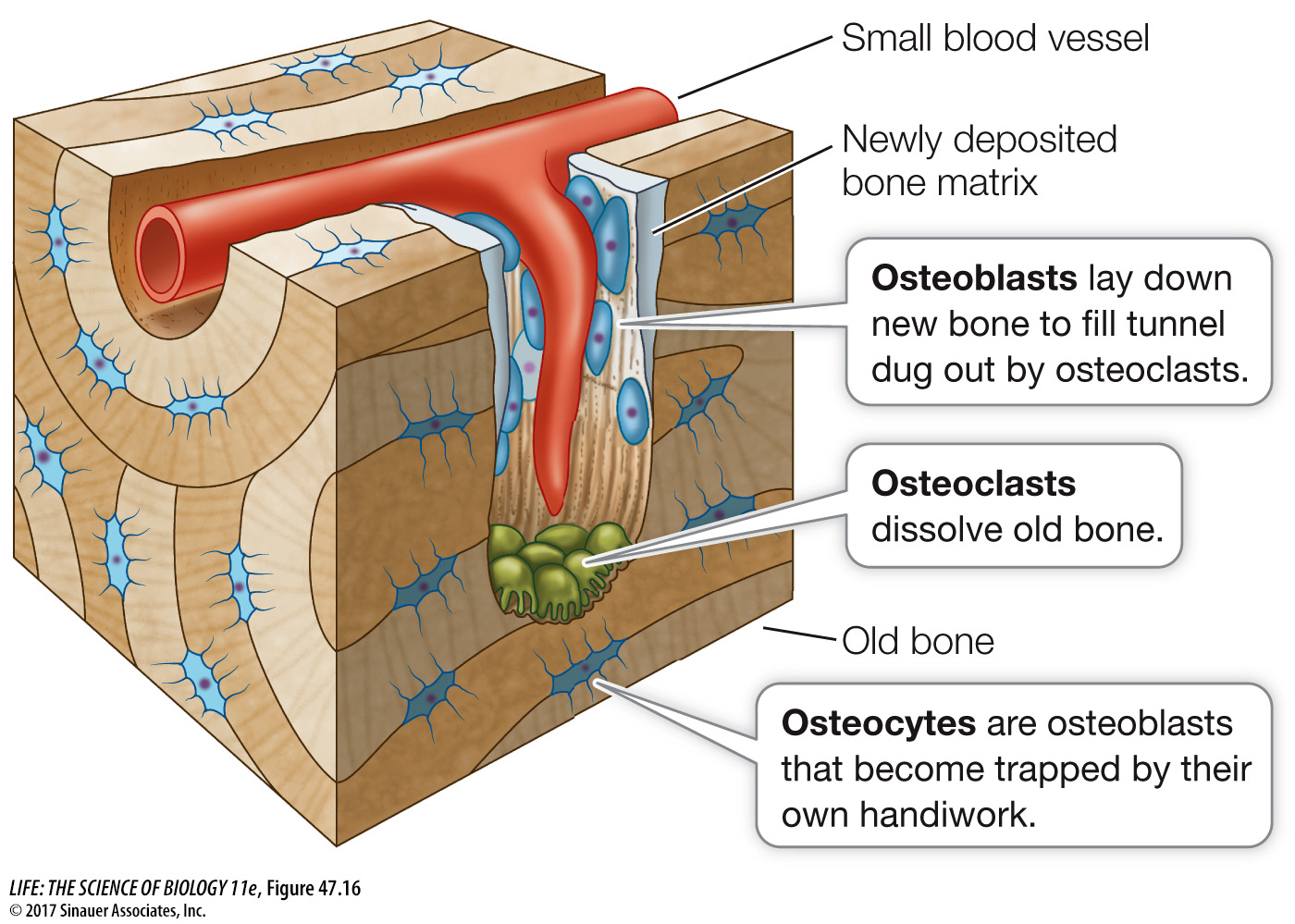
The cells that break down bone and release calcium into the extracellular fluid are called osteoclasts. They are derived from the same cell lineage that produces white blood cells. Osteoclasts erode bone, forming cavities and tunnels. Osteoblasts follow osteoclasts, depositing new bone. Thus the interplay of osteoblasts and osteoclasts constantly replaces and remodels the bones, allowing a bone to recover from damage and adjust to the forces placed on it.
A dramatic finding from the early days of manned space missions was that the bones of astronauts who spent long periods in zero gravity decalcified. Conversely, in athletes, certain bones thicken during training. Both thickening and thinning of bones are experienced by anyone who has had a leg in a cast for a long time: the bones of the uninjured leg carry the person’s weight and thicken while the bones of the inactive leg in the cast thin. We now know that there are multiple mechanisms in bone that transduce physical stress into activation of various cell signaling mechanisms that can control the bone remodeling responses to those stressors.
Because of the positive effects of physical stress on bone deposition, weight-