investigating life
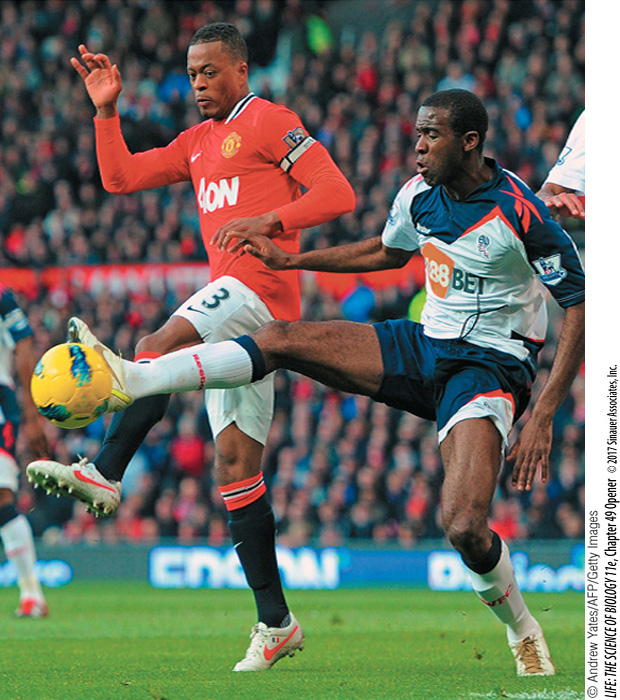
Fabrice Muamba was a much-loved and admired professional soccer player. On March 17, 2012, during a championship quarterfinal match, 23-year-old Fabrice suddenly collapsed on the field. He was immediately attended to by team physicians and a cardiologist who happened to be a spectator at the match. Fabrice received numerous defibrillator shocks, cardiopulmonary resuscitation, and was rushed to a hospital, but still his heart stopped for 78 minutes. Remarkably he survived, but there is a long list of young, fit athletes who have died from cardiac arrest during physical exertion. Sudden cardiac arrest is the most common cause of death for athletes. In most cases the cause is not a heart attack, but a condition known as hypertrophic cardiomyopathy (HCM).
Your heart is a muscular pump. At rest it beats an average of 60–70 times per minute. With each beat, it circulates about 70 milliliters of blood through your body. Without adding the increases due to work or exercise, that is 300 liters per hour, 7,200 liters per day, 2.6 million liters per year—no time-outs.
Heart failure is the leading cause of death in the United States, accounting for some one-fourth (about 600,000) of the deaths each year. Heart failure most commonly results from blockage of the blood vessels that supply the heart muscle with blood, and its risk increases with age. The most common cause of heart failure in athletes is not blocked vessels but gene mutations that affect the contractile proteins of the heart. About 1,000 such mutations have been identified, and they exist in about 1 in 500 people. Most people with one of these mutations live normally, so why are they so dangerous in athletes? The mutations decrease the efficiency of the contractions of the heart muscle, so the heart has to work much harder. Especially in athletes, the heart gets bigger to compensate for its inefficiency. The walls of the heart can get so thick that they impede the blood from leaving the heart, and the thick walls can interfere with the signals that coordinate the contractions of the heart muscle. The result is cardiac arrest. Assessment of HCM risk is improving, and many afflicted athletes are choosing to retire rather than taking a chance of dying from cardiac arrest.
Are there potential therapies that could treat HCM?