Cardiac muscle cells are electrically connected to contract in synchrony.
For the heart to function effectively as a pump, the cardiac muscle cells that make up the walls of the atria and ventricles must contract in a coordinated fashion. Atrial muscle cells must be activated to contract in synchrony during diastole to fill the ventricles, and ventricular muscle cells must contract in synchrony during systole to eject the blood from the heart. For cardiac muscle cells to pump in unison, they must be depolarized in unison by an action potential.
Cardiac muscle cells have contractile properties similar to those of skeletal muscle cells (Chapter 37). However, cardiac muscle cells are distinct in two ways. First, specialized cardiac muscle cells can generate action potentials on their own, independently of the nervous system. Second, cardiac muscle cells are in electrical continuity with one another through gap junctions (Chapter 10), meaning that they can pass their action potentials to adjacent cells. These two features of cardiac muscle cells ensure that all muscle cells in a region surrounding a heart chamber are activated and contract in unison.
The specialized cardiac muscle cells capable of generating action potentials independently function as a pacemaker that causes the heart to beat with a basic rhythm. These cells stimulate neighboring cells to contract in synchrony. They are found in two specialized regions of the heart—
Whereas most nerve cells maintain their resting membrane potential until they receive a signal from another cell, the critical feature of pacemaker cells is that their resting membrane potential gradually becomes less negative on its own until it reaches threshold and the cell fires an action potential. The tendency of their membrane potential to become less negative is due to slow leakage of sodium ions into the cell and decreased flow of potassium out of the cell. When the cell reaches threshold, voltage-
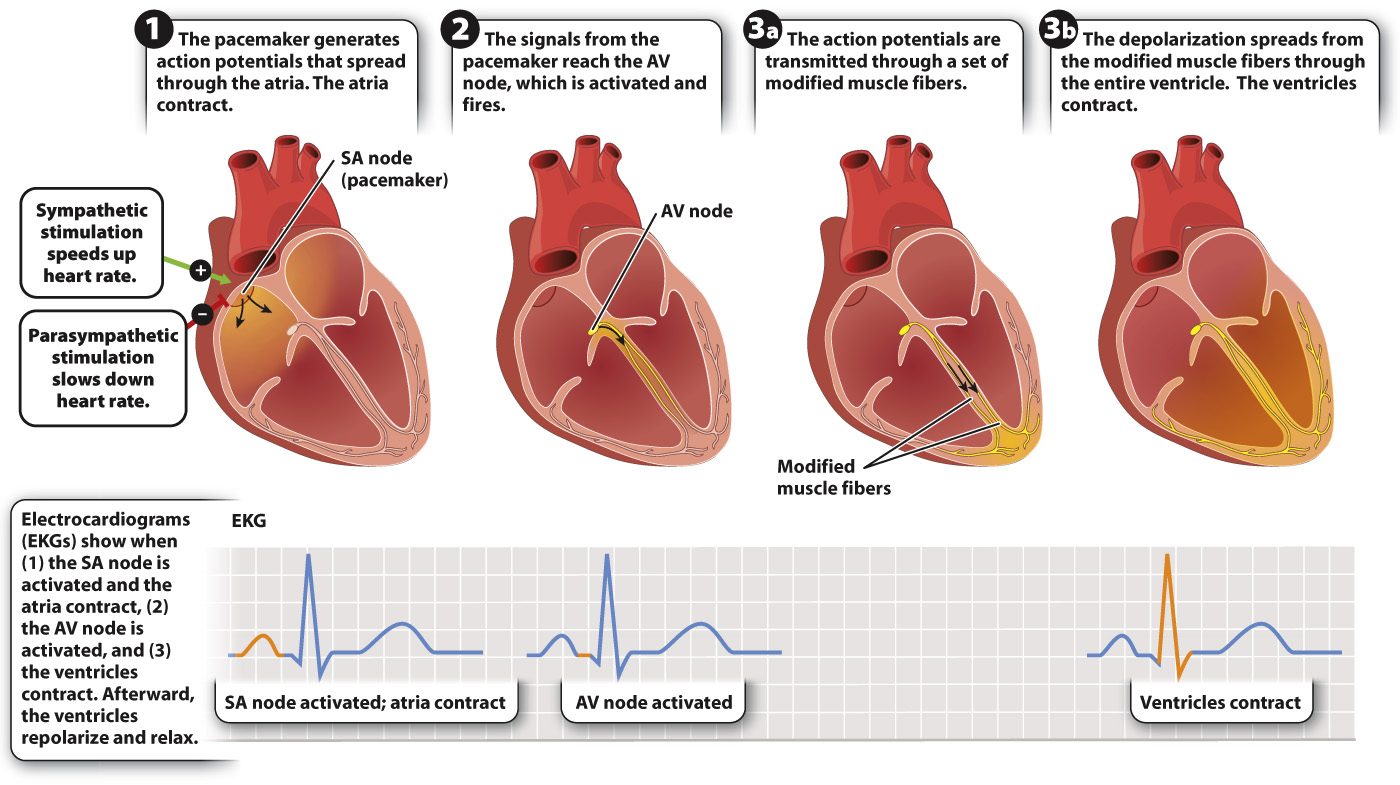
The heartbeat is initiated at the sinoatrial node, located at the junction of the vena cava and right atrium (Fig. 39.24). Because adjacent cardiac muscle cells are in electrical contact, action potentials initiated at the sinoatrial node spread rapidly from one cell to the next. Thus, when the pacemaker cells in the SA node fire an action potential, their depolarization spreads electrically throughout the right and left atria, causing them to contract in unison. Because there is no electrical contact between the atria and ventricles, the ventricles do not contract. Instead, the depolarization in the atria reaches a second set of pacemaker cells, located in the atrioventricular (AV) node.
Activation of the AV node transmits the action potential to the ventricles. A modified set of cardiac muscle fibers transmits the action potential from the AV node to the base of the ventricles. From there, the depolarization spreads throughout the ventricle walls, causing the ventricles to contract in unison. The delay in transmission from the AV node and through the conducting fibers ensures that the ventricles do not contract until they are fully filled with blood from the atria.
Electrodes placed over the surface of the chest and other body regions can record the electrical currents produced by the depolarization of the heart while it beats. This type of recording is called an electrocardiogram (abbreviated “EKG” because “kardia” is Greek for heart, although “ECG” is also used; Figure 39.24). Cardiologists use EKGs to diagnose heart problems or to determine what region of the heart has been damaged following a heart attack.