Hormones regulate the human reproductive system.
The male testes and female ovaries are not only the site of gamete production, but also part of the endocrine system (Chapter 38). That is, they respond to hormones and in turn secrete hormones. These hormones play key roles during embryonic development and puberty, and also in the adult. Hormonal control of reproduction is critically important, as it allows reproduction to take place only when, for example, a woman is able to support the developing embryo.
The master regulator of the endocrine system is the hypothalamus, located in the brain (Chapter 38). The hypothalamus secretes hormones that act on the pituitary gland, which in turn releases hormones that act on target organs (Fig. 42.17). In the case of the reproductive system, the hypothalamus releases gonadotropin-
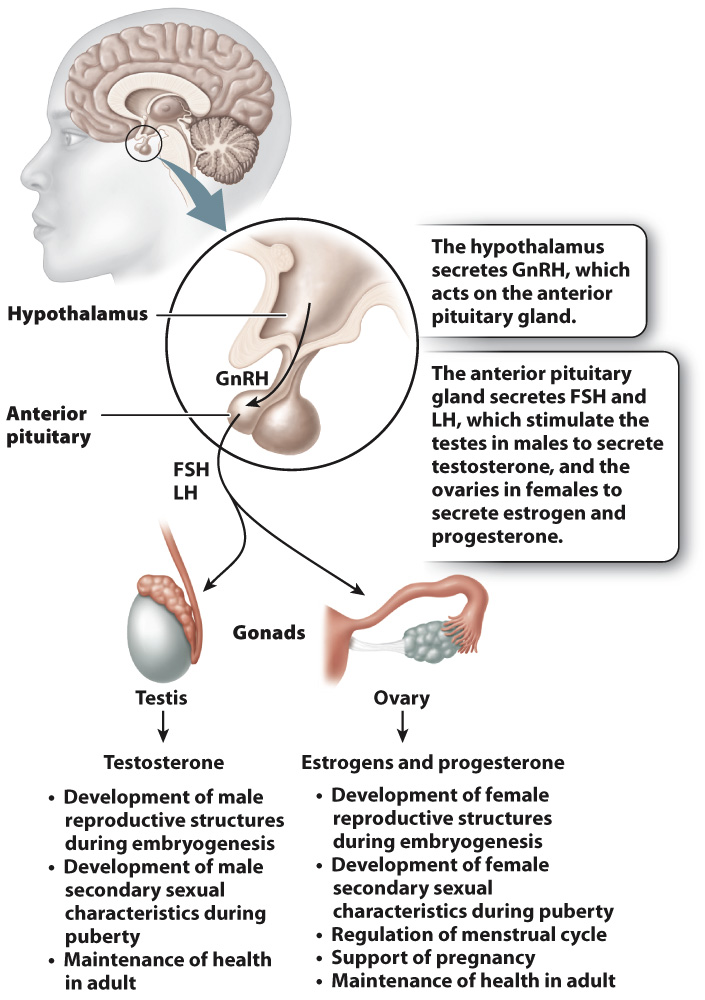
In males, LH acts on cells in the testes called Leydig cells, which secrete testosterone. Testosterone is a steroid hormone derived from cholesterol that plays key roles in male growth, development, and reproduction. Testosterone is important during embryogenesis to direct development of the male reproductive organs. At puberty, levels of testosterone increase, leading to the development of male secondary sexual characteristics, traits that characterize and differentiate the two sexes but that do not relate directly to reproduction. For males, these include a deep voice; facial, body, and pubic hair; and increased muscle mass. Testosterone together with FSH act on another group of cells in the testes, called Sertoli cells, to stimulate sperm production. Sertoli cells, located in the seminiferous tubules, support the process of sperm production. In this way, hormones help to regulate the timing of sexual maturity.
In females, an increase in the level of estrogen at puberty leads to the development of female secondary sexual characteristics, such as enlargement of the breasts, growth of body and pubic hair, and changes in the distribution of muscle and fat. Also at puberty, females begin a monthly cycle, the menstrual cycle, in which an oocyte matures and is released from the ovary under the influence of hormones (Fig. 42.18). The menstrual cycle consists of cyclical and coordinated changes in the ovaries and uterus, timing the release of an oocyte from the ovary with the growth of the uterine lining so it can support the developing embryo if fertilization occurs.
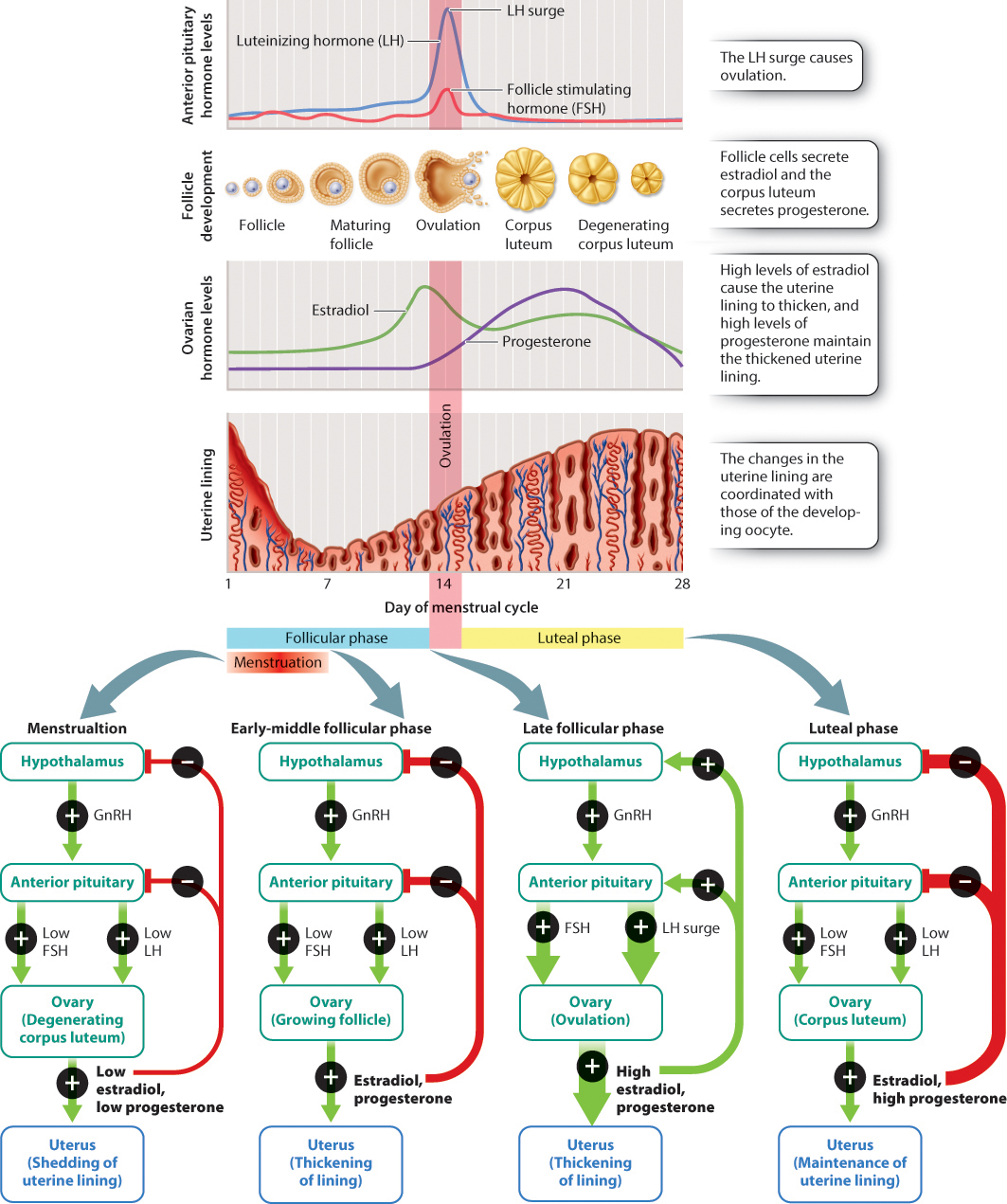
The menstrual cycle has two phases, the follicular phase and luteal phase. In the follicular phase, an oocyte develops and is eventually released from the ovary. The oocyte is located in a supporting shell of cells called a follicle. At the start of each menstrual cycle, FSH stimulates specific follicle cells called granulosa cells to secrete a form of estrogen called estradiol. In response to estradiol, oocytes in several follicles begin to mature each month, but usually only one becomes fully mature and the others die off. Estradiol also acts on the lining of the uterus, causing it to thicken. Finally, estradiol acts on the hypothalamus and anterior pituitary gland, where it reduces the secretion of GnRH, FSH, and LH by negative feedback (Fig. 42.18).
At the end of the follicular phase, this negative feedback of estradiol changes to positive feedback (Fig. 42.18). The mechanism for this change is not well understood, but may be due in part to high levels of estradiol. Positive feedback of estradiol on the hypothalamus and anterior pituitary causes a rapid increase followed by a sharp decrease in the level of LH produced by the anterior pituitary gland. This LH surge causes ovulation, the release of the oocyte from the follicle in the ovary.
Ovulation marks the end of the follicular phase and beginning of the luteal phase. The follicle, now devoid of the oocyte, is converted to a structure known as the corpus luteum, literally “yellow body,” so called because of its appearance. The corpus luteum is a temporary endocrine structure that secretes the hormone progesterone, which maintains the thickened and vascularized uterine lining, and estradiol, which inhibits the secretion of GnRH, FSH, and LH (Fig. 42.18).
The oocyte, meanwhile, is swept into the fallopian tube and travels to the uterus. If it is fertilized, the developing embryo implants into the uterine lining. In this case, the corpus luteum continues to secrete progesterone, and is first maintained by LH and then by the hormone human chorionic gonadotropin (hCG), which is released by the developing embryo. Eventually, the placenta takes over estrogen and progesterone production to maintain the uterine lining and stimulate growth of the uterus. High levels of estrogen and progesterone during pregnancy also block ovulation because they suppress the release of GnRH, FSH, and LH.
If the oocyte is not fertilized, the corpus luteum degenerates, estrogen and progesterone levels drop, and the uterine lining is shed. The monthly shedding of the uterine lining is known as menstruation. Menstrual cycles usually start occurring around age 12 in the United States and continue until approximately age 45 to 55. The cessation of menstrual cycles, called menopause, results from decreasing production of estradiol and progesterone by the ovaries.
As we have seen, the brain, anterior pituitary, ovaries, uterus, and placenta pass hormonal messages back and forth to make sure that behavior, gamete release, the uterine lining, and embryonic development are coordinated (Fig. 42.18). If hormone levels are low or absent, as occurs normally before puberty or as the result of malnutrition or some diseases, ovulation does not occur. Similarly, too much hormone at the wrong time can interfere with fertility, which is the basis for oral contraceptive pills (“the pill”). Oral contraceptive pills contain various combinations of synthetic estrogens or progesterones or both. Estrogens and/or progesterones in the pill suppress GnRH, FSH, and LH and therefore block oocyte development and ovulation.
Humans and chimpanzees both have menstrual cycles. Other placental mammals have an estrus cycle, which is characterized by phases in which females are sexually receptive. In these mammals, the uterine lining is reabsorbed instead of shed if fertilization does not occur.
Quick Check 3 A monthly course of an oral contraceptive pill is usually three weeks of hormone pills followed by one week of placebo (a sugar pill with no hormone). Why do you think the placebos are sometimes used?
Quick Check 3 Answer
High levels of estrogen and/or progesterone lead to the growth of the uterine lining. The drop in these hormones while a woman is taking placebos allows the uterine lining to be shed each month. Placebos are usually taken instead of no pills in order to help keep track of the number of days before resuming hormone-