15.4 Schizophrenia
schizophrenia a psychological disorder characterized by delusions, hallucinations, disorganized speech, and/or diminished, inappropriate emotional expression.
During their most severe periods, people with schizophrenia live in a private inner world, preoccupied with the strange ideas and images that haunt them. The word itself means “split” (schizo) “mind” (phrenia). In this disorder, however, the mind is not split into multiple personalities. Rather, the mind has suffered a split from reality that shows itself in disturbed perceptions, disorganized thinking and speech, and diminished, inappropriate emotions. Schizophrenia is the chief example of a psychosis, a broad term for a break or split from reality.
Symptoms of Schizophrenia
15-
Schizophrenia comes in varied forms. Schizophrenia patients with positive symptoms may experience hallucinations, talk in disorganized and deluded ways, and exhibit inappropriate laughter, tears, or rage. Those with negative symptoms may have toneless voices, expressionless faces, or mute and rigid bodies.
Disturbed Perceptions
People with schizophrenia sometimes have hallucinations—they see, feel, taste, or smell things that exist only in their minds. Most often, the hallucinations are sounds, frequently voices making insulting remarks or giving orders. The voices may tell the person that she is bad or that she must burn herself with a cigarette lighter. Imagine your own reaction if a dream broke into your waking consciousness, making it hard to separate your experience from your imagination. When the unreal seems real, the resulting perceptions are at best bizarre, at worst terrifying.
“When someone asks me to explain schizophrenia I tell them, you know how sometimes in your dreams you are in them yourself and some of them feel like real nightmares? My schizophrenia was like I was walking through a dream. But everything around me was real. At times, today’s world seems so boring and I wonder if I would like to step back into the schizophrenic dream, but then I remember all the scary and horrifying experiences.”
Stuart Emmons, with Craig Geiser, Kalman J. Kaplan, and Martin Harrow, Living With Schizophrenia, 1997
delusion a false belief, often of persecution or grandeur, that may accompany psychotic disorders.
Disorganized Thinking and Speech
Hallucinations are false perceptions. People with schizophrenia also have disorganized, fragmented thinking, which is often distorted by false beliefs called delusions. If they have paranoid tendencies, they may believe they are being threatened or pursued.
Maxine, a young woman with schizophrenia, believed she was Mary Poppins. Communicating with Maxine was difficult because her thoughts spilled out in no logical order. Her biographer, Susan Sheehan (1982, p. 25), observed her saying aloud to no one in particular, “This morning, when I was at Hillside [Hospital], I was making a movie. I was surrounded by movie stars…. Is this room painted blue to get me upset? My grandmother died four weeks after my eighteenth birthday.”
Jumbled ideas may make no sense even within sentences, forming what is known as word salad. One young man begged for “a little more allegro in the treatment,” and suggested that “liberationary movement with a view to the widening of the horizon” will “ergo extort some wit in lectures.”
One cause of disorganized thinking may be a breakdown in selective attention. Normally, we have a remarkable capacity for giving our undivided attention to one set of sensory stimuli while filtering out others. People with schizophrenia cannot do this. Thus, tiny, irrelevant stimuli, such as the grooves on a brick or the inflections of a voice, may distract their attention from a bigger event or a speaker’s meaning. As one former patient recalled, “What had happened to me … was a breakdown in the filter, and a hodge-
641
Diminished and Inappropriate Emotions
The expressed emotions of schizophrenia are often utterly inappropriate, split off from reality (Kring & Caponigro, 2010). Maxine laughed after recalling her grandmother’s death. On other occasions, she cried when others laughed, or became angry for no apparent reason. Others with schizophrenia lapse into an emotionless flat affect state of no apparent feeling. Most also have an impaired theory of mind—they have difficulty perceiving facial emotions and reading others’ states of mind (Green & Horan, 2010; Kohler et al., 2010). These deficiencies occur early in the illness and have a genetic basis (Bora & Pantelis, 2013).
Motor behavior may also be inappropriate. Some perform senseless, compulsive acts, such as continually rocking or rubbing an arm. Others may remain motionless for hours (a condition called catatonia) and then become agitated.
As you can imagine, such disturbed perceptions, disorganized thinking, and inappropriate emotions profoundly disrupt social and work relationships. During their most severe periods, people with schizophrenia live in a private inner world, preoccupied with illogical ideas and unreal images. Many have sleep problems, which can increase night eating and obesity (Palmese et al., 2011). Given a supportive environment and medication, over 40 percent of people with schizophrenia will have periods of a year or more of normal life experience (Jobe & Harrow, 2010). Many others remain socially withdrawn and isolated or rejected for much of their lives (Hooley, 2010).
Onset and Development of Schizophrenia
15-
chronic schizophrenia (also called process schizophrenia) a form of schizophrenia in which symptoms usually appear by late adolescence or early adulthood. As people age, psychotic episodes last longer and recovery periods shorten.
Nearly 1 in 100 people will experience schizophrenia this year, joining the estimated 24 million worldwide who have this disorder (Abel et al., 2010; WHO, 2011). It typically strikes as young people are maturing into adulthood. It knows no national boundaries, and it affects both males and females. Men tend to be struck earlier, more severely, and slightly more often (Aleman et al., 2003; Eranti et al., 2013; Picchioni & Murray, 2007). The risk of schizophrenia is higher for those who experience childhood abuse: They are three times more likely than their unabused counterparts to develop this disorder (Matheson et al., 2013). Other types of childhood adversity, such as bullying, also increase the risk (Varese et al., 2012).
acute schizophrenia (also called reactive schizophrenia) a form of schizophrenia that can begin at any age, frequently occurs in response to an emotionally traumatic event, and has extended recovery periods.
When schizophrenia is a slow-
When previously well-
Understanding Schizophrenia
Schizophrenia is a dreaded psychological disorder. It is also one of the most heavily researched. Most studies now link it with abnormal brain tissue and genetic predispositions. Schizophrenia is a disease of the brain manifested in symptoms of the mind.
642
Brain Abnormalities
15-
Might chemical imbalances in the brain underlie schizophrenia? Scientists have long known that strange behavior can have strange chemical causes. The saying “mad as a hatter” refers to the psychological deterioration of British hatmakers whose brains, it was later discovered, were slowly poisoned as they moistened the brims of mercury-
Dopamine Overactivity One possible answer emerged when researchers examined schizophrenia patients’ brains after death. They found an excess of receptors for dopamine—a sixfold excess for the dopamine receptor D4 (Seeman et al., 1993; Wong et al., 1986). Such a hyper-
Most people with schizophrenia smoke, often heavily. Nicotine apparently stimulates certain brain receptors, which helps focus attention (Diaz et al., 2008; Javitt & Coyle, 2004).
Abnormal Brain Activity and Anatomy Brain scans show that abnormal activity accompanies schizophrenia. Some people diagnosed with schizophrenia have abnormally low brain activity in the frontal lobes, areas that help us reason, plan, and solve problems (Morey et al., 2005; Pettegrew et al., 1993; Resnick, 1992). Brain scans also show a noticeable decline in the brain waves that reflect synchronized neural firing in the frontal lobes (Spencer et al., 2004; Symond et al., 2005). Out-
One study took PET scans of brain activity while people were hallucinating (Sil-
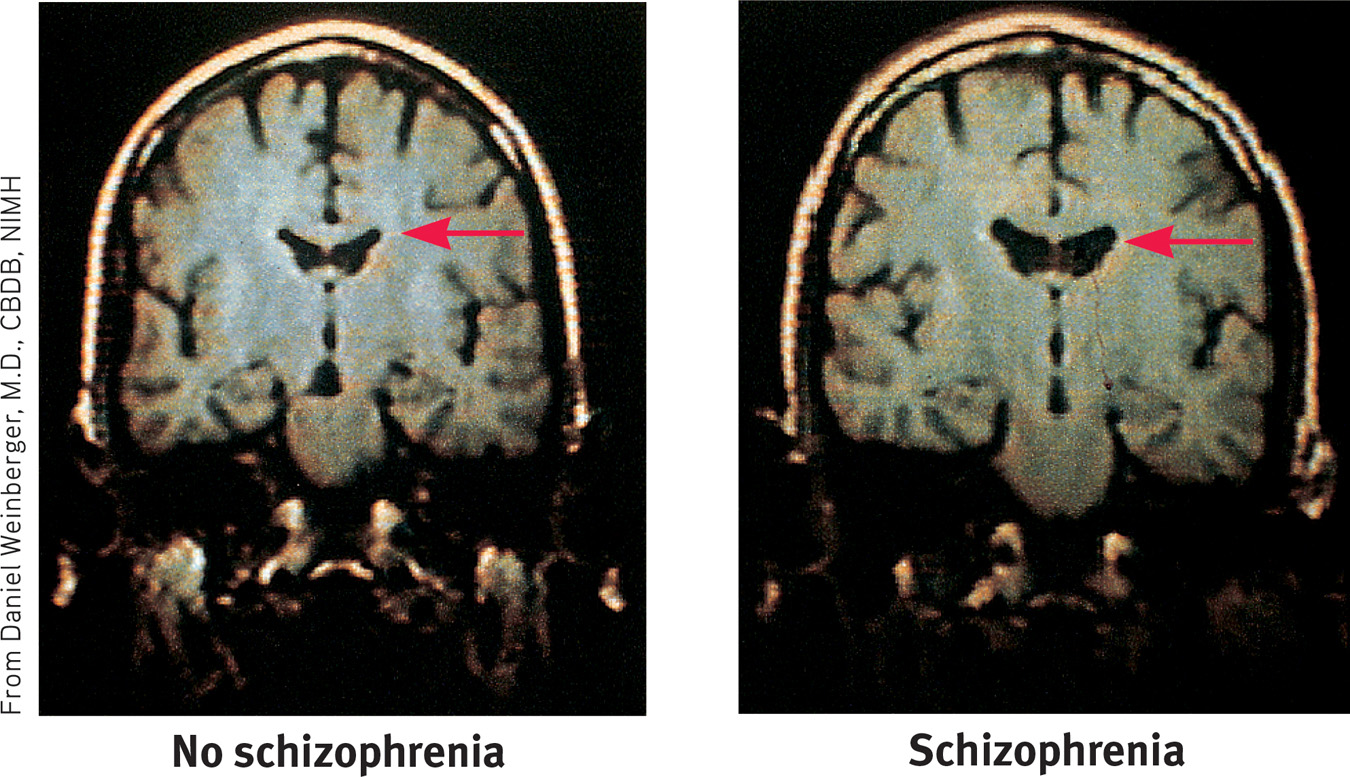
Many studies have found enlarged, fluid-
Two smaller-
Prenatal Environment and Risk
15-
What causes brain abnormalities in people with schizophrenia? Some scientists point to mishaps during prenatal development or delivery (Fatemi & Folsom, 2009; Walker et al., 2010). Risk factors for schizophrenia include low birth weight, maternal diabetes, older paternal age, and oxygen deprivation during delivery (King et al., 2010). Famine may also increase risks. People conceived during the peak of World War II’s Dutch wartime famine later developed schizophrenia at twice the normal rate. Those conceived during the famine of 1959 to 1961 in eastern China also displayed this doubled rate (St. Clair et al., 2005; Susser et al., 1996).
643
Let’s consider another possible culprit. Might a midpregnancy viral infection impair fetal brain development (Brown & Patterson, 2011)? Can you imagine some ways to test this fetal-
- Are people at increased risk of schizophrenia if, during the middle of their fetal development, their country experienced a flu epidemic? The repeated answer has been Yes (Mednick et al., 1994; Murray et al., 1992; Wright et al., 1995).
- Are people born in densely populated areas, where viral diseases spread more readily, at greater risk for schizophrenia? The answer, confirmed in a study of 1.75 million Danes, has again been Yes (Jablensky, 1999; Mortensen, 1999).
- Are those born during the winter and spring months—after the fall-winter flu season—also at increased risk? Although the increase is small, just 5 to 8 percent, the answer has been Yes (Fox, 2010; Schwartz, 2011; Torrey et al., 1997, 2002).
- In the Southern Hemisphere, where the seasons are the reverse of the Northern Hemisphere, are the months of above-average schizophrenia births similarly reversed? Again, the answer has been Yes, though somewhat less so. In Australia, people born between August and October are at greater risk. But there is an exception: For people born in the Northern Hemisphere, who later moved to Australia, the risk is greater if they were born between January and March (McGrath et al., 1995, 1999).
- Are mothers who report being sick with influenza during pregnancy more likely to bear children who develop schizophrenia? In one study of nearly 8000 women, the answer was Yes. The schizophrenia risk increased from the customary 1 percent to about 2 percent—but only when infections occurred during the second trimester (Brown et al., 2000). Maternal influenza infection during pregnancy affects brain development in monkeys also (Short et al., 2010).
- Does blood drawn from pregnant women whose offspring develop schizophrenia show higher-than-normal levels of antibodies that suggest a viral infection? In one study of 27 women whose children later developed schizophrenia, the answer was Yes (Buka et al., 2001). And the answer was again Yes in a huge California study, which collected blood samples from some 20,000 pregnant women during the 1950s and 1960s (Brown et al., 2004). Another study found traces of a specific retrovirus (HERV) in nearly half of people with schizophrenia and virtually none in healthy people (Perron et al., 2008).
These converging lines of evidence suggest that fetal-
Why might a second-
Genetic Factors
15-
Fetal-
644
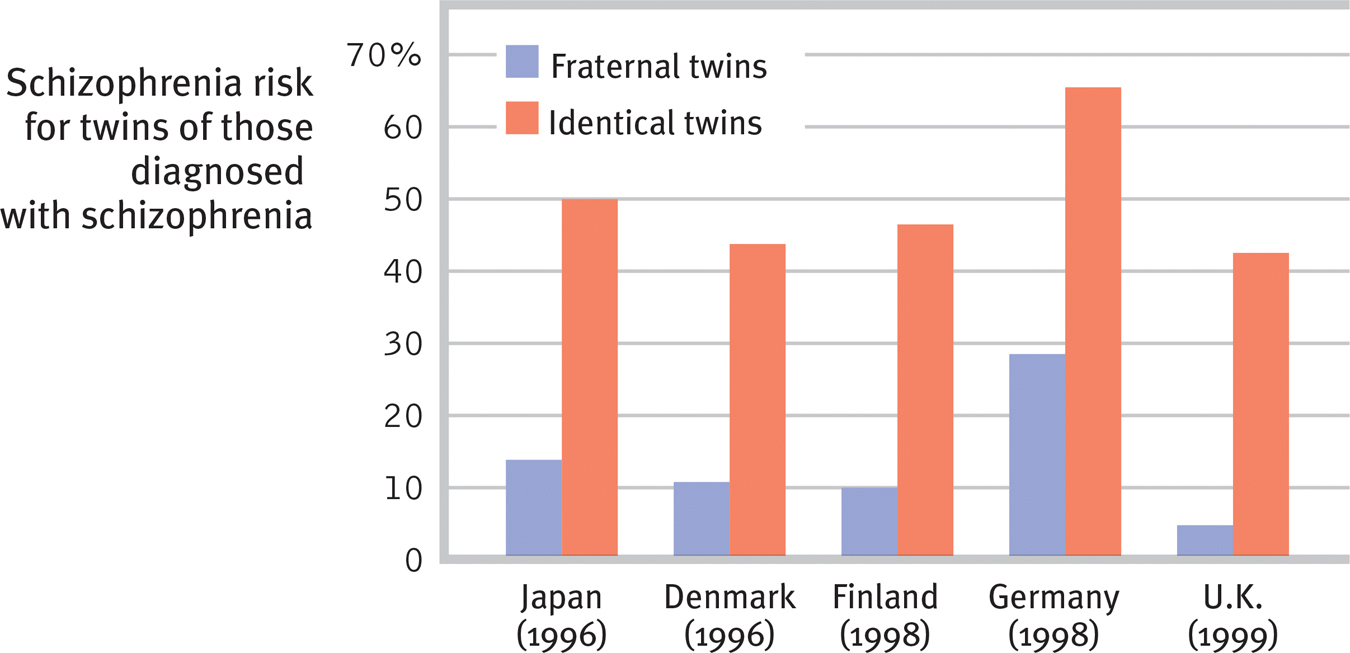
 Figure 15.11
Figure 15.11Risk of developing schizophrenia The lifetime risk of developing schizophrenia varies with one’s genetic relatedness to someone having this disorder. Across countries, barely more than 1 in 10 fraternal twins, but some 5 in 10 identical twins, share a schizophrenia diagnosis. (Data from Gottesman, 2001.)
Remember, though, that identical twins share more than their genes. They also share a prenatal environment. About two-
Adoption studies help untangle genetic and environmental influences. Children adopted by someone who develops schizophrenia seldom “catch” the disorder. Rather, adopted children have an elevated risk if a biological parent is diagnosed with schizophrenia (Gottesman, 1991).
The search is on for specific genes that, in some combination, predispose schizophrenia-
Although genes matter, the genetic formula is not as straightforward as the inheritance of eye color. Genome studies of thousands of individuals with and without schizophrenia indicate that schizophrenia is influenced by many genes, each with very small effects (International Schizophrenia Consortium, 2009; Xu et al., 2012). And, as we have so often seen, nature and nurture interact. Epigenetic (literally “in addition to genetic”) factors influence whether or not genes will be expressed. Like hot water activating a tea bag, environmental factors such as viral infections, nutritional deprivation, and maternal stress can “turn on” the genes that put some of us at higher risk for schizophrenia. Identical twins’ differing histories in the womb and beyond explain why only one of them may show differing gene expressions (Dempster et al., 2013; Walker et al., 2010). Our heredity and our life experiences work together. Neither hand claps alone.
645

Consider how researchers have studied these issues with LaunchPad’s How Would You Know If Schizophrenia is Inherited?
Thanks to our expanding understanding of genetic and brain influences on maladies such as schizophrenia, the general public more and more attributes psychiatric disorders to biological factors (Pescosolido et al., 2010). In 2007, one privately funded new research center announced its ambitious aim: “To unambiguously diagnose patients with psychiatric disorders based on their DNA sequence in 10 years’ time” (Holden, 2007). In 2010, $120 million in start-
Environmental Triggers for Schizophrenia
If prenatal viruses and genetic predispositions do not, by themselves, cause schizophrenia, neither do family or social factors alone. It remains true, as Susan Nicol and Irving Gottesman (1983) noted over three decades ago, that “no environmental causes have been discovered that will invariably, or even with moderate probability, produce schizophrenia in persons who are not related to” a person with schizophrenia.
Hoping to identify environmental triggers of schizophrenia, researchers have compared the experiences of high-
- A mother whose schizophrenia was severe and long-lasting
- Birth complications, often involving oxygen deprivation and low birth weight
- Separation from parents
- Short attention span and poor muscle coordination
- Disruptive or withdrawn behavior
- Emotional unpredictability
- Poor peer relations and solo play
- Childhood physical, sexual, or emotional abuse
Few of us can relate to the strange thoughts, perceptions, and behaviors of schizophrenia. Sometimes our thoughts jump around, but we rarely talk nonsensically. Occasionally we feel unjustly suspicious of someone, but we do not fear that the world is plotting against us. Often our perceptions err, but rarely do we see or hear things that are not there. We feel regret after laughing at someone’s misfortune, but we rarely giggle in response to bad news. At times we just want to be alone, but we do not live in social isolation. However, millions of people around the world do talk strangely, suffer delusions, hear nonexistent voices, see things that are not there, laugh or cry at inappropriate times, or withdraw into private imaginary worlds. The quest to solve the cruel puzzle of schizophrenia continues, more vigorously than ever.
646
 For an 8-minute description of how clinicians define and treat schizophrenia, visit LaunchPad’s Video: Schizophrenia–New Definitions, New Therapies.
For an 8-minute description of how clinicians define and treat schizophrenia, visit LaunchPad’s Video: Schizophrenia–New Definitions, New Therapies.
RETRIEVAL PRACTICE
- A person with schizophrenia who has ______________ (positive/negative) symptoms may have an expressionless face and toneless voice. These symptoms are most common with ______________ (chronic/acute) schizophrenia and are not likely to respond to drug therapy. Those with ______________ (positive/negative) symptoms are likely to experience delusions and to be diagnosed with ______________ (chronic/acute) schizophrenia, which is much more likely to respond to drug therapy.
negative; chronic; positive; acute
- What factors contribute to the onset and development of schizophrenia?
Biological factors include abnormalities in brain structure and function, prenatal exposure to a maternal virus, and a genetic predisposition to the disorder. However, a high-
REVIEW: Schizophrenia

|
REVIEW | Schizophrenia |
LEARNING OBJECTIVES
RETRIEVAL PRACTICE Take a moment to answer each of these Learning Objective Questions (repeated here from within this section). Then click the 'show answer' button to check your answers. Research suggests that trying to answer these questions on your own will improve your long-term retention (McDaniel et al., 2009).
15-
Symptoms of schizophrenia include disturbed perceptions, disorganized thinking and speech, and diminished, inappropriate emotions. Delusions are false beliefs; hallucinations are sensory experiences without sensory stimulation. Schizophrenia symptoms may be positive (the presence of inappropriate behaviors) or negative (the absence of appropriate behaviors).
15-
Schizophrenia typically strikes during late adolescence, affects men slightly more than women, and seems to occur in all cultures. In chronic (or process) schizophrenia, the disorder develops gradually and recovery is doubtful. In acute (or reactive) schizophrenia, the onset is sudden, in reaction to stress, and the prospects for recovery are brighter.
15-
People with schizophrenia have increased dopamine receptors, which may intensify brain signals, creating positive symptoms such as hallucinations and paranoia. Brain abnormalities associated with schizophrenia include enlarged, fluid-filled cerebral cavities and corresponding decreases in the cortex. Brain scans reveal abnormal activity in the frontal lobes, thalamus, and amygdala. Interacting malfunctions in multiple brain regions and their connections may produce schizophrenia’s symptoms.
15-
Possible contributing factors include viral infections or famine conditions during the mother’s pregnancy; low weight or oxygen deprivation at birth; and maternal diabetes or older paternal age.
15-
Twin and adoption studies indicate that the predisposition to schizophrenia is inherited. Multiple genes probably interact to produce schizophrenia. No environmental causes invariably produce schizophrenia, but environmental events (such as prenatal viruses or maternal stress) may “turn on” genes for this disorder in those who are predisposed to it.
Possible early warning signs of later development of schizophrenia include both biological factors (a mother with severe and long-lasting schizophrenia; oxygen deprivation and low weight at birth; separation from parents; short attention span and poor muscle coordination) and psychological factors (disruptive or withdrawn behavior; emotional unpredictability; poor peer relations and solo play).
TERMS AND CONCEPTS TO REMEMBER
RETRIEVAL PRACTICE Match each of the terms on the left with its definition on the right. Click on the term first and then click on the matching definition. As you match them correctly they will move to the bottom of the activity.
Question
schizophrenia delusion chronic schizophrenia acute schizophrenia | (also called reactive schizophrenia) a form of schizophrenia that can begin at any age, frequently occurs in response to an emotionally traumatic event, and has extended recovery periods. (also called process schizophrenia) a form of schizophrenia in which symptoms usually appear by late adolescence or early adulthood. As people age, psychotic episodes last longer and recovery periods shorten. a psychological disorder characterized by delusions, hallucinations, disorganized speech, and/or diminished, inappropriate emotional expression. a false belief, often of persecution or grandeur, that may accompany psychotic disorders. |
Use  to create your personalized study plan, which will direct you to the resources that will help you most in
to create your personalized study plan, which will direct you to the resources that will help you most in  .
.