20.2 The Other Senses
Our brain gives seeing and hearing priority in the allocation of cortical tissue. But extraordinary happenings also occur within our other senses. Sharks and dogs rely on their outstanding sense of smell, aided by large brain areas devoted to this system. Without our senses of touch, taste, smell, and body position and movement, we humans would be seriously handicapped, and our capacities for enjoying the world would be greatly diminished.
Touch
20-

Touch is vital. Right from the start, touch aids our development. Infant rats deprived of their mother’s grooming produce less growth hormone and have a lower metabolic rate—
Humorist Dave Barry was perhaps right to jest that your skin “keeps people from seeing the inside of your body, which is repulsive, and it prevents your organs from falling onto the ground.” But skin does much more. Touching various spots on the skin with a soft hair, a warm or cool wire, and the point of a pin reveals that some spots are especially sensitive to pressure, others to warmth, others to cold, still others to pain. Our “sense of touch” is actually a mix of these four basic and distinct skin senses, and our other skin sensations are variations of pressure, warmth, cold, and pain: Some examples:
- Stroking adjacent pressure spots creates a tickle.
- Repeated gentle stroking of a pain spot creates an itching sensation.
- Touching adjacent cold and pressure spots triggers a sense of wetness, which you can experience by touching dry, cold metal.
- Stimulating nearby cold and warm spots produces the sensation of hot (FIGURE 20.5).

 Figure 20.5
Figure 20.5
Warm + cold = hot When ice-cold water passes through one coil and comfortably warm water through another, we perceive the combined sensation as burning hot.
Touch sensations involve more than tactile stimulation, however. A self-
Pain
20-
Be thankful for occasional pain. Pain is your body’s way of telling you something has gone wrong. By drawing your attention to a burn, a break, or a sprain, pain orders you to change your behavior—
More numerous are those who live with chronic pain, which is rather like an alarm that won’t shut off. The suffering of such people, and of those with persistent or recurring backaches, arthritis, headaches, and cancer-
Understanding PainOur pain experiences vary widely. Women are more sensitive to pain than men are (their senses of hearing and smell also tend to be more sensitive) (Ruau et al., 2011; Wickelgren, 2009). Our individual pain sensitivity varies, too, depending on genes, physiology, experience, attention, and surrounding culture (Gatchel et al., 2007; Reimann et al., 2010). Thus, our experience of pain reflects both bottom-
BIOLOGICAL INFLUENCES There is no one type of stimulus that triggers pain (as light triggers vision). Instead, there are different nociceptors—sensory receptors in our skin, muscles, and organs that detect hurtful temperatures, pressure, or chemicals (FIGURE 20.6).
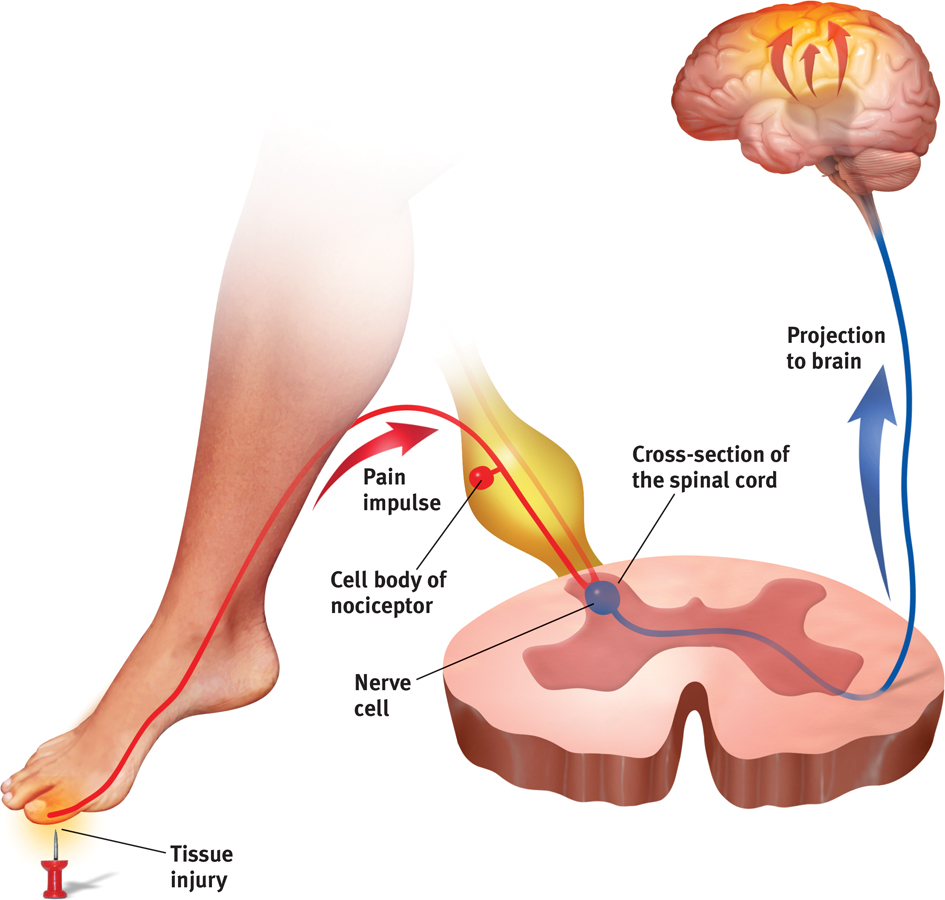
 Figure 20.6
Figure 20.6The pain circuit Sensory receptors (nociceptors) respond to potentially damaging stimuli by sending an impulse to the spinal cord, which passes the message to the brain, which interprets the signal as pain.

Although no theory of pain explains all available findings, psychologist Ronald Melzack and biologist Patrick Wall’s (1965, 1983; Melzack & Katz, 2013) classic gate-control theory provides a useful model. The spinal cord contains small nerve fibers that conduct most pain signals, and larger fibers that conduct most other sensory signals. Melzack and Wall theorized that the spinal cord contains a neurological “gate.” When tissue is injured, the small fibers activate and open the gate, and you feel pain. Large-
But pain is not merely a physical phenomenon of injured nerves sending impulses to a definable brain area—
The brain can also create pain, as it does in people’s experiences of phantom limb sensations, after a limb has been amputated. Their brain may misinterpret the spontaneous central nervous system (CNS) activity that occurs in the absence of normal sensory input. As the dreamer may see with eyes closed, so 7 in 10 such people may feel pain or movement in nonexistent limbs (Melzack, 1992, 2005). (Some may also try to step off a bed onto a phantom limb or to lift a cup with a phantom hand.) Even those born without a limb sometimes perceive sensations from the absent arm or leg. The brain, Melzack (1998) has surmised, comes prepared to anticipate “that it will be getting information from a body that has limbs.”
Phantoms may haunt other senses too, as the brain, responding to the absence of sensory signals, amplifies irrelevant neural activity. People with hearing loss often experience the sound of silence: tinnitus, the phantom sound of ringing in the ears. Those who lose vision to glaucoma, cataracts, diabetes, or macular degeneration may experience phantom sights—
PSYCHOLOGICAL INFLUENCES One powerful influence on our perception of pain is the attention we focus on it. Athletes, focused on winning, may play through the pain. Halfway through his lap of the 2012 Olympics 1600 meter relay, Manteo Mitchell broke one of his leg bones—
We also seem to edit our memories of pain, which often differ from the pain we actually experienced. In experiments, and after medical procedures, people overlook a pain’s duration. Their memory snapshots instead record two factors: their pain’s peak moment (which can lead them to recall variable pain, with peaks, as worse [Stone et al., 2005]), and how much pain they felt at the end. In one experiment, researchers asked people to immerse one hand in painfully cold water for 60 seconds, and then the other hand in the same painfully cold water for 60 seconds followed by a slightly less painful 30 seconds more (Kahne-
Curiously, when asked which trial they would prefer to repeat, most preferred the 90-
The end of an experience can color our memory of pleasures, too. In one simple experiment, some people, on receiving a fifth and last piece of chocolate, were told it was their “next” one. Others, told it was their “last” piece, liked it better and also rated the whole experiment as being more enjoyable (O’Brien & Ellsworth, 2012). Endings matter.
SOCIAL-CULTURAL INFLUENCES Our perception of pain varies with our social situation and our cultural traditions. We tend to perceive more pain when others seem to be experiencing pain (Symbaluk et al., 1997). This may help explain other apparent social aspects of pain, as when pockets of Australian keyboard operators during the mid-
Thus, our perception of pain is a biopsychosocial phenomenon (Hadjistavropoulos et al., 2011). Viewing pain from many perspectives can help us better understand how to cope with it and treat it (FIGURE 20.7).
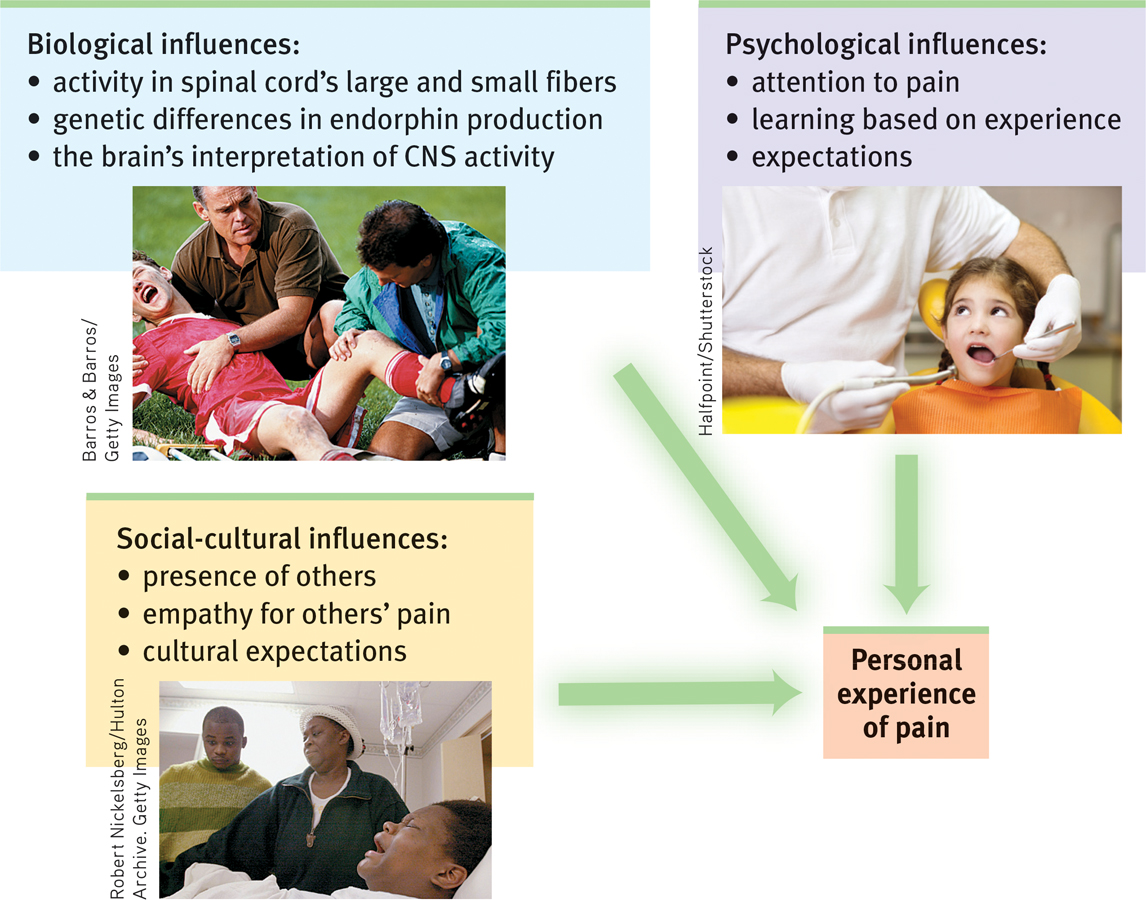
 Figure 20.7
Figure 20.7Biopsychosocial approach to pain Our experience of pain is much more than the neural messages sent to our brain.
Controlling PainIf pain is where body meets mind—
That explains some striking influences on pain. When we are distracted from pain (a psychological influence) and soothed by the release of our naturally painkilling endorphins (a biological influence), our experience of pain diminishes. Sports injuries may go unnoticed until the after-

PLACEBOS Even an inert placebo can help, by dampening the central nervous system’s attention and responses to painful experiences—
Another experiment pitted two placebos—
DISTRACTION Distracting people with pleasant images (“Think of a warm, comfortable environment”) or drawing their attention away from the painful stimulation (“Count backward by 3’s”) is an effective way to activate pain-
“When belly with bad pains doth swell, It matters naught what else goes well.”
Sadi, The Gulistan, 1258
“Pain is increased by attending to it.”
Charles Darwin, Expression of Emotions in Man and Animals, 1872

 Figure 20.8
Figure 20.8Virtual-
THINKING CRITICALLY ABOUT
THINKING CRITICALLY ABOUT: Hypnosis and Pain Relief
Imagine you are about to be hypnotized. The hypnotist invites you to sit back, fix your gaze on a spot high on the wall, and relax. In a quiet, low voice the hypnotist suggests, “Your eyes are growing tired…. Your eyelids are becoming heavy … now heavier and heavier…. They are beginning to close…. You are becoming more deeply relaxed…. Your breathing is now deep and regular…. Your muscles are becoming more and more relaxed. Your whole body is beginning to feel like lead.”
After a few minutes of this hypnotic induction, you may experience hypnosis. Hypnotists have no magical mind-
Can hypnosis relieve pain? Yes. When unhypnotized people put their arms in an ice bath, they felt intense pain within 25 seconds (Elkins et al., 2012; Jensen, 2008). When hypnotized people did the same after being given suggestions to feel no pain, they indeed reported feeling little pain. As some dentists know, light hypnosis can reduce fear, thus reducing hypersensitivity to pain.
Hypnosis inhibits pain-
Psychologists have proposed two explanations for how hypnosis works. One theory proposes that hypnosis is a form of normal social influence (Lynn et al., 1990; Spanos & Coe, 1992). In this view, hypnosis is a by-
Another theory views hypnosis as a special dual-
Another form of dual processing—
RETRIEVAL PRACTICE
- Which of the following options has NOT been proven to reduce pain?
- Distraction
- Hypnotic suggestion
- Phantom limb sensations
- Endorphins
c.
Taste
20-

Like touch, our sense of taste involves several basic sensations. Taste’s sensations were once thought to be sweet, sour, salty, and bitter, with all others stemming from mixtures of these four (McBurney & Gent, 1979). Then, as investigators searched for specialized nerve fibers for the four taste sensations, they encountered a receptor for what we now know is a fifth—
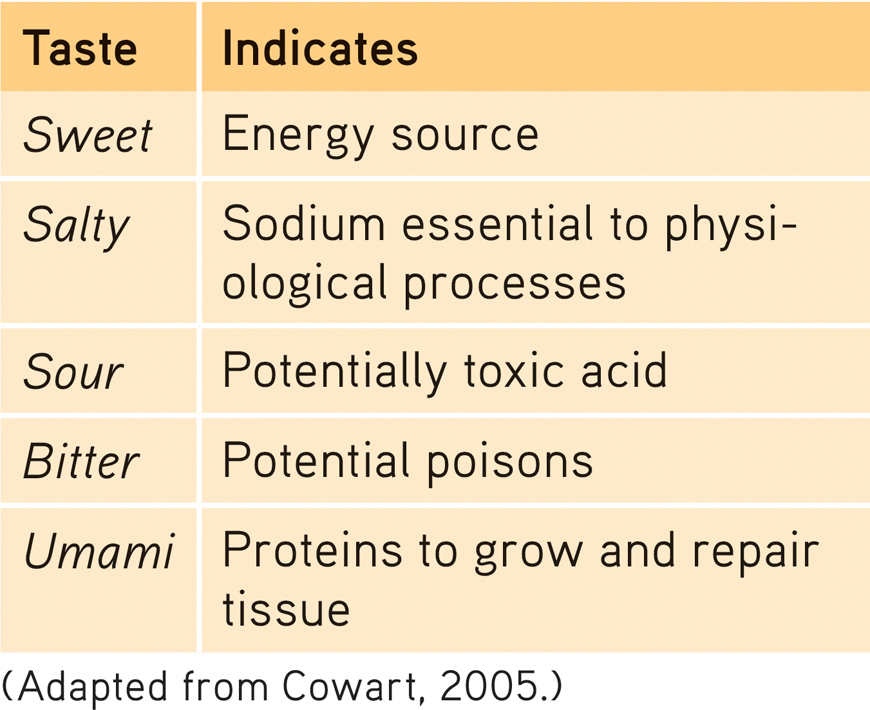
Tastes exist for more than our pleasure (see TABLE 20.1). Pleasureful tastes attracted our ancestors to energy-
 Table 20.1
Table 20.1The Survival Functions of Basic Tastes
“Life is not measured by the number of breaths we take, but by the moments that take our breath away.”
Author unknown
Taste is a chemical sense. Inside each little bump on the top and sides of your tongue are 200 or more taste buds, each containing a pore that catches food chemicals. In each taste bud pore, 50 to 100 taste receptor cells project antenna-
Impress your friends with your new word for the day: People unable to see are said to experience blindness. People unable to hear experience deafness. People unable to smell experience anosmia. The 1 in 7500 people born with anosmia not only have trouble cooking and eating, but also are somewhat more prone to depression, accidents, and relationship insecurity (Croy et al., 2012, 2013).
Taste receptors reproduce themselves every week or two, so if you burn your tongue with hot food it hardly matters. However, as you grow older, the number of taste buds decreases, as does taste sensitivity (Cowart, 1981). (No wonder adults enjoy strong-
Essential as taste buds are, there’s more to taste than meets the tongue. Expectations can influence taste. When told a sausage roll was “vegetarian,” people in one experiment found it decidedly inferior to its identical partner labeled “meat” (Allen et al., 2008). In another experiment, being told that a wine cost $90 rather than its real $10 price made it taste better and triggered more activity in a brain area that responds to pleasant experiences (Plassmann et al., 2008).
Smell
Life begins with an inhale and ends with an exhale. Between birth and death, you will daily inhale and exhale nearly 20,000 breaths of life-
Like taste, smell is a chemical sense. We smell something when molecules of a substance carried in the air reach a tiny cluster of 20 million receptor cells at the top of each nasal cavity (FIGURE 20.9). These olfactory receptor cells, waving like sea anemones on a reef, respond selectively—
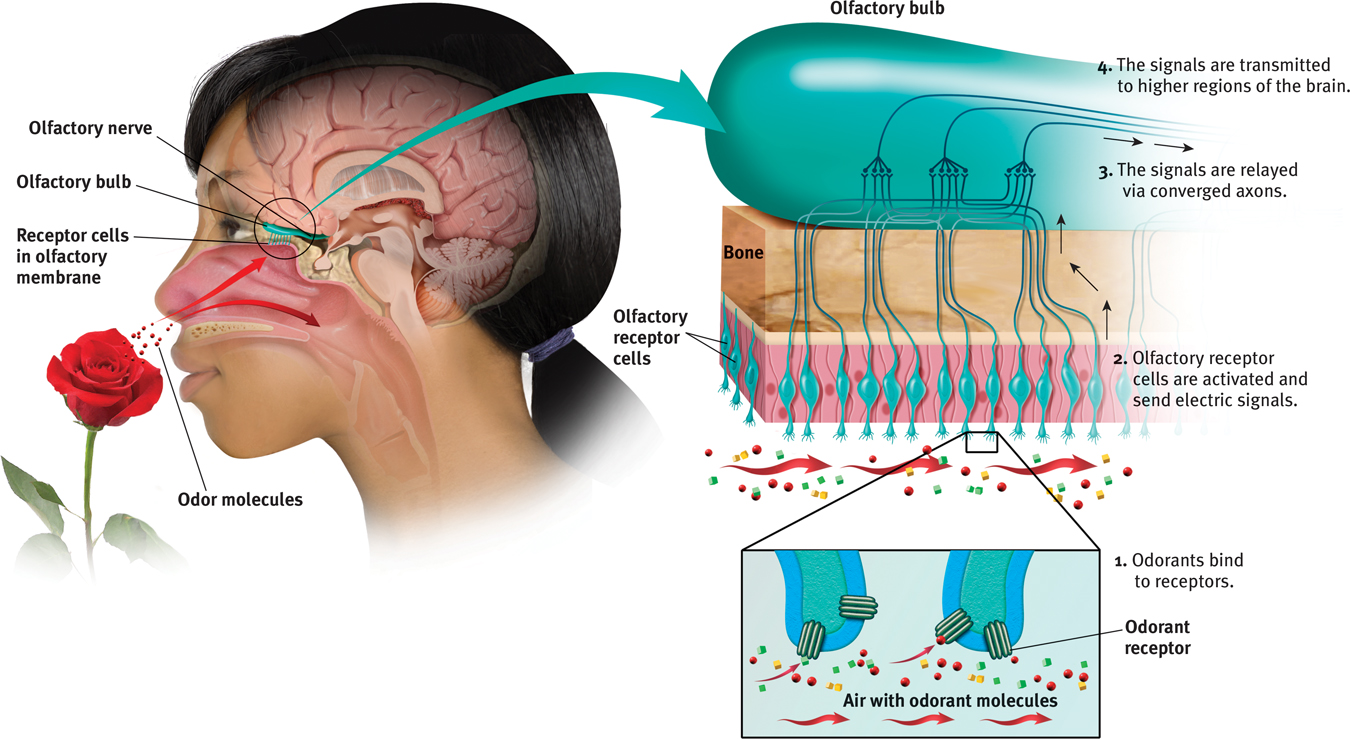
 Figure 20.9
Figure 20.9The sense of smell If you are to smell a flower, airborne molecules of its fragrance must reach receptors at the top of your nose. Sniffing swirls air up to the receptors, enhancing the aroma. The receptor cells send messages to the brain’s olfactory bulb, and then onward to the temporal lobe’s primary smell cortex and to the parts of the limbic system involved in memory and emotion.
Even nursing infants and their mothers have a literal chemistry to their relationship. They quickly learn to recognize each other’s scents (McCarthy, 1986). Aided by smell, a mother fur seal returning to a beach crowded with pups will find her own. Our human sense of smell is less acute than our senses of seeing and hearing. Looking out across a garden, we see its forms and colors in exquisite detail and hear a variety of birds singing, yet we smell little of it without sticking our nose into the blossoms.
Odor molecules come in many shapes and sizes—
 For an animated explanation of how we smell, visit LaunchPad’s Concept Practice: Sense of Smell.
For an animated explanation of how we smell, visit LaunchPad’s Concept Practice: Sense of Smell.
Gender and age influence our ability to identify scents. Women and young adults have the best sense of smell (Wickelgren, 2009; Wysocki & Gilbert, 1989). Physical condition also matters. Smokers and people with Alzheimer’s disease, Parkinson’s disease, or alcohol use disorder typically have a diminished sense of smell (Doty, 2001). For all of us, however, the sense of smell tends to peak in early adulthood and gradually declines thereafter (FIGURE 20.10).
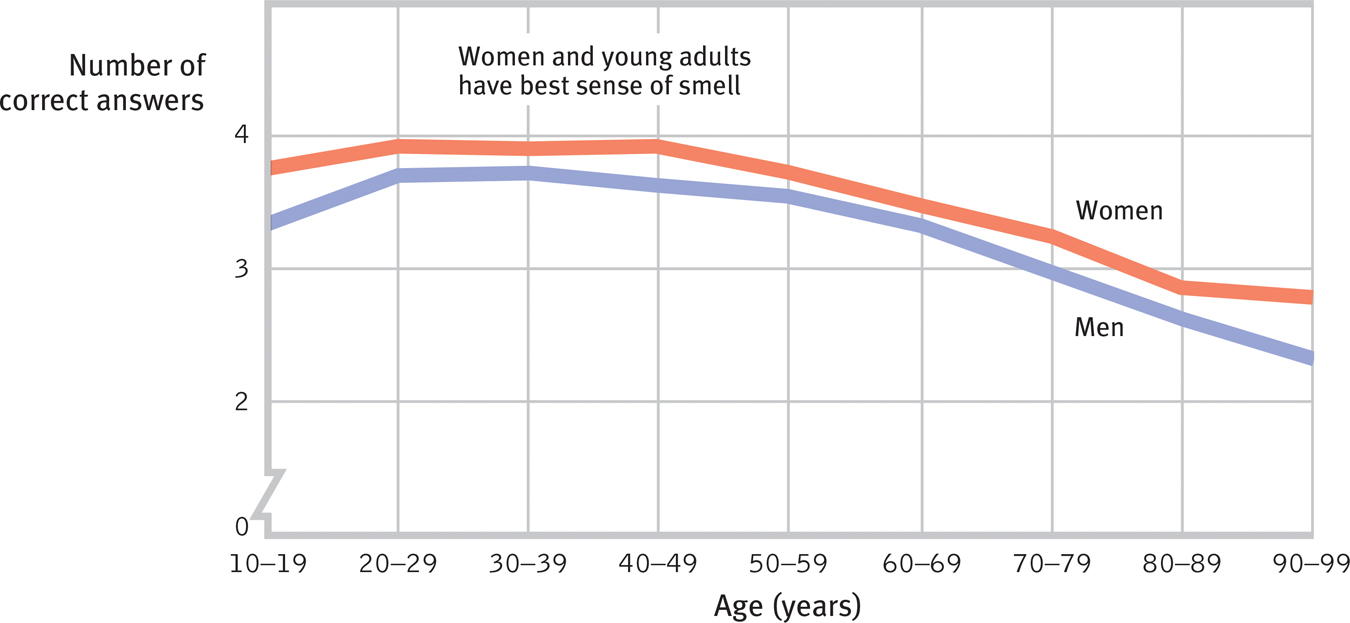
 Figure 20.10
Figure 20.10Age, sex, and sense of smell Among the 1.2 million people who responded to a National Geographic scratch-
Despite our skill at discriminating scents, we aren’t very good at describing them. Try it: Which is easier, describing the sound of coffee brewing, or the aroma of coffee? For most people, it’s the sound. Compared with how we experience and remember sights and sounds, smells are primitive and harder to describe and recall (Richardson & Zucco, 1989; Zucco, 2003).
“There could be a stack of truck tires burning in the living room, and I wouldn’t necessarily smell it. Whereas my wife can detect a lone spoiled grape two houses away.”
Dave Barry, 2005
As any dog or cat with a good nose could tell us, we each have our own identifiable chemical signature. (One noteworthy exception: A dog will follow the tracks of one identical twin as though they had been made by the other [Thomas, 1974].) Animals that have many times more olfactory receptors than we do also use their sense of smell to communicate and to navigate. Long before a shark can see its prey, or a moth its mate, olfactory cues direct their way, as they also do for migrating salmon returning to their home stream. After being exposed in a hatchery to one of two odorant chemicals, salmon have, when returning two years later, sought whichever stream near their release site was spiked with the familiar smell (Barinaga, 1999).

For humans, too, the attractiveness of smells depends on learned associations (Herz, 2001). As babies nurse, their preference for the smell of their mother’s breast builds. So, too, with other associations. As good experiences are linked with a particular scent, people come to like that scent. This helps explain why people in the United States tend to like the smell of wintergreen (which they associate with candy and gum) more than do those in Great Britain (where it often is associated with medicine). In another example of odors evoking unpleasant emotions, researchers frustrated Brown University students with a rigged computer game in a scented room (Herz et al., 2004). Later, if exposed to the same odor while working on a verbal task, the students’ frustration was rekindled and they gave up sooner than others exposed to a different odor or no odor.
Though it’s difficult to recall odors by name, we may recognize long-
Our brain’s circuitry helps explain an odor’s power to evoke feelings and memories (FIGURE 20.11). A hotline runs between the brain area receiving information from the nose and the brain’s ancient limbic centers associated with memory and emotion. Thus, when put in a foul-
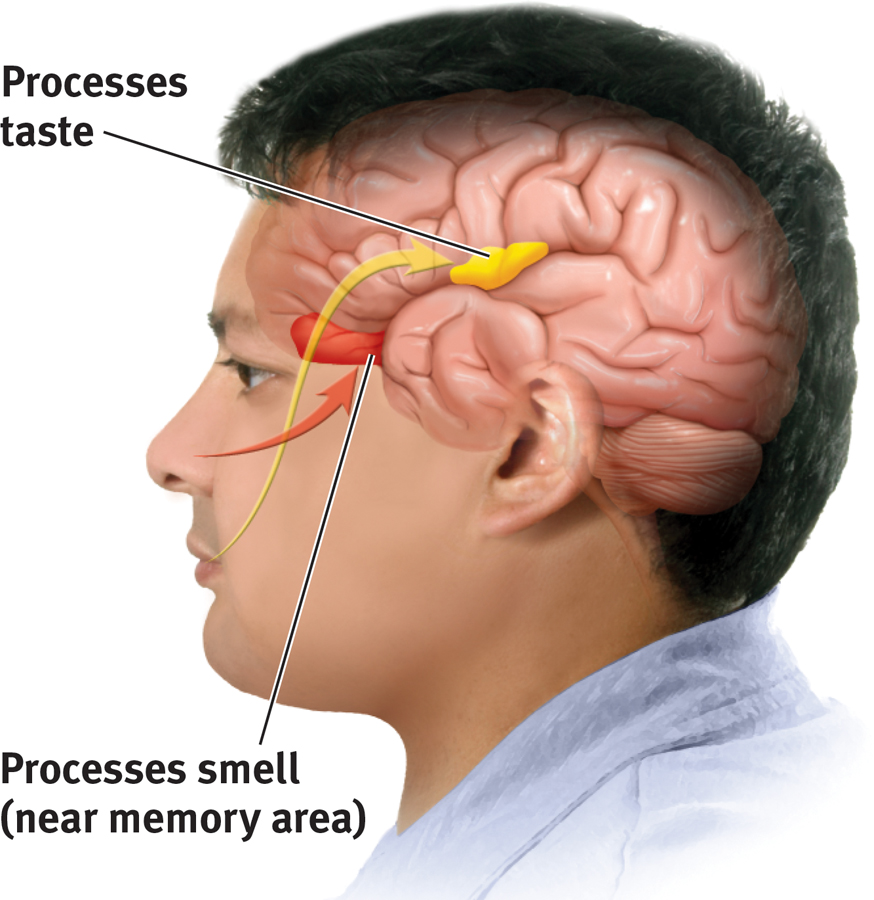
 Figure 20.11
Figure 20.11Taste, smell, and memory Information from the taste buds (yellow arrow) travels to an area between the frontal and temporal lobes of the brain. It registers in an area not far from where the brain receives information from our sense of smell, which interacts with taste. The brain’s circuitry for smell (red area) also connects with areas involved in memory storage, which helps explain why a smell can trigger a memory.
Smell is indeed primitive. Eons before the elaborate analytical areas of our cerebral cortex had fully evolved, our mammalian ancestors sniffed for food—
RETRIEVAL PRACTICE
- How does our system for sensing smell differ from our sensory systems for touch and taste?
We have four basic touch senses and five basic taste sensations. But we have no basic smell receptors. Instead, different combinations of odor receptors send messages to the brain, enabling us to recognize some 10,000 different smells.
Body Position and Movement
20-

Important sensors in your joints, tendons, and muscles enable your kinesthesia—your sense of the position and movement of your body parts. By closing your eyes or plugging your ears you can momentarily imagine being without sight or sound. But what would it be like to live without touch or kinesthesia—
A companion vestibular sense monitors your head’s (and thus your body’s) position and movement. The biological gyroscopes for this sense of equilibrium are two structures in your inner ear. The first, your semicircular canals, look like a three-
If you twirl around and then come to an abrupt halt, neither the fluid in your semicircular canals nor your kinesthetic receptors will immediately return to their neutral state. The dizzy aftereffect fools your brain with the sensation that you’re still spinning. This illustrates a principle that underlies perceptual illusions: Mechanisms that normally give us an accurate experience of the world can, under special conditions, fool us. Understanding how we get fooled provides clues to how our perceptual system works.
RETRIEVAL PRACTICE
- Where are the kinesthetic receptors and the vestibular sense receptors located?
Kinesthetic receptors are located in our joints, tendons, and muscles. Vestibular sense receptors are located in our inner ear.