Chapter 21. Can Depression Break Your Heart?
21.1 Can Depression Break Your Heart?

Read the article below. Then answer the questions that follow.
According to a growing body of research that shows depression plays an important role in heart disease, people with depression and anxiety are twice as likely to suffer a repeat heart attack, or to require emergency bypass surgery. Furthermore, patients who feel sad and depressed after heart surgery also face longer recoveries and a greater risk of death. Even a light case of the blues can have an impact; people who feel depressed for longer than two weeks, but don’t suffer from full-blown clinical depression, have a 74% higher risk of serious heart-related illness.
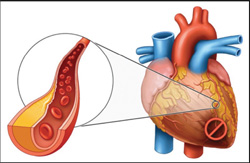
How can our state of mind be so physiologically powerful? Along with anxiety, grief, and social isolation, it turns out depression can exacerbate the inflammatory process involved in arteriosclerosis, or hardening of the arteries. To understand the underlying physiology, let’s take a look at the connection between the circulatory and immune systems.
Depression and heart disease
When people feel down in the dumps, they may eat badly, sleep too much or too little, and get less exercise. While this impacts heart health over time, research shows the mind-body connection is more profound than lifestyle choices can explain. Studies show a clear link between depression and heart disease, even when researchers compare individuals with similar lifestyles, omit patients who suffer from irregular sleep and eating patterns, and account for the potential heart-related side effects of anti-depressants. Does this mean that depression can directly impact our heart?
The connection may involve our immune system. Depression has been shown to decrease natural killer cells, lymphocyte activity, and other immune responses. Clinical studies also have shown that depression weakens defenses against viruses.
By the same token, depression can increase other immune responses. Chronic, low levels of inflammation triggered by depression have been shown to contribute to illness, including heart disease.
Are your cytokines sad?
When it comes to the link between depression and heart disease, a class of proteins called cytokines are the most commonly studied.
In the case of heart disease, cytokines trigger the body’s immune defenses in areas where the arteries are damaged (often as a result of excess fat and cholesterol). Cytokines tell macrophages to migrate to the site of a damaged artery and ingest the fat and bad cholesterol. It is possible that increased cytokine levels lead to the activation of more macrophages, and as the macrophages gather and become activated, they produce a variety of factors that can lead to further damage of the artery as well as arterial spasm. Fat-laden macrophages can also stimulate blood clots and scarring of the blood vessel, which lead to plaque formation.
Psychological stress stimulates cytokine production by increasing levels of a cell-signaling molecule named NFKappa B.
“If you look at a group of people that have a lot of distress and depression, you will see higher levels of cytokines and inflammation,” says Andrew Miller, a researcher at Emory University in Atlanta. “Cytokines aren’t necessarily causing the illnesses, but the inflammation that cytokines cause has been shown to predict the onset and progression of many diseases.”

Smile for your health!
Not all cytokines exacerbate inflammation. Laughter, happiness, and high self-esteem have been shown to help raise levels of the cytokines that fight disease, and lower those affiliated with chronic inflammation. Optimism has been shown to increase levels of a particular cytokine called the tumor necrosis factor alpha, which attacks cancer cells. In another study, levels of an inflammatory cytokine dropped after patients watched a comedy performance. Married couples have also been shown to have lower levels of inflammatory cytokines after pleasant conversations than after conflicts.
Of course we are just beginning to understand the mind-body connection, and more research is needed. Within the confines of a single study, researchers have not shown that healing or worsening depressive conditions directly alters cytokine levels, or that any changes in inflammation improves or worsens the risk of heart disease.
Each part of this article has been established by separate studies and different patient groups.
© 2015 WH Freeman and Company.
21.2 Comprehension Questions
Answer the following questions to demonstrate your understanding of the article.
Question 21.1
Studies have shown that depression decreases x7opDLY5KvT7Y2Z31ndfZhSeNeMJNco94plIX5vtknv5Q1WIvwoFoGV5HiSExzjTjFU0aC/8t9o= cells and activity of 0c5XLFgVbhEHK2P2UQFyBzm3fEabq3jlgPXEJUh0Kj7FcU/yvKS9ikCEj7wd2S/VWmKefQ==, in turn reducing immune response to illness.
Question 21.2
Fill in the Blank:
There appears to be a link between heart disease and a class of proteins called crj/lLWpGCSUdM6eDtQSwQ==, which have the ability to signal immune cells to take part in immune responses.
Question 21.3
kDlFpN/u/Ef2fXYF2s3SSg1PVhxKLOXAH/2mS4z/fkMg+KZf6e9u1h5yvt0DLy3nyXe8pY1mInq4a3Lfl8oFHUOC6OOZMbPgGn+dve4b4IuX1t/edWY10U86jmeozZAOKDWICUiohIkmHeOp4pHnbEf26xGoFOEqLufscqswiv6DFym+Psc58ICx55GPqDvwHqalIpKnFsQmaClBPzh0NEi2UgI2Tbv65XMpJN0nB3rgFFACozK+nI85WTyr2kSz+qzzc+IOSKq4cNsGt7C4Wn4iFFS0vBavqlQbT0b1604AjQJNxO/tWh+kwilQG7p00ndZxeRunOieFNjH2VwtRAGNpRFphqtOGL5kEa+OcVGJAWzcWZ/W6kYzAcTE48q0XSOYRUnLpx48cJgojuG0cGZML/V8xbCcmPzPCNysSgySQbgw04fG1B/HJRRKYqcnbb7LmSZ9F/miH47EuzoJFAGSdSEWzxGNCuMfXqjcf1bExs6qVUPZc/SdqWYE8DAYpXVwN3mVmI8nTsx3KnqIquF+XP1L+FDseVNtg704Io8LOpz6xVYi5jvljUeHnDCBTi+NJP2nbQybNLvDK++iSaIkvzCXMSmN2y9K/v4g6lQZx82xOUWHvN1a0eVuhvDZKHoHBRurlHMAPF/Eiw7yD5ZvqgY0H/TScP9ckGW3RmwWGDkMisngoEMvvqe0DCYlg3vWXg==Question 21.4
True/False:
Studies have found that cytokines trigger the body’s immune system to respond to damaged arteries and ultimately lead to further damage and plaque buildup.
l/z1Yl7oaTd5t5aAlzVI9g==
Question 21.5
M3LukXe2UM07dqFCj3EiKVYK+1iAZIJJGyVsW+cTLgVS6ZLMhqWb6G/oPYC3zA2EKoAw+0BrKPJ3IoVlfMC3wAx3cgVyqgOuo2T0uQgf0s3Yfhd6rpIzH/mLD6MlHWIzMRoEUV9MmC/ei90U823qxQSueEcC/0QPH7GsHIOn0j3yL0D8F0go2ENCAEVh8jSTB650GhrIX+jcICpw61x5wpSrDr6445een424vr3JZFz9Eah0HvNQQjUnkLobonRyhFTpqI4MPpPzfELkMYtatB3HwSciLy6L6dshtE6byRG1WSWz3vofQgPqvz1EEpdQT3QZ9G8aZrdAGSvksqbp+0dvD3U1tgouxIm2rnQIYTeo3SGlSP0HvlQ4UleI5AyAvLH0E2VPwnJf99HrhTsuYGQo9Poi7dscLDLZz1qRes7/p4eGx1N27L9blBdaR396vQ1ojUlF4Q49an/TjIL93lkzh1zzZx34tJMr72UKZYB02HQcCSb7MXPMopiF5Y0ajjphk8tSH4s=Question 21.6
Fill in the Blank:
Individuals with a positive outlook on life tend to have heightened levels of tumor necrosis factor alpha, a specific cytokine that attacks gl3JEX+j7cMcWwko cells.
Question 21.7
ueK3LuByW3YDnuPrbV9EjoOWwo9ADicQ7hDf5Bw7FSLubJS7IlG6QDGeBUQJ0uhoZkWEpdgoYDbfai9VnhPzyYpkWumVr8T8Ws1FaW5GgogWK8DfD7rNSwSlkBx3ew9x8sGyhyla4hpM4JSIwTvI5+QSQ8yj7NojzU9F9e7ZlaIwdJOOckPy6MJBl+Ivv3dA+yaueKcOxpGXcNyCEPXFJ78P8SuWPrpHZppcLAMJKDqilFT6/VODXt0q+yIcmKDmNtaXG0Wu5Sq+mwCIpm4MMGojtCq92tZxdygDwVLClVNmKPhu+lRFOKt90GzvSXl0TVgySHBJUucWqK7QPCFvxGnsl1aqzUEoWBHmL3nWcePIQiUi9irq4xA0428KuRsDSNEXhuW9+wNLuZblrK3F0eQQDPxC+K52GX/L7Vc5Yt20UDR0dNHCZVJ6rshbYLLMtOC0cHI0d8AFrSG6xo9+E3Rt2VpAl5//mZrnfjw6geLuFw7us9jiKwMGOueyEoLbhV2R39gdU4TfZRU9GJOUQVPUHYMk2FltBhS9sDG2jo8wNaOMMS/dtDxBkxHJwY7Sge7AlP1yyslcmx7PEMB/EetveW+BLYvr8OgXpKKs+PpLEmH5bo2efZTsVg/Ui+7R8lJvk9p0VlxE+u/9dSmX7Por2QMnI+7b7+hgcdPnGdZ+IK0zWqwBpB6V0NUkw2tGcuZujdnO44FRb9f/UlFynGeA9x8IEHkYfhowLGv222VS5RptPatCZ0/zdld8gTaDgfDyxMkrYzxaY2wAaPDAo8u2lvfPyQ9+gsWlh1hYZr0V4UOunZKq+GC8EkQX9Ns9U18fVoyRxBI8RS2braAs6PkwQhmJMGxyHKO47WsV7HuYvD81D/RJGSpmv1+/yh+jWlANYahoGxrkKNbel0am+Z3NyHJje5HcTR/uRKZYdx/gpLen9rn1xFjU8ZfuV4e7Vrt9U+wy2AY39xu5yJl8Fsx7Y3MJpkMdhNDXLJlalEtUNYrHYj7j5dwvFKXwenhz3y4Y+pHWYuvG0N7x8xiKm5pSs83BkrAKlKKTFnjVrC/d8fYhkl97MToUyh9uRltufrHhkfGNvSpT0xLLE/vTQIFRCv58TMX3zv63EiYfs8xYDfOxyfskAeOFDZy+YqRpoV6wazAJzwJf+CXlYOzHmyQmZXItWrGix2185F9f++un+0BiPswJ8ZTV+esnBpytTdDJcteRt4ZS8kdWo+FPnaTFFcKFTwIl7t4wNottlcv0V1Ns6pJCgEhtmCVCKXyB2SaOpTfv9fukRoimo2nfmNV8w4/DverZ1wBMBmJN3vDofY94y7Vzew2Eg92aCR1Fwc6pPGPpRqeltBKvxN6BPXhOOxUgNbBJ1TvAdH+sEx4ewg0ygaac7/Ru2gUigdtNVryfjjTglK2cMR46wFC+yc8nKnccO/j0iwT06q/PR5UNl5Ed5Ej9/wbW7yhnWAW1Z5t6ximAz1JBtcKWb1c/hypk2HrEaU+V8k1WJKBYaQCi5gJOlhv4au8jpNbt4E2bYLscZB6r3AjloxY1i2bDp04dbmL4HHrFCL9k8DnnnYAWlL73ZwXKi3B4oH4FdIoEdLCzW4eBo61TPKh5gwTAbqKDa57embdmCFmfEt59tcHodwCYbN1LO45MPoSl+igZhNaY3RayB4YSjiy8dXt13fRbBJj2HzVLy3wBr31uliLfOJ9qwzwFvnmvuaniDoNtXw/+fJh35ZFB4hm4qlwixyVRwcMPaNksdD6mqlcLjJFVXkTLKKV3eb1EoUhv9vquzvpq+/gtpZyTJmskQOw6f6nTAakUB4Gn6+sdi2dmFY1q0F0FvsHqSlmWZWTk1s0ZO/FDqPLRhPO1eAYP4ZQ8EZC4eVXn0fQCp94LNpuHHYfWRO2KX2bF3mBZVIa5hiTwDn8plyVVNkuG6ZKzo6GWTkBY+32+pmP/77ZKB6X5fD2h1YHHSj7mGA1OcRDs1ptSDFFGcSHEEF3VEPnFL0ID7kq4Mlxtb/w5An1giUGBAxDpWVGXSZJf31KeUICJqL5sbrMyx+ZuLiKx63uxRs/ys+5de4+Ara6j+JTL85dsp/hiGDhmgDGo2Fsdm2+9wT0WYy+iS+6ohvAArgy1UPTOJdZD6la6HZswMLgBo/SdioqqfJ0tQuestion 21.8
55mSjWgSZCDVdkA5AWpNZCtWmZsmApqZFNyZfiqm5kEZxabG1XZFSjrt9zGl8h7/L9EPdq7zqEmNmIG8OFLrjCxMc1ZM9rijxurs72jr5qAKXiFA+qU795pDO4klHxvx3azfcG24JSHDQT1C5/Xdj6IsyZWLvSmTyVCxAmZw1CLOz6UkgHX3rz1whP+cv7IvqaA2uuF7bA1d3ztdojqoL4Y1VY/X4+DdXmiyq5gmp0zm6E57u7X0f1Q54BeY0z2SVZuWPawufzK+Gj9fzFXMG7pC8jej2JEwo2HHnCvvya43XHFNdTVIotZOkxGt6a5yA8MHgit7iqntfcwfvfsdKeFqxuQUU26MNWNA5P2ODg+jFrnpb5GcgM+zYko7gpqcjw6FgsvII3pLC7IYSbjkxp0E6UfWJpf2G11s+zODW40s2kh7MV8jBFBYeHmXZtJkmKS3XH4aWG9UCKdgdxW7o9x6oyoxUqgK/meL8M+vw2fU8owBfY7qOlQegAiOdkdq8Z+8Ar/uAmVlotuOVd3vOT03dgRCrQCws8s3oGhYnBo1zNCzeJrujJ0r0LqjB/oKj1FD8TA+85u3dLoZu416Nxs2uU/Ggu6sOguz+pcAjl9uO3uK4FRN8ttr5Br+Tv/YAv0RV9zd3Xu/emxGzQ1r2fg2AZr26Dl3w6iMr5rR+5woMrjsibNlvjzqVfUUWNfPgeZspGu8H8i+W221CnPjrJNzRiKnbcj3FLYHsaVR5B6ykia/tDXQFDMo4M4LFJfTvZukWgQceJQIlTs6acmy6xrPwfekfnbXHNz6ZTR3zx7Q3+Icb0jkT3EjFWd+CqomasRwgTbHpT1rzTDnuOBL93Zaq253IMgBS4eMhh2kHvrWMMyMRrJ/xRe3yJmRi6gKljuhLI7mbKuH4cqSeNaopOS9CLKnR8fsCL7OqJYErw7mJqPnsYj1kpy38jz3geknrllintgDE2Od038nLynIciqzhbDufvcm04uIbLACHLWA3hsiIqnu/RAyUCZ9K1BCqgkstDa4fD63bgFrKu9sYCXUK2sDQ2IGh2a3KBMvMu6OWoJ/xhXjNGvKWztCnc3uGnjeDH8YDbgsDWuWGLvcF1Kz5ME8f3Sfpfsyax5RBC2g43KdRVi8APOOUCDC96kWN43y4FFJotHMUpif5BNITY+YlwHaVyzniYb4jYTKYiiE5Q+hgpwY9R7AM4d+lfcW758tNRYTBsexqfYyA7jIZFP92uIZz0trv0wtkRacnOQ3eoSQ9GBpChyb81ZW2opqFRAOr7V6v2omlLeV4I5yaBkpEFuJTMLupa+MOwPBbKKButhOX/tyYrPpt42JABosMQhPDV08WvmBL1mf7WgXUrj4Sr6ae9eCFjK5A6fLGZCL5fihc9BW2N63Aq9uoB2UJqBL2+pv5EK72kq1M1GXNZ2lz/iUOCSiVXIfmezsDOFMi6VnZvOcgsQYqvtUeUC02DOxizji/KvqZTIDmCVuKcLByAviYGeSFabRt2gi2+SBpw32qEG8x27yLBT9Ty30csyKyhewkf+xa5FZmx2G51ThdXHxrMmkmFinoIexAcWRC5FZP4XY4nSLlW+2R+MkI075CA501b5faIG5Xm1qP0aeEDtXw9RddYLbElynnshQPkwcqDy6VO2Wh90ak1TvYXCc05D86vsAURZYVe/dBqtFg0PdlYR5O6+fbvdLOTnWXAlyJFcuITlyq7uMsPKn6wvE4hSjFRd6e7Q9Qqm1EY7CMCzlAFX6Question 21.9
iGs91W2KamgAXJkWNKWRXHj/drkonyttrh7PzFg7S7y2D6wPNhHW2SvLAC5kJDgINzvxOujp9yQw/3/lmhMlCszzG7zqqaHaUrQLMDP5VVVjQNmKCFJLuR5TryK/EgxClrLw9/meOwCJWVpmY4AT9DDvZhDfnqowe0CW8uX++7vltAq1PMc7byJmG8pUusByk9Sh8+hcpPqjKAgyGVp+pPYjVFHy1fJHx/wb3rInbHMn2Ct56eoYFHgNNxeqaOzc+EKhCHKNh9aMgKBy5l/pr0fyxkoLAn67qfuT82nKZz7h7VwOQK1/CnOJnxnAhi7HCinLvV3OCCSGdBz3bFj8/4/FEHGvgoyXsdyoUTrGB0ZUENNXymw0Wov1UFyrVJnzvRaSSVpc6lLl68ntwBFiu3hf09oBUNiU2oCWrN20gWC9oD+5tMpK43cPQO6wFpZx4hwMSlGp8pZOw0YxYF8y4p43uqrUHch99/aJ7U25KtZp68VGEa2wy6SO8hb1UUIHpnxLlx1g0hp5SUiYUX+/JN1XW37Qa9ZMTSt/XL7sMQ5PNHPbGtnujsTBwaFHPeVhjntNt6sgRlwQ+9tdLrZZ0yz/pskzPmCPdY//PuwbZrOQQfpFrwYLqgfx6rSeZfH61+NWVkS01jes4T+XSdtqeBVfuHDMcjqvSDGNZ9qeEBEDLSFG92O8T3POXdDhzrcAhx71R0Te86xRJhWQmBr+GC8JNlgqAtUHjXBRY9svPMtM5LqHgH835Uxulz31ZI4QkYWX3UxyBBhifdgoa3OWNTDCLMdRL/1g/QJ8EjhcHvsLbYeQrXWjbRW/Mf7k9Qyv7K2sLMlWoMH5huIb+BQ6M0HyBwmFX6YORnVTbRWyCbKCF6PBn8cs2dSfvZSwH6+ukFTLMtOEgAehSlBgvLtOIFQoksTdsO7IrQsmKMLYPNv15Tmj+F6Y4NmD1j6EUN4OmlFcnL9P8lDXyL+k+4bCx/WOvvIk4M/khrQvjvWOzGo5IXXSeJzRkTyVCmDaUIfDWT3IpF6gM4/eDZJrwTvi6bry5G+p/L2emO3xf8sJQbRW8W/E3ecMRtCTb2FtpZXtfzbOkqSyBtZwFXLX7++HI9bO6dU1KDxY//yqvbYn+yXFc7Rg4d2y70dTImbh9ickKP3N3D5pSoPjlHpYQqWHXgiiUpB78FyaFzQpJ4zYA2f4lZhGMnoCAVUeB/AmUD9qX4VXL36TJ8mwArhOh9PP/wKimpuZs4Vyzq0JaPQPkZ60AFiOV1WREovKaZJbP1Ez8+VUEPgwyo2DiBTyooDKJKLaI9tJKm2x/t3g2ZlN3FYz2bZDpDMxwW1VU8SA5rb5ZrUW37fodAFYHZiuxq5ETvT2bKUYDRY68i2GEwm6O/3rdV/S9PN8VPd54v7A9QYnliAaN5ICO/E9j+QMrPdQ+HHDbBwk4B9fGncSewjkI+lo3BLQcuiUQM1oSxEPiuPM4VsFlKeGsz67yLjySfjH2EP+ENJ5RZ8NqZOSQ+nZOAwXB9F1OfcZKndauc22mE2tujwT8/dsCNoyQdgphFlAWgGkmqQVPtC1xH8ltpoNi62ZvSsvrfQEtb3MPWrAjwGR4YvfsVnyYS8K25WrJFY+OQVP1Omx9q67TOn8QgoAcark2CdltliPVZiC/R4YXZxyzfi3/KOUHpeVAxTQW0+mJZ9dInzqxx9Asnqlegn/ZBCCr1o4UKqbnGCL6IjH6DVXIOtkdI58WkBQ96cYkHZ1hLNpiTsuC/aNxi3zGnIANpxMGS3M7GSKGbRTgswYuCm4YMquZdwHCesgHojAPUqHMysRMQFciYkhAliCgL3RZScav5n48gGFfr9S8cHLsy0mYmgfzYNhPHj48yTC+cBNR2PporbJUt3gr8IX/LHy9tkhsscnL79C1mrUouDY4KZ2symHqn0GrrrW2xQMRXmB3TAGwmYxCR9aP4ix3EHco55p+s4q7ppBnB1FhRDSrTL9bW0ovpHpGa8a8yNUXg0TeXtJ1xzYgmXAmvjhD0yLeTOOj6+JD+0ptByl3gTnLPRb+gtrcl1r782vPCNBCqNc5l6vMZqeg+DnfYU8vSYB2XYc/Cl12GwHHCTjekzNlndBY94Gi/KW8rMA4AqzmPQgOcpXOO9JK/PDFRZL368cZKRoOlMrjWOpoUz4xgaZc42MuOIhgk05k1EkN6uniCg98xUBhcUmb2gtMRttuTJMSJqNQTMj+aAKg5gHx0aOpA4LuSA1Ve62z+ZfLjyE/ip1qz4GBsx2lDxQBOsaB+FCGIKFPIPmQkGCqEJcC0OuruL6Question 21.10
aZmSiHomAmRFqBe/Fcnm3gPhEXWo0J+omrmanivdeDD5lAoJMloHyRKzRqNYPWvGcM/CouDPkcbvpYiU6u9A7K285XfPGQISYK3NiHtY89dWJ+4NvXKqy/0mJDm6xHp63rSCWD8SfiLEHKgLrIDrkU3wlfqQpXAlJaj2VpwAp/UBvvvy4oZOPhkkWU1EDknTEn5WbtwowCDH5E8sQLQX1u06QsfgD2ZzzZL4JQdCsCCpgI4KZaWC+qYONgI7Z6TGMqj4DtNzvOJufxZtz6uGsmcZafotdishdvAN0hWUiEGRCtjTaHM0P+6Ezdn0GJ5EU3BycsNkvk2cU00RfNnOchXpD5HoLRPjTZGm7PXBO74/LHANTwy8e5pQJti3Mm/cSue5GhzIWP8ORbTsLy2zv4tmQXJeIIxUG1fuxEzV0YVI4v7BYHarisNkNFFaJ6IDTzEZUpQKlCrBDxqamQh1buwhebK2ix0Gw02dNq6U9ecL6cjCfRkpdKMXSlI21ivTHiu2+VB4rUXXTuHBhkmYUb3OzGDQdt0utdCFqtL63xdCC9hTJd72ICZayvxsO29vSjn4C5t0rC438mpPMe5uurAIQcJMqDqfdUYWXY1fFAdgctRlmlatP9qWIdJheA/wU8JIcrDFX8seSehjBs61bqZh+1mK4DCDq4+h0Zs3BtmQDvCA5qEhK21sCAGGjK/xd9U9H+vai3CD508wekdG98Jl6aVB8fK2WOIMn5YiL+pI/8rfFCVEuyd87Z8ePtCaxR5QG2fpYO3qZ58dLUg/B7PbC+IsoE3UKlctd1dI8iBgZs91IR1t99Y4BUK3sRlPpY30SbAzKyQBbBzivf3yAHA5y2VQzR1Tqqr+fMiugGHpzUBzg74WTIVqmXYVa24hG7voviy6p5VTy3/xtpcWEJgS7YkkKsHEw5jEJYjZ4hb0Q77UDRV91Z8EoFEPNmwRTzjAlypKFFIVS2ASKlfY9QKyXnkJ/+hk4xjvJuydcxn1ZlfGO23XoEImey+9/vwWLRbcZjqWiX4iriv2BQju1ONRKfIbhmdR8OAsfoTs8QPRsro9sO4AgvNZLxXVVo2ZjLsY9rT3VbNhPNvw67Vl1ftxkoQqBoiWWiV0mTacjFA85JZSrP0wTamOT2wEmBQH9TIlQrgPqDWl1jADvatX+s8PwDq4ZdU75e57pHKurQSx1D1azaIlff49/yYgGTjHb7vg3GdErBYUlqBLxrgOPQ/kem7EbFua9l6HR8XaXhGhSUfijnKBMcU7VnQCXlmj5igrWWKwy09lfMQokjNXOHdUjyy02+2A90Jgn8dE+H/SvAMuV+6rT4THcYbnZTWBZsiYMhGdIpKfWoiYHa/zUdyXM7Dtwx8JGYNR/f/rDuChBwyomgXRj/vY8vEFFr7wpvYnLV2MMW3TrBr+h5ebvVmlgAE6hmSg8hjH4Xzxn743v568+YaZXzxhzyAxHDRbJ2k8rviTvBaDAot9YaES1MlUFKwnSkPNR68lS9t2UBVNsxXwzWsR+i59SUYyjKLqHgJUkWjQ3qfKTQtdgOZXmG+jICERAG295C1/TiMuGFNpMsA6Elb2VVSiAgwrnRFGdliZGFyq0/f5TeDQSL9zXx/A/QB/w1QW7nLLvNW2bmCx0huWOw2tfynMPTX9NJD3E9mYUf20eX0l2HHBoyJNe9bQEJD6/48U0SEprHwO0Q5blV9c7ptWeUidsJ5JQo0SYBUu6xy++UBd7XK/JVDIqKiWqYzejiLhYQs4EtnY/CRazPLZgZwrxQC6rv7V6Z98tRDDqrfbTIaCGyQNqc64eL3YwtpCiA7rEbKtgSi4rmYBe1z+4szU0zM3yD91h/uniaIyYeIPmWl7PLNaMb24hCMwgzf0l4WId3gQZJ8bmmrhfKlARtQ1FNu3dxWHx0WJv78kYBkwGdKl2mKKS52c8eKW0cak37X/iroL6F2kiqr5Ky39r+CR8tkUXR9A5k7KFzoI4FnIevsoLCT0MZABZNIC/5vEcqDuTSBmGF+qRJQxL0jHNvvsk3WLAk/mB702a01/T6HOkiimGhy7Mi3SgV+BWoPd1lp7ZUqRHBMI2rgthr649fioqMPQ6t6JUJjSiJC3kYdiS21XLnRHW6a4u0yGGbp/xZvYf/RtSPAIJwZQ5V36FSPdgc85aqNrvQkCRze7R62a5u+NO5YyT1yDmiYMAWpWrbpBWttQtG5Oq9I9T2XoAIibDqAMt3gb2CTs6/1x9kinqAqjlQZWook44GOi6Y3IjflIPNH0d9JdxaEzXfWHecHSFOoYhmcpcYNDl5BV09Qjo9WlVVPVv3uWyuV5WX1MNs7C+BSHZjimJTpccj3WtRNiyFeFtekvlMYthdfPhHi8/PK5uSgsIHIn2vJccsPtLqmhswHE5ybPxGfEnPRNRRQmV/dHONjAXAOBO/DCiYqFJhvglnbDcO4kgHFHk+ytfodO5NrYS4HPlfF6f3qWXkaCKeiL2oyuWof6kDtvz4wZcCm9GMp+pb1orN86sS5YF0OC4SpxMtJEgkUuOMi3rRzogNYQN/1hpH4jZ0JL83nPsb3MRpO//Cvf7fAdEzP2orECCyPMnscGRiFXcFOrl9r9cfCKLgssPlPN7tXBoSgiD2Eaf/I5mIlqSXcnedXawW/9KFUqpFuRIBemJHCyLIig6A2MZyGcCSgZ+yR7vkVyNeHi6w1kLi49buRxwU30VFKqfrPsNDzU9wMYcDzQRlLn7ua8G1XGmUlVKadKWTiKEP9fDY5h6S/696LpdRmbJjuLc/1oRZStoD5YDTwuw/J01s3hJaw+QBXMeI3b58KoJvdmlr0J3La0IoXl9av81Au4LVybNkyOlTrzJzPAJxfYqhgaNeMOYJTb6tGeGAPF8Ku1834tG6Eqb3d+2X+/Pa+tUqN5+RdHjNBtRQjMbnJOQLgLYz3RuzAniA1V6CvIiS/KPg8wHZRx0SP25Jj0owqqvG5jj4XEGfhfMUAt6ui4GTZxz4Vxq+sW7F/DBMKrNrL+KjKBOeiJyF/Rp5VAx/k+I9zicekfZ53CfIzTVeoa5hB4ML6KLJzt/gTN/G7WwT8MntMOuJHZJdLXJZ26nS8qW72myqq93NYqP6c0E5iyCs7wx2UIiMAmVqv3aONOPnJD9rfL6vajHS5CJwTRRgNHa6Ef2wYhZDBHYIEmyH5w2vjBUaO3py4V8wCH6CYkOumb+bHNNkV+asV64vAle2d5K3A9NmoetqCwbGMfpyjI7NyFpS9843vJzy+TOEAd8RErJCvHaO9KWg8Q7wJ1MYjPeZV16YfLqtGeNOmJKdgu24eFXv/DMLcC9AgFgoZ54NrQXaJgBFndyqAOtehIMGH29w4/E6A3DyGuXIWOxYxbyKmirmCgssB4c+Mq81BtFunHrSEvjXaDARzzdWwrJnIPJ3btg1fzN9k+NwuhVfoQhP2jMmYOl1+Ed+vDwrVHDCoOJxnguwxzE5fDTxtTbHNcOmRwCNf5L4rj11jJEdUuA0HHdZ0uYn8VMtcXg9HWPy98pgHXGI1E+noTRLFVJP8cLEzw0qZ7ZVNA3kVTrtJttOd69iLBXQYkJlMe/x4PzmcfNXOqkq3aw9HM0Kj3NmoMOLe+X8VNRO+VjTde2J4yfbx/wSZO3D8/zRNWLs8YAAReR0NX0rk4cp9nx6TKzjQFuo1uo94yJFpdv/cL3UBut1ue/Tmg8/ukLgO56uYp/HR+571WG1MHp4f/oyStFKV93S3B3v1h8kxSfoxTPNP44DbA2r2aNseqO8OrNb2HpO2ub+COHaHEFJ+ndZiux1n5eyIDSyliOjBTAXL6Dc16qUv1qOphk2y/+T9X0snpj/lZM0klCHrYnOJyjhX9hSffvx3HuxHFpZHpONKov1d1khHHNxyCs+6JsCZA3DWFd48xlKDBQgWYXMSttc5mA+kIYrFFcQHT97ZEaj6/zqVJBzBg+PMmWLxmUDowXZiZWuUu0LJG00El4Zct/8oHKqzne0KfDgdjagiBSMpr+tbBusC8rJ/l1OnV3cH+jELBPn9Q0IsKBxxdqj9cl0XmuQDY9PdAE2wYjg1B4N8NA9NI2amIVj66zIBmlZnaDW38l+oVUxRw/gButP5wtQB4uXTBdV/mUcez3UPfAyjMGmKlzPYIL5PwC2lyiGXhI3GabaAD7I36WWCYsCRzJuCawmpz+2iVcMBJp+BAtWSEnGMUeVVSoHdKAftF3KJ1OG+QwvhOuHv+RYL1v4f4jM/KX+uszT5nzCwaUVU1rDGtQGnENDJhUDjblB2cboj3UaZsNFDwKpujRwcP5ehdpqIqHIFBmjHPb+ulNToBAV3cI7dvdswYqgst9ZiR8Tu+uB3LtRJfqWrm2oDdvnle8lFpLYeOHlf18MvA57LS4WMXFsjejAyduL1jZXWFyLghijEr4ueg5+xUITCUBifSY5ww1QnlOU2FVqzQF6xi5itEtF2u0KM1fY2ndTBoF+JDaBaTHLYRjzCCActivity results are being submitted...