While we don’t notice that our non-
1054
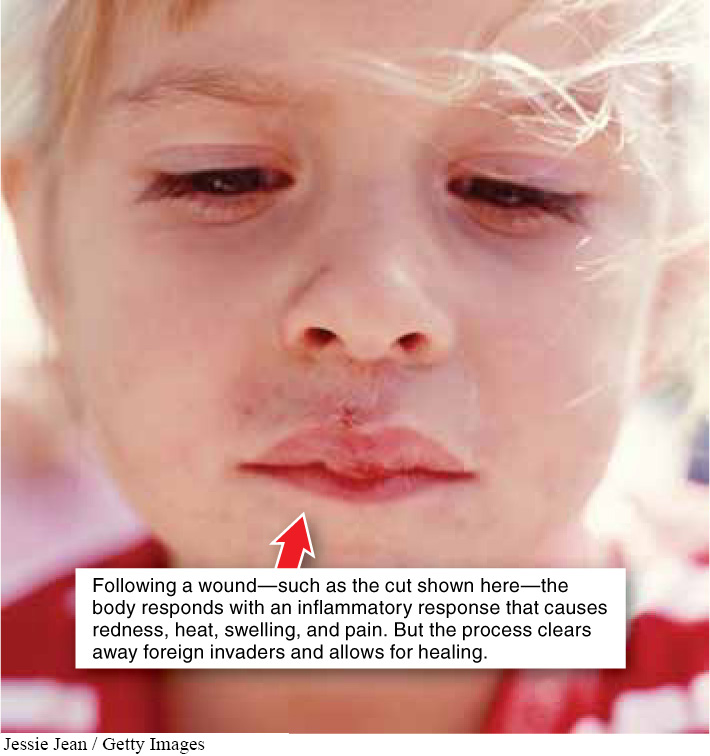
In the first century A.D., the Romans first described the four signs of inflammation: redness, heat, swelling, and pain—
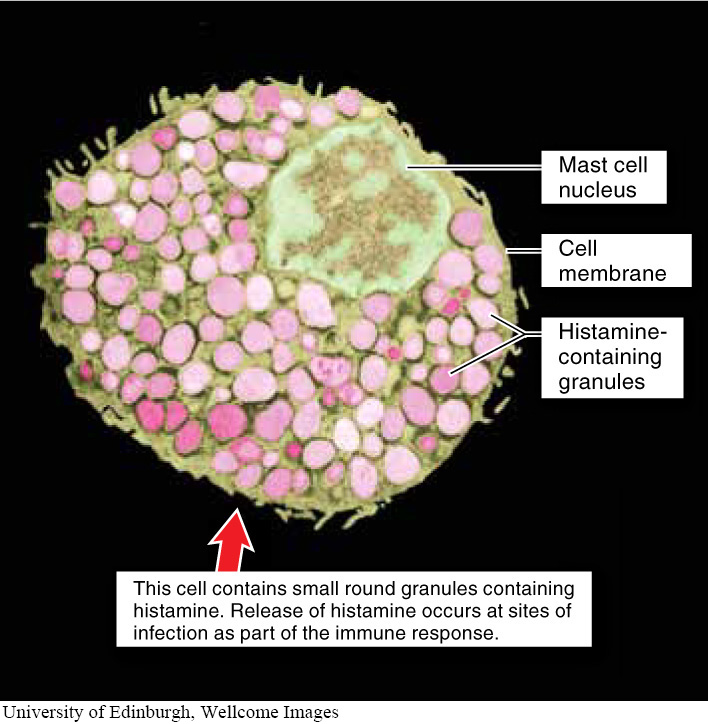
Let’s imagine a scenario in which you cut your finger with a small knife while slicing a bagel. Three quick steps happen within a matter of minutes. First, invading pathogens from the knife and the skin surface are quickly engulfed by the macrophages that reside outside the blood vessels, in all tissues. Second, those macrophages release cytokines to recruit more phagocytes to the wound location. And, third, the cytokines also summon two other types of white blood cells, which initiate inflammation. Basophils, which circulate in the blood, and mast cells, found in the tissues (FIGURE 26-13), both release histamine, a molecule that produces inflammation by causing nearby non-
When blood vessels dilate, the flow of blood increases and allows a faster, greater supply of defensive molecules and cells that can fight infection. The increased leakiness of the blood vessels makes it easier for neutrophils to exit the blood, enter tissue at the site of infection, and begin destroying any invading pathogens. The increased blood supply at the site of injury causes the redness and heat associated with inflammation. The leakiness is the reason for the swelling, because fluid leaking from the blood vessels accumulates in the tissue. And the increased pressure stimulates local pain receptors. Macrophages and neutrophils then begin an immediate response to destroy pathogens, and they also release cytokines that call more immune cells to the infection site (FIGURE 26-14).
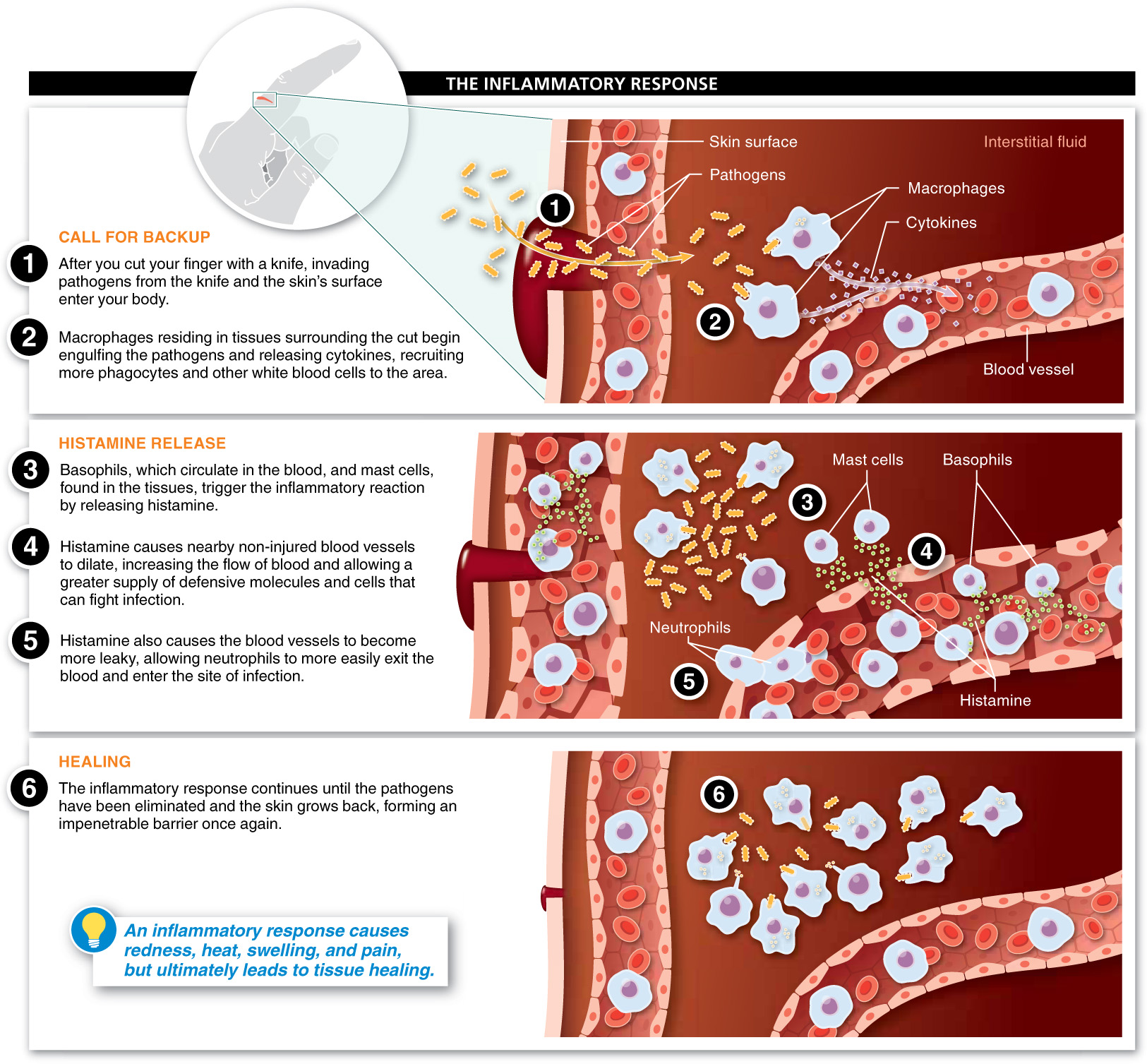
Complement proteins also play a role in inflammation. Just as cytokines (secreted by macrophages) trigger the inflammatory response, activated complement proteins can also trigger initial inflammatory reactions. Activated complement proteins at the site of an infection cause mast cells to release histamine and further amplify the inflammatory response by attracting additional phagocytes. As mentioned in Section 26-

So what about that cut on your finger? A scab—
1055
Sometimes an infection is overcome quickly by the inflammatory response and is confined to the site of damage. However, if pathogens are not quickly destroyed, macrophages will be constantly stimulated and will continue to release cytokines. Some cytokines can cause a fever, an elevated body temperature, if their concentration is high enough—
1056
Why do chills and sweating sometimes occur together when you have a fever?
When your body’s thermostat is set higher with a fever, you feel cold and your body responds with rapid periods of muscle contractions and relaxations (shivers and chills). Chills are the body’s way of trying to warm up to the higher temperature setting of the thermostat. When your fever “breaks,” the thermostat is being reset to normal. You sweat because your body is now too hot, and sweating cools your body down. Anti-
Is it always wise to treat a fever with aspirin or other medication?
In the StreetBio at the end of Chapter 20, we described “Darwinian medicine,” a new perspective on when to treat and when not to treat symptoms. From this perspective, many protective responses that have evolved in organisms are recognized as having value in fighting illness. And consequently, treating symptoms such as fever, which is actually part of the immune system response to infection, can hinder our efforts at fighting infection. This idea was supported, for example, by the observation that chicken pox lasted longer, on average, in patients taking aspirin than in patients taking a non-
TAKE-HOME MESSAGE 26.4
Inflammation is a major way in which pathogens are eliminated by the non-
Describe the events (beginning with a wound) that cause the signs of inflammation.
Microorganisms entering a wound are engulfed by macrophages, which release cytokines to attract macrophages, basophils, and mast cells. These basophils and mast cells release histamine, which dilates nearby blood vessels and causes them to leak fluids into tissues. The increased blood supply causes the redness and heat associated with inflammation, while the increased leakiness of the blood vessels causes the swelling. Lastly, the increased pressure stimulates local pain receptors.
1057