23.6 Viruses Are Associated with Some Cancers
As mentioned earlier in this chapter, viruses are responsible for a number of cancers in animals, and there is evidence that some viruses contribute to at least a few cancers in humans (Table 23.6). For example, about 95% of all women with cervical cancer are infected with human papilloma viruses (HPVs). Similarly, infection with the virus that causes hepatitis B increases the risk of liver cancer in some people. The Epstein–Barr virus, which is responsible for mononucleosis, has been linked to several types of cancer that are prevalent in parts of Africa, including Burkitt lymphoma.
| Virus | Cancer |
|---|---|
| Human papilloma viruses (HpVs) | Cervical, penile, and vulvar cancers |
| Hepatitis B virus | Liver cancer |
| Human T-cell leukemia virus 1 (HTLV-1) | Adult T-cell leukemia |
| Human T-cell leukemia virus 2 (HTLV-2) | Hairy-cell leukemia |
| Epstein–Barr virus | Burkitt lymphoma, nasopharyngeal cancer, Hodgkin lymphoma |
| Human herpes virus | Kaposi sarcoma |
| Merkel cell polyomavirus | Merkel cell carcinoma |
| Note: Some of these associations between cancer and viruses exist only in certain populations and geographic areas. | |
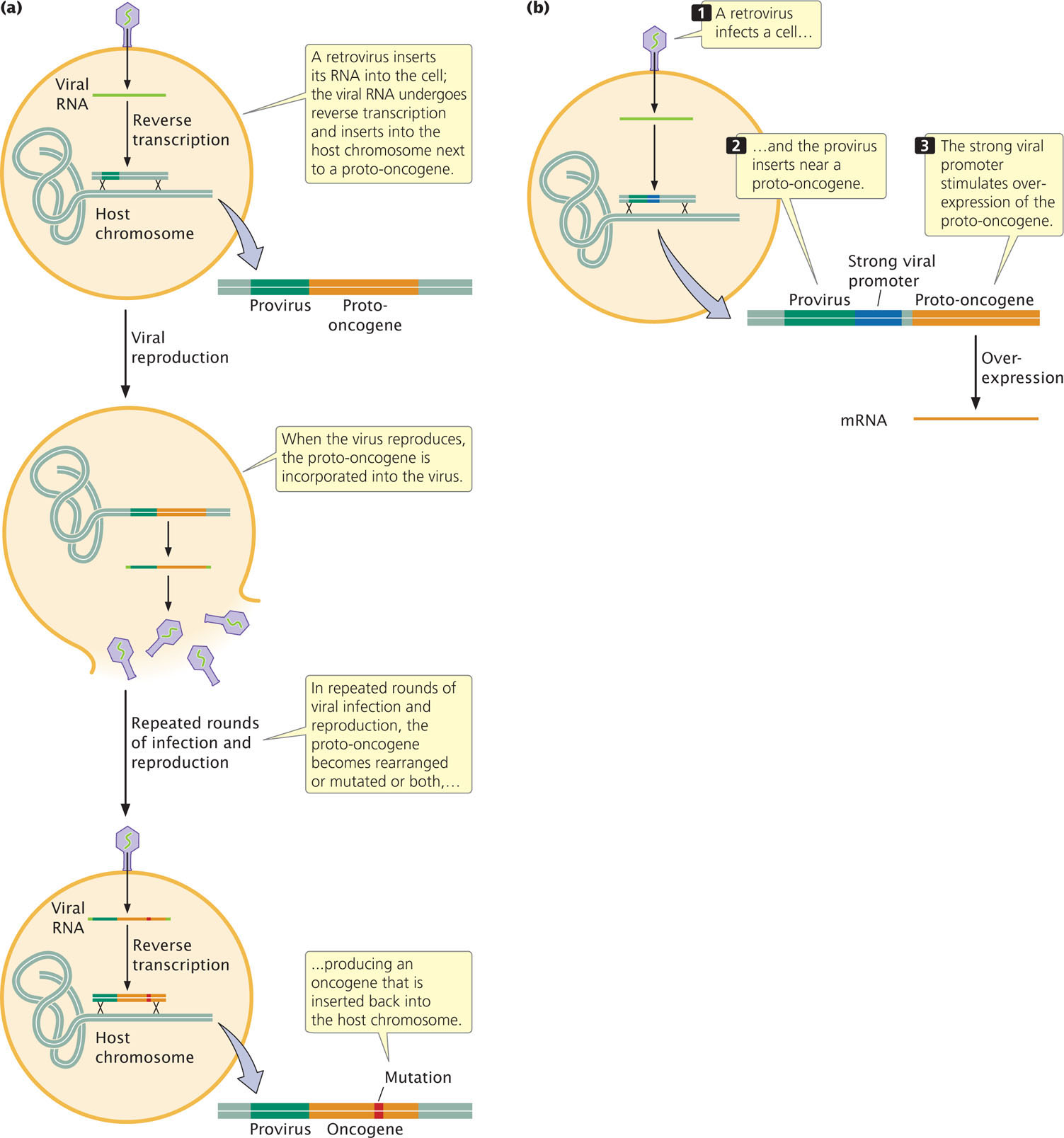
Retroviruses and Cancer
Many of the viruses that cause cancer in animals are retroviruses; earlier, we saw how studies of the Rous sarcoma retrovirus in chickens led to the identification of oncogenes in humans. Retroviruses sometimes cause cancer by mutating and rearranging host genes, converting proto-oncogenes into oncogenes (Figure 23.14a). Another way in which viruses can contribute to cancer is by altering the expression of host genes (Figure 23.14b). Retroviruses often contain strong promoters to ensure that their own genetic material is transcribed by the host cell. If the provirus inserts near a proto-oncogene, viral promoters can stimulate high levels of expression of the proto-oncogene, leading to cell proliferation.
There are only a few retroviruses that cause cancer in humans. HTLV-1, the first human retrovirus discovered, is associated with human adult T-cell leukemia. Other human cancers are associated with DNA viruses, which, like retroviruses, integrate into the host chromosome but, unlike retroviruses, do not utilize reverse transcription. For example, HPV is a DNA virus that is strongly associated with cervical cancer.
Human Papilloma Virus and Cervical Cancer
Human papilloma virus causes warts and other types of benign tumors of epithelial cells. More than 100 different types of HPV are known, about 30 of which are sexually transmitted and cause genital warts. A few of them are associated with cervical cancer. In the United States, 70% of the cases of cervical cancer are caused by HPV-16 and HPV-18. These viruses cause cervical cancer by producing proteins that attach to and inactivate RB and p53, two proteins that play key roles in the regulation of the cell cycle. When these proteins are inactivated, cells are stimulated to progress through the cell cycle and divide without the normal controls that prevent cell proliferation.
About 75% of sexually active women in the United States are infected with HPV, but only a small number of these women will ever develop cervical cancer. The risk of infection by HPV can be reduced by limiting the number of sexual partners and by a vaccine that was approved by the U.S. Food and Drug Administration in 2006. This vaccine is highly effective against four of the most common HPVs associated with cervical cancer. In spite of the large number of women infected with HPVs, the incidence of cervical cancer in the United States has declined 75% in the past 40 years. The primary reason for this decline is widespread use of the Pap test, which detects early stages of cervical cancer, as well as cervical dysplasia, a precancerous growth that can be removed before it develops into cancer.
Although rare in the United States, cervical cancer is the second most common cause of cancer in women worldwide, with high incidences in many developing countries such as those of Sub-Saharan Africa, South Asia, and South and Central America. An estimated 510,000 women throughout the world develop cervical cancer each year, and 288,000 die from the disease. The primary reason for the high incidence and death rate in developing regions is lack of access to the cervical-cancer screening procedures such as the Pap test. The availability of the vaccine against cervical cancer in these developing countries could greatly reduce the incidence of cervical cancer.
CONCEPTS
Viruses contribute to a few cancers in humans by mutating and rearranging host genes that then contribute to cell proliferation, or by altering the expression of host genes.