VITAMIN D
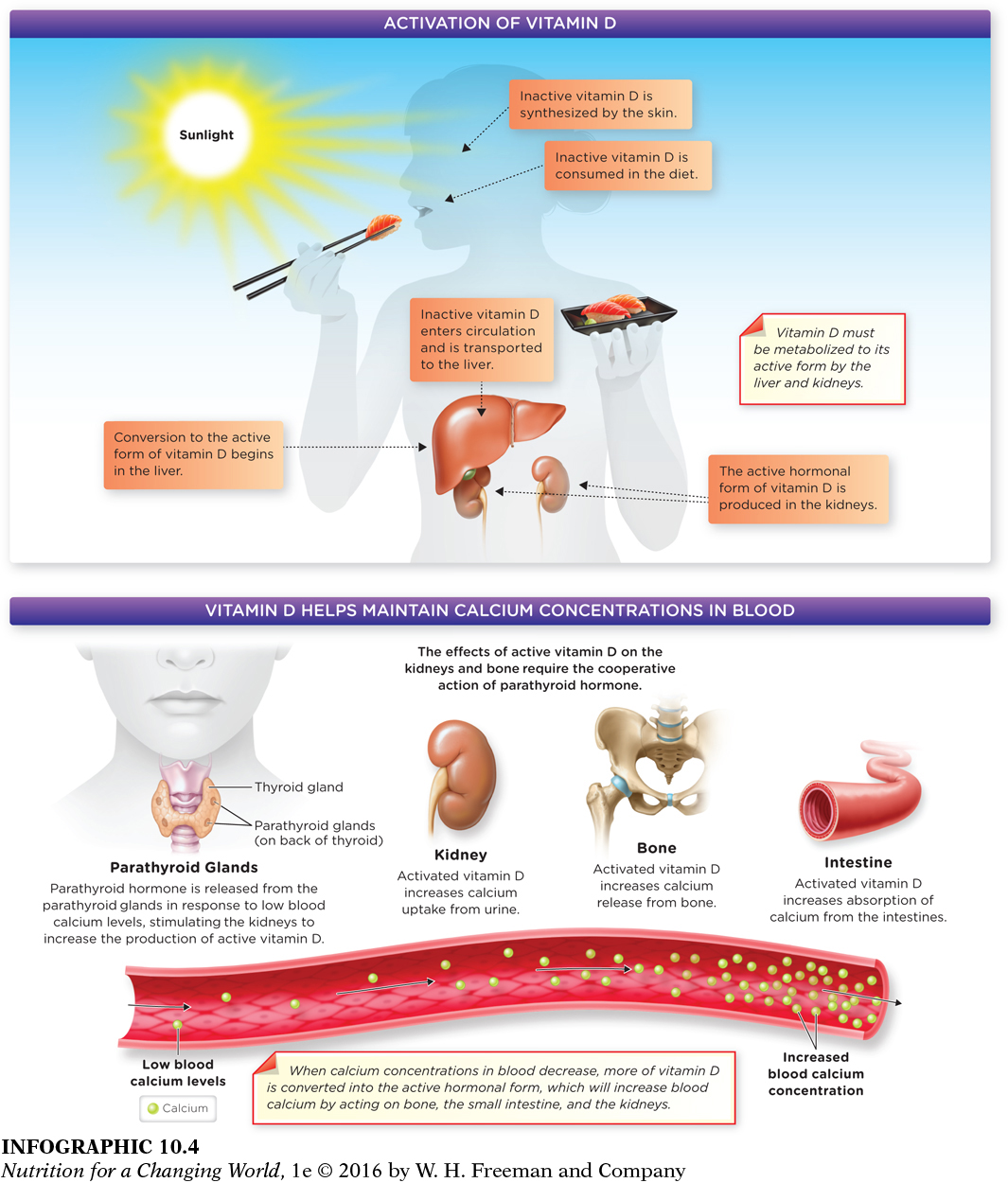
Most people have not considered that a primate could experience a vitamin D deficiency and be stricken with rickets, a condition typically associated with bone malformations in children. However, many people know that vitamin D is often called the “sunshine vitamin,” since it can be produced in the skin from cholesterol with exposure to ultraviolet (UV) light. Most of us meet at least some of our vitamin D needs this way, but with limited sun exposure or impaired synthesis it becomes important to consume sufficient vitamin D through our diet. But, whether through synthesis in the skin or through foods, vitamin D must be activated in the kidneys and liver to fulfill its biological functions in the body.

■ ■ ■
And that, Holick realized, is ultimately what had sickened Kimani—
Sources of vitamin D
Although sunlight can be a significant source of vitamin D, the RDAs—
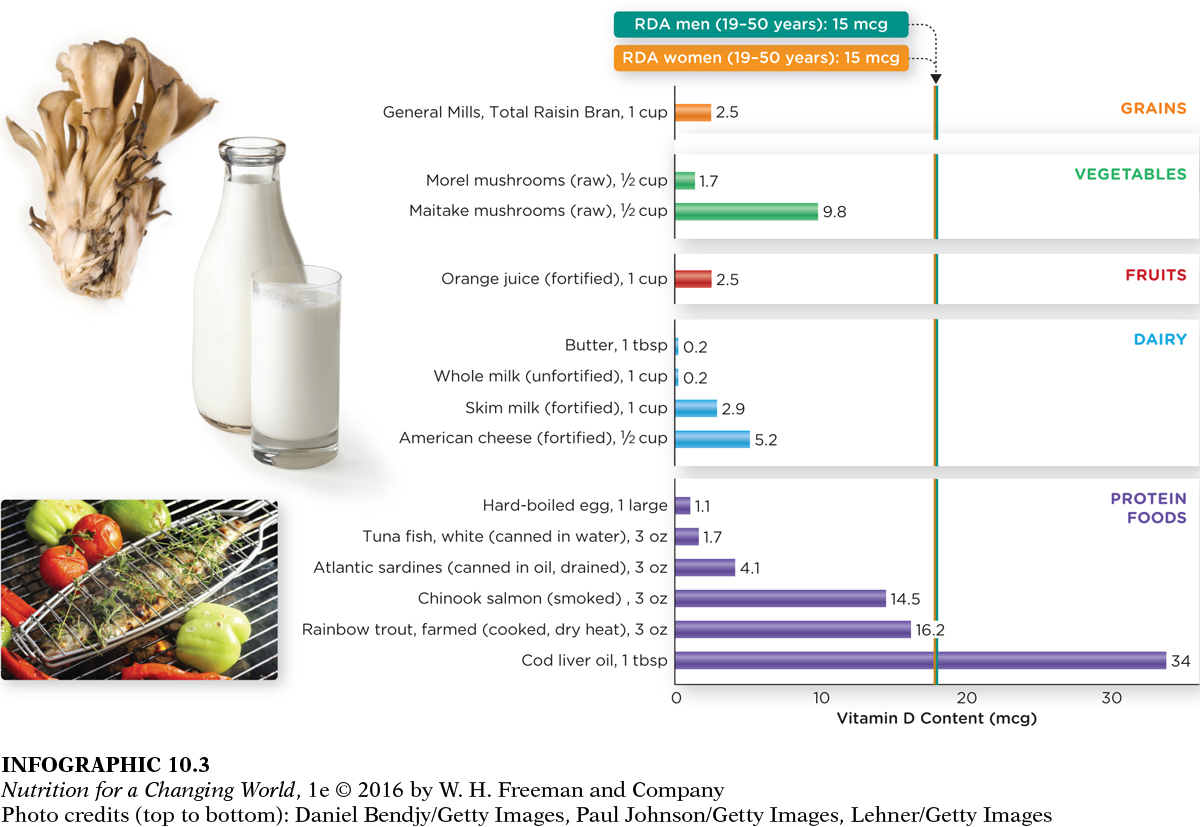
It can be difficult to meet those RDAs from food alone, because vitamin D is present in very few foods naturally. Some of the best sources include fatty fish (such as salmon, tuna, and mackerel) and fish liver oils. Beef liver, cheese, eggs, and some mushrooms (particularly those exposed to UV light) contain small amounts of vitamin D. Alternatively, most Americans get dietary vitamin D from fortified foods—
Question 10.2
 Check the food labels at home to determine which foods have been fortified with vitamin D.
Check the food labels at home to determine which foods have been fortified with vitamin D.
Milk, cheese, yogurt, and orange juice are often fortified with vitamin D.
Functions of vitamin D in the body
Vitamin D has many important known functions in the body. Mainly, as illustrated by the case of Kimani, vitamin D plays a key role in the growth and maintenance of bone by maintaining blood concentrations of minerals involved in bone development, such as calcium and phosphorus. In addition, vitamin D works in combination with other nutrients and hormones in bone growth and maintenance. But beyond bone health, research continues to explore and expand vitamin D’s role in human health.
Vitamin D actually functions as a hormone, since, like hormones, it is made in one part of the body, but carries out its regulatory effects elsewhere. Since it is made from cholesterol, vitamin D is a member of the steroid family of hormones (which includes estrogen, testosterone, and cortisol, among others).
Vitamin D also plays an important role in the regulation of calcium. Most calcium in the body is stored in bones (see Chapter 13), with less than 1% circulating in the blood; however, this circulating calcium is critical for normal muscle and nerve functioning and must be maintained. (INFOGRAPHIC 10.4)
Question 10.3
 Why might the maintenance of appropriate blood calcium concentrations be impaired in someone with advanced liver or kidney disease?
Why might the maintenance of appropriate blood calcium concentrations be impaired in someone with advanced liver or kidney disease?
Advanced liver and kidney disease would impair the conversion of vitamin D to its active form. Active vitamin D is necessary for proper calcium balance in the blood. Additionally, the kidney is responsible for removing excess calcium from the blood.
The regulation of blood calcium requires the interaction of bones, kidneys, and intestines. For example, when the concentration of calcium in blood falls, vitamin D is converted into its fully active hormone form (calcitriol) in the kidneys. This active hormonal form of vitamin D then increases the absorption of calcium in the gastrointestinal tract—
It is estimated that calcitriol is involved in regulating the synthesis of 5% of all proteins in the body. Consequently, it is required for normal cell development and immune function and is critical for other organs and body systems, including the brain, heart, and nervous system, reproductive organs, skin, and muscle. Recent findings suggest that maintaining vitamin D levels in the elderly increases muscle strength and function, and appears to reduce the risk of falls. Evidence is also accumulating that vitamin D is necessary for regulating cardiovascular function. Research now provides evidence that sufficient intake and stores of vitamin D may reduce the risk of a number of important diseases, including cancer, autoimmune diseases, kidney disease, type 2 diabetes, and even cardiovascular disease.
Vitamin D deficiency and toxicity
Vitamin D is listed as a nutrient of concern in the 2015 Dietary Guidelines for Americans. According to data from the 2007-2010 National Health and Nutrition Examination Survey, 94% of all Americans consume less than adequate intakes of vitamin D increasing risk of deficiency particularly in vulnerable populations. People most at risk are those who avoid vitamin D–
OSTEOMALACIA the adult form of rickets, characterized by softening and weakening of bones (brittle bones) accompanied by pain in the pelvis, lower back, and legs
Having extremely low levels of vitamin D can, over time, cause serious bone diseases. Starting in the mid-
But you can also get too much vitamin D—
