SODIUM, POTASSIUM, AND CHLORIDE MAINTAIN FLUID BALANCE IN THE BODY
ELECTROLYTES electrically charged minerals (ions) dissolved in body fluids that balance the fluid outside the cells with the fluid inside the cells
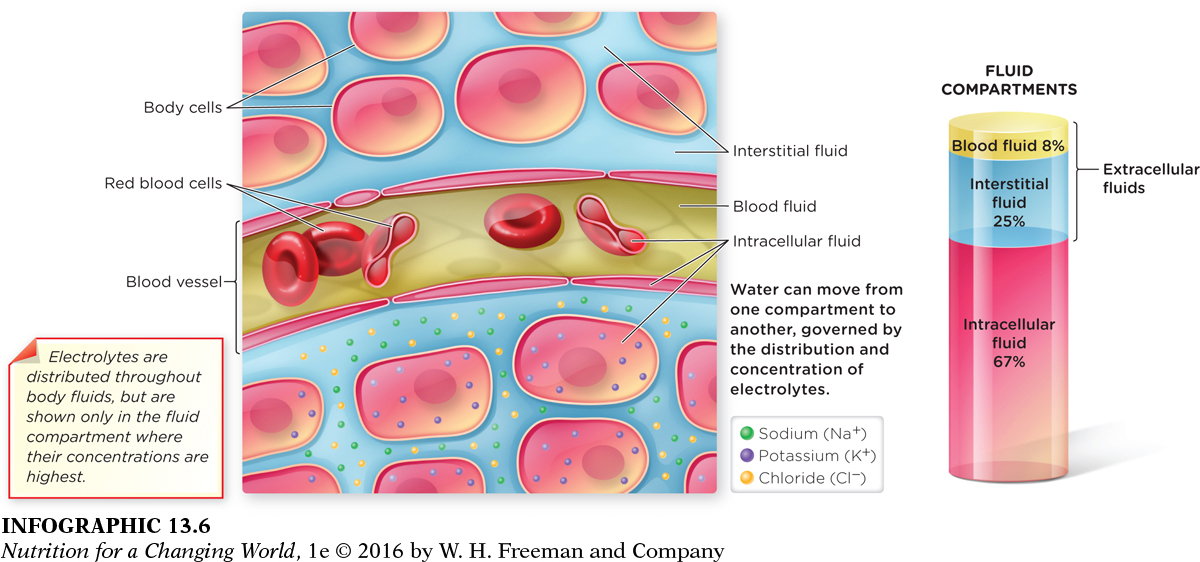
The minerals sodium, potassium, and chloride maintain fluid balance in the body, transmit nerve impulses, and help muscles contract. When dissolved in bodily fluids, such as blood and urine and the fluids inside and outside our cells, these electrically charged minerals are known as electrolytes. Maintaining the right balance of electrolytes is necessary for the transport of nutrients, muscle contractions, and other processes. With the help of the kidneys, electrolytes balance the fluid outside the cells with the fluid inside the cells. Sodium and chloride are primarily found outside cells and potassium is typically found inside cells. (INFOGRAPHIC 13.6)
Question 13.2
 Extracellular fluids include which two fluid compartments?
Extracellular fluids include which two fluid compartments?
Blood fluid and interstitial fluid make up the extracellular fluids.
Sources and functions of sodium
Sodium (Na) is a mineral we are all familiar with, in part because it is widely consumed as table salt, which is otherwise known as sodium chloride (NaCl). Sodium is used extensively in food processing and is often added to foods during cooking and at mealtimes to improve taste. The sodium content of packaged foods is a mandatory component of the Nutrition Facts Panel on food labels.
An essential nutrient, sodium is the primary electrolyte responsible for maintaining fluid balance between cells and throughout the body. It plays a crucial role in regulating blood pressure, and is the major positively charged ion in extracellular fluids such as blood. It is also required to transmit nerve impulses and contract muscles, and is involved in the active transport of a number of nutrients. For instance, sodium is required to move glucose and amino acids into cells. Its role in the active transport of a variety of compounds also means that it is indirectly needed to maintain the body’s acid-
Sodium intake recommendations
HYPERTENSION blood pressure of at least 140/90 mmHg most of the time; a major risk factor for cardiovascular disease and stroke
Overconsumption of sodium is common and increases the risk of hypertension, defined as having a blood pressure of at least 140/90 mmHg most of the time. On average, as Dahl and others have found, blood pressure rises progressively with intakes of sodium above 2,300 milligrams per day. Hypertension is a major risk factor for cardiovascular disease and stroke.
The Institute of Medicine has set the AI level for sodium at 1,500 milligrams per day for men and women aged 19 to 50 years, noting that needs can be increased in endurance athletes who perspire a lot and people who work in hot and humid conditions. The UL for adults 19 years and older is 2,300 milligrams daily. The Dietary Guidelines for Americans recommend limiting sodium intake to 2,300 milligrams per day for adults and children ages 14 and older. The recommended limits align with the UL for sodium for all age groups. No more than 1500 milligrams of sodium per day is advised for adults who would benefit from blood pressure lowering, specifically those with prehypertension or hypertension. Although reducing sodium intake to this level has been demonstrated to reduce the risk of hypertension, there is currently only moderate evidence that it actually reduces the risk of heart disease and stroke. In fact, there is some evidence that low sodium intake (less than 2,300 mg) may actually be associated with adverse health effects in some subgroups.
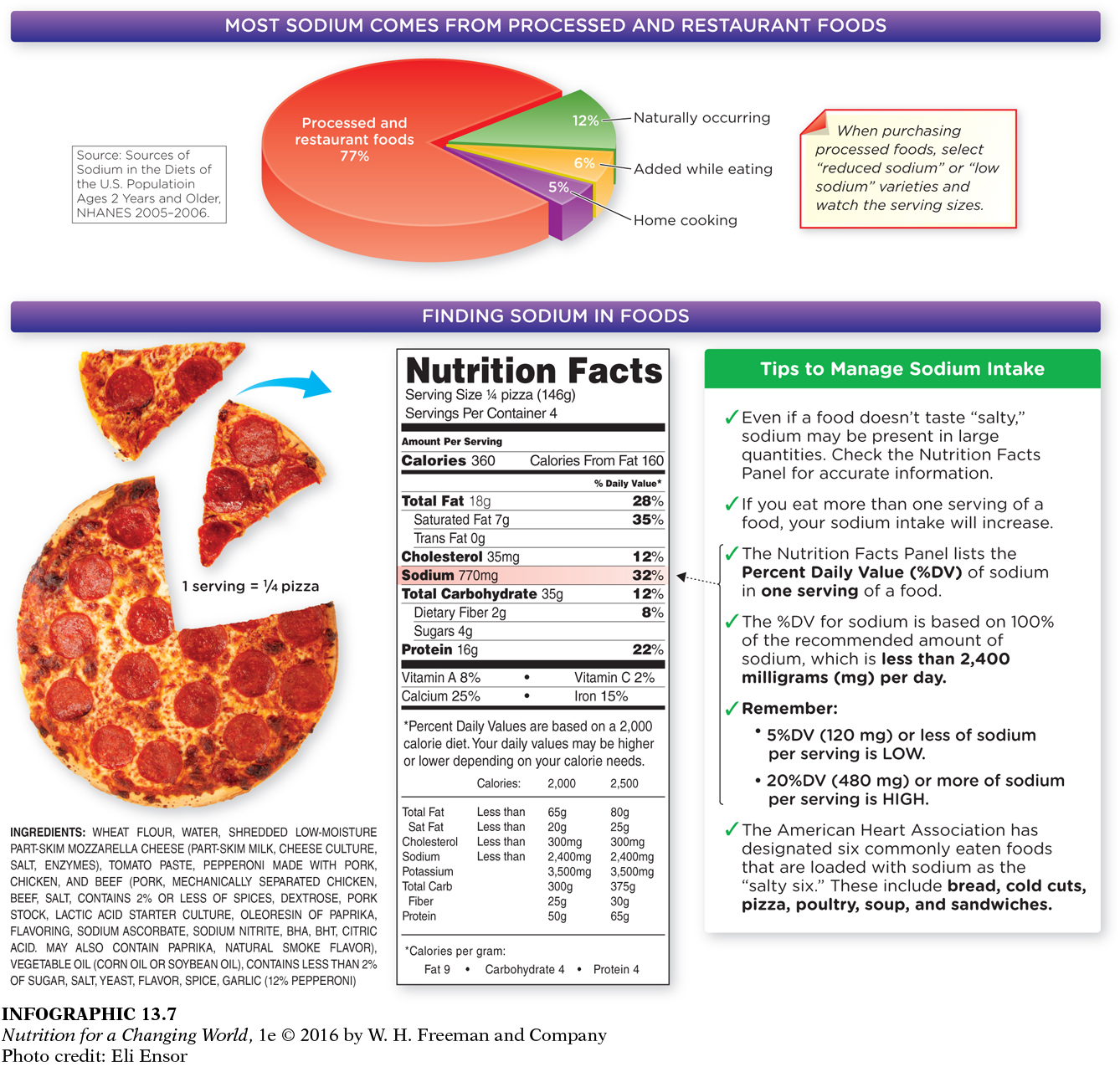
Currently, an estimated 90% of Americans exceed sodium recommendation and average about 3,400 milligrams a day, but that number varies by age and sex. We get most of our sodium from packaged, processed and restaurant foods, with only about 10% coming from salt added at the table and another 10% coming from “fresh” unprocessed foods. (INFOGRAPHIC 13.7)
Question 13.3
 How many times does the word “sodium” or “salt” appear in the ingredients list?
How many times does the word “sodium” or “salt” appear in the ingredients list?
The word “salt” appears on the label three times. “Sodium ascorbate” and “sodium nitrite,” which are additives used in curing meats, also each appear on the label once, for a total of five appearances of salt or sodium on the label.
DASH diet
DASH DIET Dietary Approaches to Stop Hypertension; a food plan that moderates sodium intake while increasing the intake of foods rich in potassium, calcium, and magnesium to assist with blood pressure control
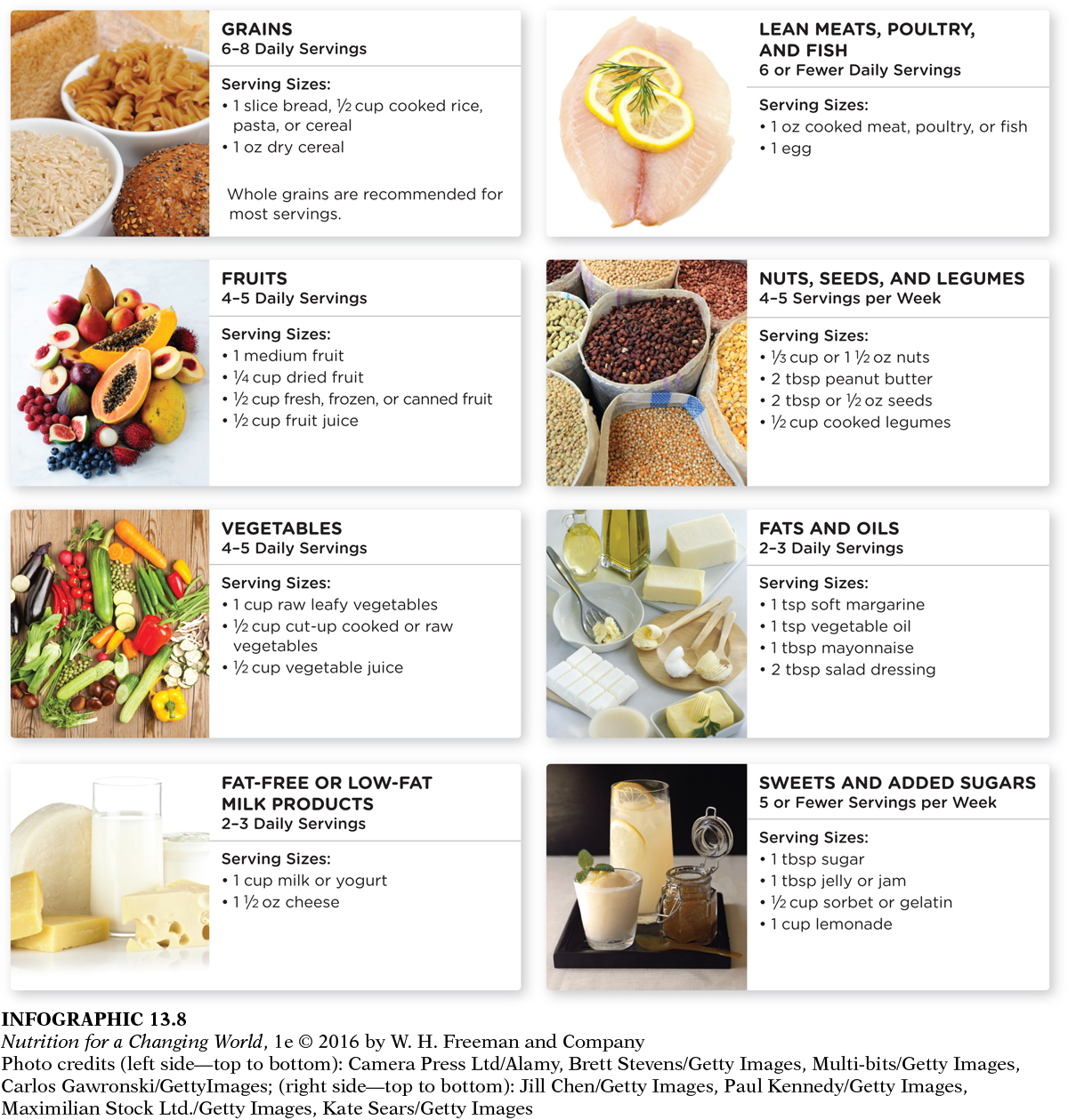
To help Americans reach these lower sodium goals—
Potassium
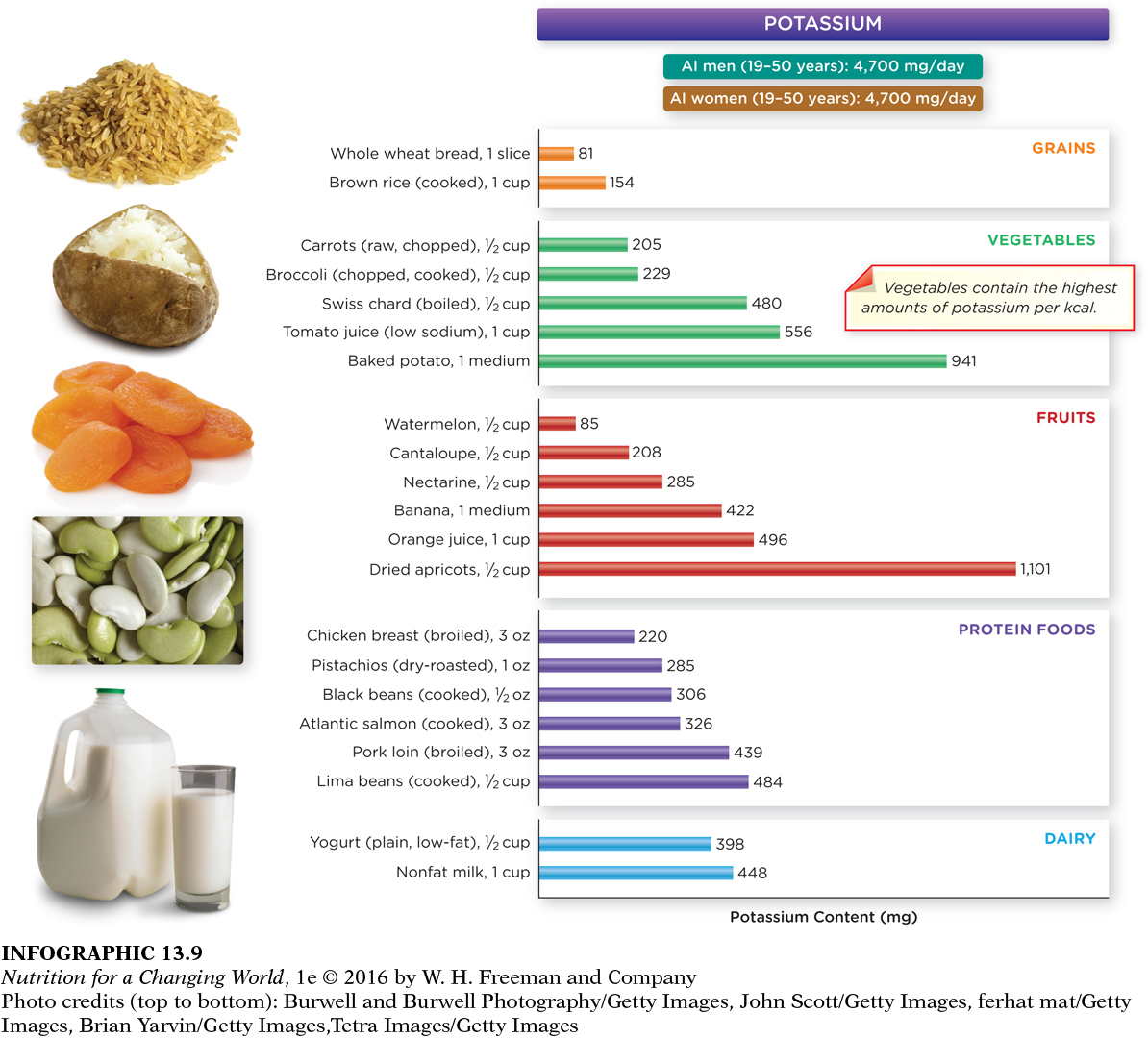
Potassium (K), the primary electrolyte within cells, works together with sodium (and chloride) to maintain fluid balance. As Dahl found back in the 1960s, the level of intake of these minerals affects blood pressure. A diet that emphasizes foods rich in potassium (the DASH diet, for example) may help mitigate some of the effects of excess sodium by increasing sodium excretion in the urine. Potassium may also help relax blood vessel walls, which can also lower blood pressure. Found in a wide range of minimally processed foods, particularly fruits and vegetables, potassium also functions as a co-
Question 13.4
 Vegetables have the highest potassium contents per kcal, but potatoes have a higher content per serving. Considering the concept of nutrient density explain why this is so.
Vegetables have the highest potassium contents per kcal, but potatoes have a higher content per serving. Considering the concept of nutrient density explain why this is so.
The vegetables are more nutrient dense than the potato, so they have much fewer calories per serving. A potato has more potassium but also more macronutrients in a single serving.
HYPOKALEMIA decreased blood levels of potassium
Potassium deficiency, when serious—

Chloride
Chloride (Cl) is the third electrolyte involved in fluid balance. Like sodium, it is primarily found in extracellular fluids such as blood. Since chloride composes half of the mineral composition of table salt (NaCl), our chloride intake correlates directly to our sodium intake. In addition to its role in fluid balance, chloride also forms half of hydrochloric acid (HCl), found in the stomach’s gastric juices. Because sodium is abundant in the American diet, chloride deficiencies are extremely rare. Overconsumption of chloride, like sodium, increases blood pressure.
■ ■ ■

On the morning of April 19, 2004, 27-
Suddenly, at mile 19, Robinson started feeling nauseated and his legs began to cramp. But he kept going, assuming it was just typical end-
It was not dehydration. Robinson was actually dangerously overhydrated. Because he had consumed so much water before, during, and after the race, Robinson’s blood was diluted and contained low levels of sodium. The extra fluid he consumed was also causing his brain to swell. Robinson wound up in a coma and was placed on a life-