FOOD ALLERGIES
FOOD ALLERGY a reproducible, adverse reaction to a food that is caused by activation of an immune response involving the production of antibodies
ALLERGEN an antigen that, when exposed to the body, stimulates an abnormal immune response
FOOD ALLERGEN a substance in food (usually protein) that the body identifies as harmful and that elicits an allergic reaction from the immune system
ANTIBODIES proteins found in blood that are produced in response to foreign substances, such as bacteria, viruses, and allergens, that have entered the body
IMMUNOGLOBULIN E a class of antibody released in response to an allergen
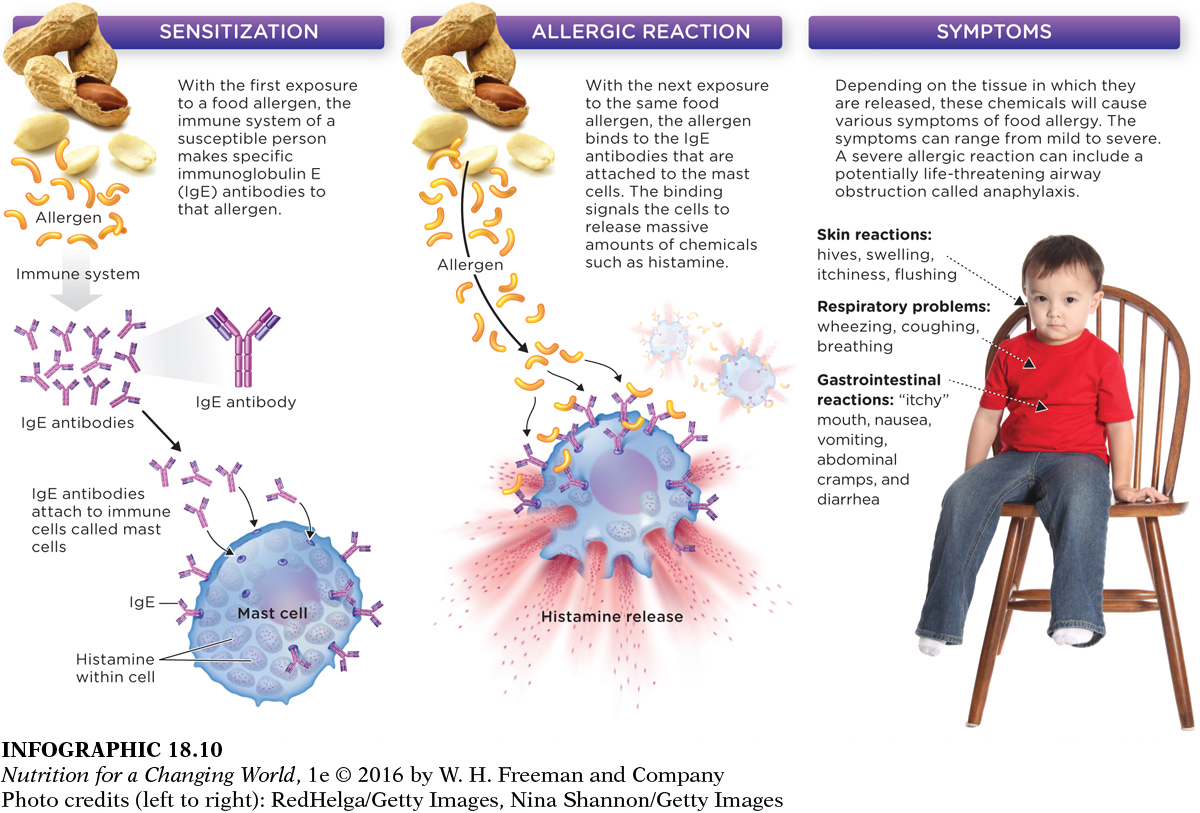
Studies demonstrate that 1 in every 13 U.S. children has a food allergy, a reproducible, adverse reaction to a food that is caused by a type of immune reaction to an allergen in that food. Usually, a food allergen is a small fragment of protein from the food that in susceptible individuals is identified by the body as harmful and that elicits an allergic reaction by the immune system. Interestingly, the first exposure to a food does not cause an allergic response, but it sensitizes susceptible individuals to the food by causing the immune system to produce antibodies (immunoglobulin E [or IgE]) that are specific to the food allergen. When the food is consumed again the food allergen binds to these antibodies, which stimulates immune cells to release histamine and other chemical substances that trigger an allergic reaction. (INFOGRAPHIC 18.10)
Question 18.7
 Why doesn’t first exposure cause any symptoms in those people who develop an allergy?
Why doesn’t first exposure cause any symptoms in those people who develop an allergy?
The first exposure to a food allergen doesn’t cause any symptoms because the immune system does not recognize the allergen. It can’t recognize the allergen until it builds specific antibodies to do so. This immune response is called sensitization. After the antibodies are produced, an allergic reaction is possible with the next exposure to the same food allergen.
ANAPHYLAXIS a condition caused by decreased oxygen supply to the heart and other body tissues, and by vasodilation as a result of a heightened immune response to an allergen
ANAPHYLACTIC SHOCK a massive immune response that occurs in oversensitive individuals and can result in death
EPINEPHRINE (ADRENALINE) a hormone that can be administered as an injection to treat the potentially life-
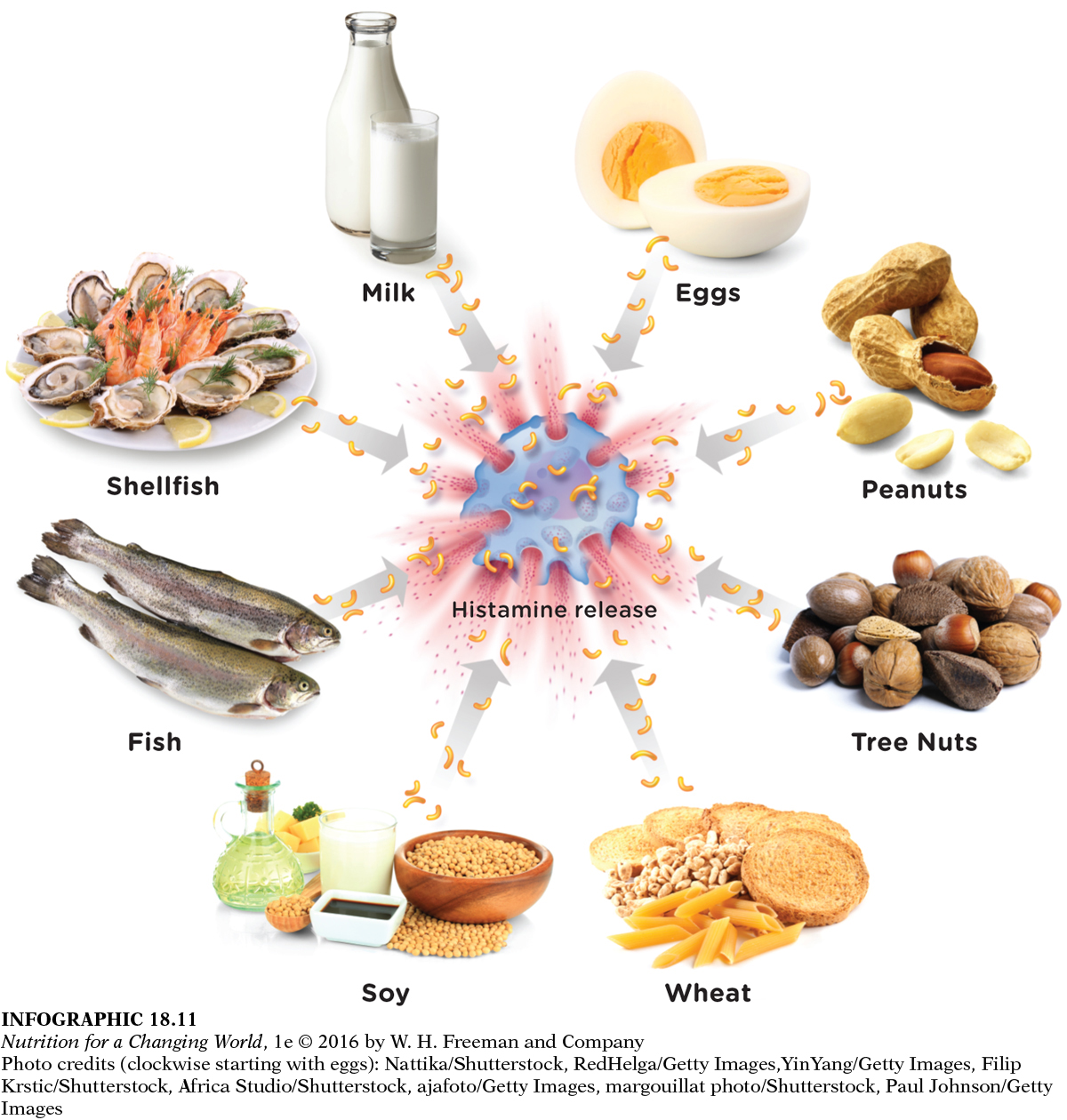
The most common food allergies are to cow’s milk, eggs, peanuts, tree nuts, wheat, soy, fish, and crustacean shellfish. For individuals allergic to one or more of these foods, consuming even minute amounts can be immediately life-
FOOD INTOLERANCE a reproducible adverse reaction to a food that is not a direct result of an antibody dependent immune response; not usually life-
IMMUNE RESPONSE how the body recognizes and protects itself against invading pathogens and foreign substances
Although most adverse reactions or sensitivities to food are attributed to allergies, many food-
How can parents distinguish between food allergies and intolerances? In general, the best way to diagnose mild food allergies is through immunologist-
Some food allergies are diagnosed in children and persist into adulthood. Allergies to peanuts and tree nuts are good examples of this category. There are some allergies, however, that tend to be diagnosed more commonly in adults. For example, estimates of fish allergy appear to be more than twice as high in adults than in children and allergy to crustaceans was five times more common in adults. Furthermore, food allergies can develop at any point in a person’s life.
Why are allergies becoming more common? Some contend that heightened awareness among the public and health care providers translates to increased recognition and diagnosis of allergies. Another theory that was already mentioned was the hygiene hypothesis—
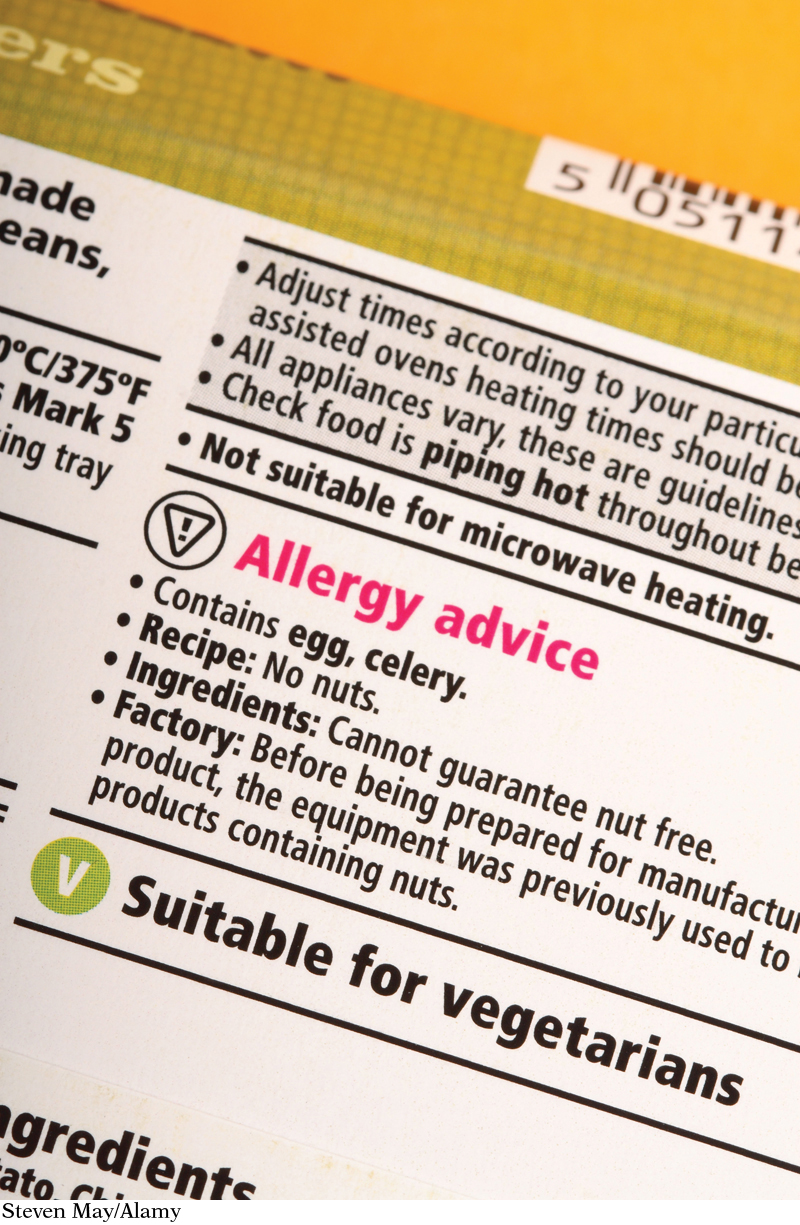
Although there are no food allergy “cures,” it is now getting easier for families to avoid foods that elicit allergic reactions. As a result of the Food Allergen Labeling and Consumer Protection Act of 2004, food manufacturers and packagers have to declare the presence of major food allergens on food packages.
The Academy of Nutrition and Dietetics suggests that parents read food labels carefully; that they educate family members, caregivers, and teachers about allergy severity; and that they teach children about their allergies at a young age. It may also help for parents of children with food allergies to consult with a registered dietitian to develop a healthy eating plan that avoids allergens.
The Academy of Nutrition and Dietetics has published tips for parents who want to minimize the risk of food allergies in their children. They suggest exclusive breastfeeding for at least four months during infancy, which decreases the risk of atopic dermatitis, cow’s milk allergy, and wheezing compared with the use of cow’s milk–
In light of the growing evidence in support for the hygiene hypothesis, can parents do anything else, lifestyle-