WHAT IS DIABETES MELLITUS?
Diabetes mellitus, more commonly known simply as diabetes, is a group of diseases that affect how the body uses blood glucose, and left untreated, can result in life-
The underlying cause of diabetes was unknown until a crucial clue came at the end of the nineteenth century, when German scientists discovered that removing the pancreas from a dog caused it to develop diabetes and die. This suggested that the pancreas isn’t just an organ that supplies digestive enzymes—
■ ■ ■
Most of us know someone with diabetes, and we may know that diabetes affects young people and old people, and has something to do with blood sugar, and that people living with the disease pay close attention to diet and may take medications. But what are the different types of diabetes, and what can you do to prevent diabetes? Understanding what happens when blood glucose is regulated normally, and what happens when it goes awry, is a good place to start.
Blood glucose is tightly regulated
INSULIN a hormone produced in the pancreas that removes glucose from the bloodstream for use by the cells
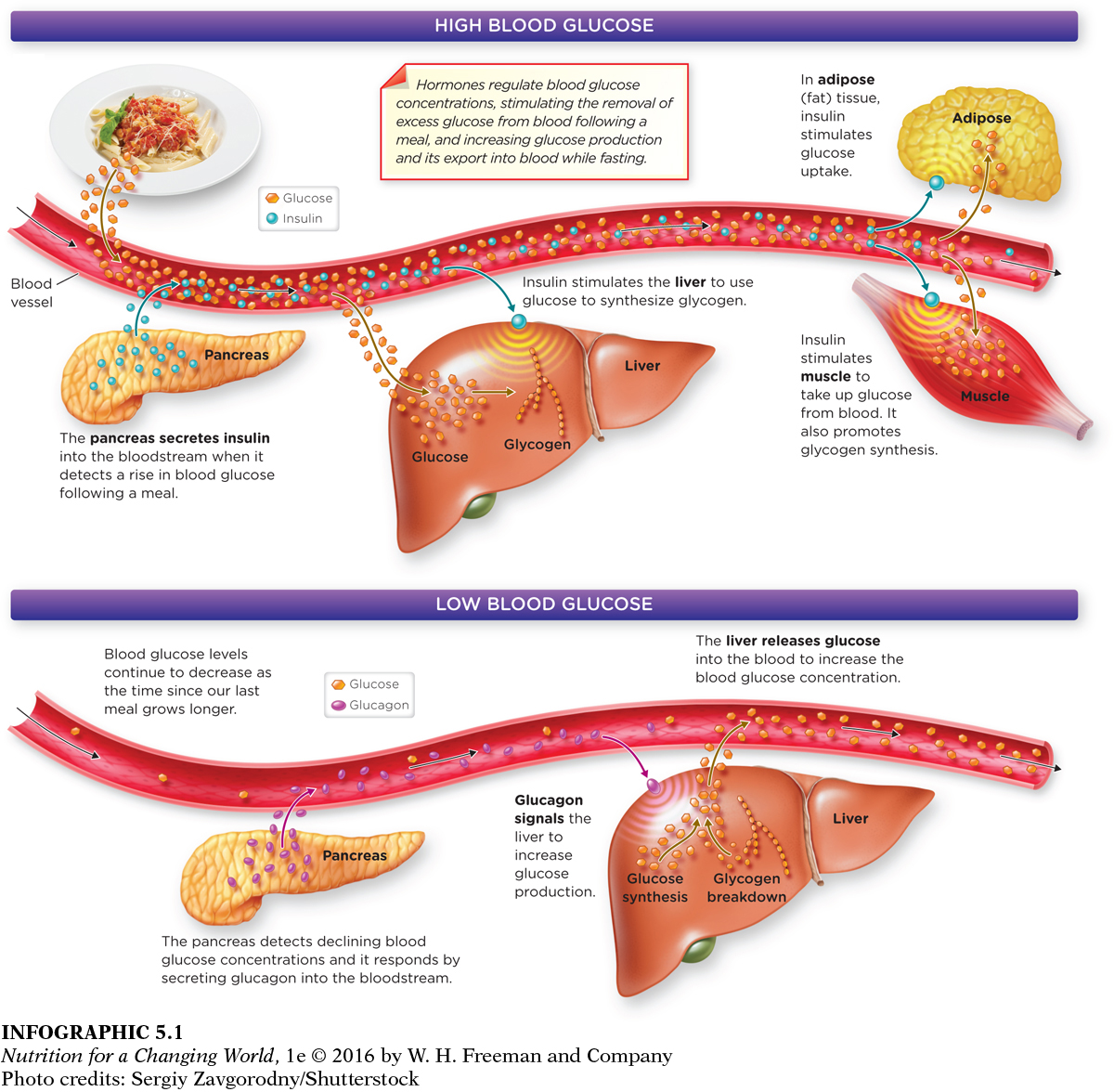
After we eat, levels of glucose in our blood rise. This stimulates the pancreas to secrete the crucial hormone insulin, which directly stimulates the cells in skeletal muscle, cardiac muscle, and adipose tissue (but not other tissues) to take up glucose from the blood. Because more glucose may be available than is needed, the body is able to store the excess energy for later use. Insulin is a potent anabolic hormone in that it stimulates the synthesis of large molecules. Insulin promotes the storage of excess glucose (recall glucose is a single sugar molecule) as glycogen (a molecule made up of many glucose molecules bonded together) in the liver and in skeletal muscle. Because there is a limit to how much glycogen can be stored, insulin also promotes the conversion of glucose to fat in the liver and adipose tissue.
GLUCAGON a hormone produced in the pancreas that increases glucose availability in the blood in response to low blood glucose
Hours after you’ve eaten and levels of glucose in the blood have fallen, the pancreas releases another hormone, glucagon, which signals liver cells to release glucose into the blood to maintain blood glucose levels. The liver produces and exports this glucose by breaking down glycogen, as well as by synthesizing new glucose molecules (primarily from amino acids). (INFOGRAPHIC 5.1)
Question 5.1
 What tissues or organs are stimulated by insulin to take up glucose from blood into their cells?
What tissues or organs are stimulated by insulin to take up glucose from blood into their cells?
The liver, muscle tissue, and adipose (fat) tissue are stimulated by insulin to take up glucose. The liver and muscle tissue both use glucose to synthesize glycogen.
Blood glucose regulation is disrupted in diabetes
TYPE 1 DIABETES MELLITUS an autoimmune disease characterized by elevated blood glucose levels, caused by destruction of the cells in the pancreas that normally produce insulin
We’ve noted the importance of insulin in blood glucose regulation. In diabetes, the hormone insulin is either absent or the cells of the body are resistant to its action. In type 1 diabetes, the pancreatic cells that secrete insulin are destroyed by the body’s immune system, leading to a major deficiency of insulin that typically progresses to its complete absence. Type 1 diabetes is an autoimmune disease, like celiac disease (covered in Chapter 3). In an autoimmune disease, the body’s immune system attacks or destroys its own cells. Type 1 diabetes is not preventable, and between 5% and 10% of individuals with diabetes have type 1.
KETONES (KETONE BODIES) compounds synthesized from fatty acids by the liver when insulin levels are low
KETOACIDOSIS the formation of excess ketone bodies from fatty acids when there is a relative absence of insulin
In type 1 diabetes, the extremely low levels of insulin limit the body’s ability to use glucose. To minimize the breakdown of muscle protein for energy (and prevent muscle wasting), fatty acids are released from adipose tissue. However, the brain cannot use fatty acids effectively for energy, so the liver converts some of these fatty acids into a source of energy the brain can use called ketone bodies. If the diabetes is left untreated, over time these ketones build up in the bloodstream, increasing the acidity of blood and causing a condition called ketoacidosis, which can lead to coma and death.
HYPERGLYCEMIA higher than normal blood glucose levels (fasting plasma glucose ≥ 100 mg/dl).
When the pancreas becomes unable to produce insulin, muscle and adipose tissues cannot appropriately take up glucose, and blood glucose levels skyrocket—


■ ■ ■
Turn-

In a race against time, Banting and Best began their experiments. They knew that the pancreas was producing insulin, so they wanted to find a way to isolate the pancreatic cells that produced insulin. They theorized that if they could purify extracts of these cells to produce insulin itself, they could give them to dying children to make up for what their bodies lacked.
The researchers disrupted the digestive function of the pancreas of one of the dogs, to prevent digestive enzymes from destroying the insulin that they were seeking isolate. They removed the pancreas of one of the dogs, ground it up into a soupy mixture, filtered it, and injected that final product into another dog that had diabetes. Immediately, the dog’s blood glucose levels fell and it appeared to be healthier. With a few daily injections, the dog remained symptom-
If this treatment were to work, Banting and Best reasoned, they needed more pancreas than a handful of dogs could supply. (They had resorted to catching stray dogs on the street.) So they turned to slaughterhouses, procuring fresh pancreas from cows and pigs. That appeared to work just as well, without having to disable the organ’s digestive function first. A biochemist was brought on board to help purify the extracts. Now, with a larger supply of insulin, they could keep several dogs with diabetes alive.
Then, of course, the researchers wanted to find out if this treatment worked in people. For that, they needed a brave volunteer.
Around that time, a 14-
Amazingly, Thompson immediately got stronger. Encouraged, other families brought in their children with diabetes, and those children also reacted well to the medicine. A new era of medicine was born; the next year, Banting and Macleod won the Nobel Prize for Physiology or Medicine.
The researchers soon realized that in order to supply all the insulin that children needed worldwide they had to find a way to mass-