STAPH THE MICROBE
Bacteria are everywhere: in the air, in food, on toothbrushes and computer keyboards—even on and inside the human body. Indeed, the body is host to a wide variety of bacteria, ranging from helpful ones like Lactobacilli and Bifidobacteria that live in the gut and aid digestion, to harmful ones like Salmonella that cause food poisoning. In fact, there are more bacteria living on and in you than there are human cells making up your body. The helpful bacteria on your skin produce acids that make your skin inhospitable to other, less helpful bacteria, generally protecting you from invaders. At any given moment, a fair number of us harbor potentially dangerous bacteria on our skin. Most of the time, this isn’t a problem. But in certain circumstances, these bacteria can overgrow your helpful skin bacteria and cause serious infections.
MRSA infection is caused by the Staphylococcus aureus bacterium—often simply called “staph.” Although several species of staph bacteria can cause human disease, the medical community is especially concerned about staph species, such as S. aureus, that have developed resistance to antibiotic drugs that once effectively killed them. “MRSA” is actually a misnomer because the antibiotic methicillin is no longer used to treat staph infections. Drug-resistant strains of staph are usually resistant to several different types of antibiotics, including penicillins and cephalosporins.
305
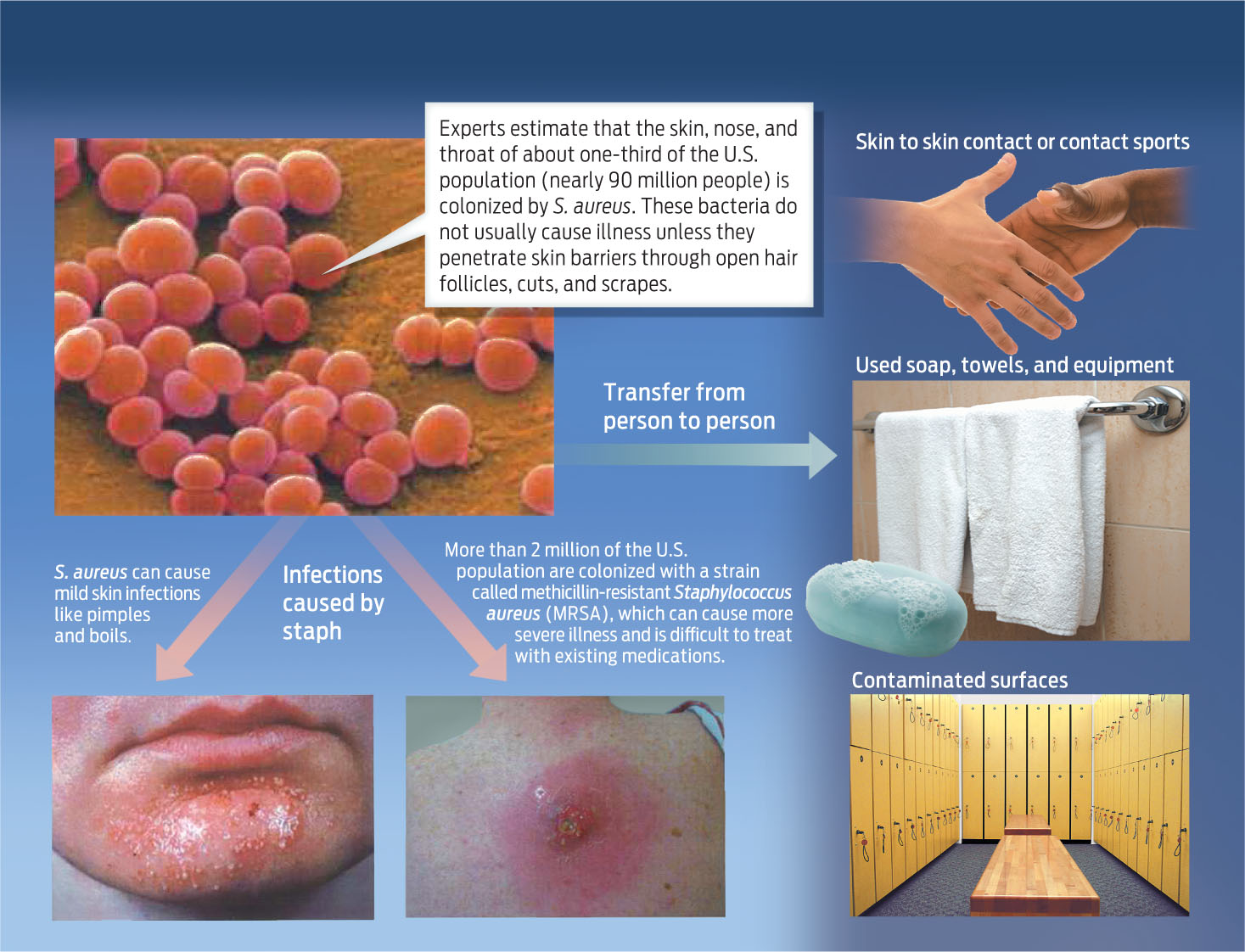
Surprisingly, staph bacteria cause no harm to most of the people who carry them. Between 30% and 40% of the population carries staph on their skin or in their noses, and about 1% of the population carries drug-resistant strains, according to the CDC. If you carry staph of any strain but aren’t sick, you are “colonized” but not infected. Staph spreads from person to person through skin-to-skin contact or through shared, contaminated items such as towels and bars of soap.
Most healthy people can be colonized with any staph strain, including MRSA, and not become ill—for the most part the skin and our immune systems protect us. But infections can occur if staph bacteria come into contact with a wound or otherwise enter the body. For example, athletes who have cuts and scrapes may acquire a staph infection in locker rooms or during contact sports. In otherwise healthy people, staph infection usually causes only minor skin eruptions such as boils or pustules that can resemble spider bites (INFOGRAPHIC 14.1) .
Staphylococcus aureus is a spherical bacterium that can cause pimples, boils, and wound infections in healthy people. S. aureus can be passed from person to person by direct contact with contaminated skin or by transfer of the bacteria via contaminated objects or surfaces.
“Every one of us has probably had a staph infection at some point,” explains Daum. “Staph ranges from the commonest cause of infected fingernails all the way to a severe syndrome with rapid death, and everything in between. Most staph infections don’t even result in a medical encounter.”
306

People with a weakened immune system are at risk for more-severe staph infections, especially if staph finds a way to enter the bloodstream, for example through a surgical wound. The elderly, whose immune systems are weakened, and the young, whose immune systems are still developing, are at especially high risk. And people who are already sick and fighting off other infections can be at high risk, too. When bacteria such as staph do cause illness, they do so by multiplying on or in human tissues. They can also secrete toxic substances that harm human cells or interfere with essential cellular processes. MRSA infections in the lungs and bloodstream are especially dangerous.
Staph bacteria can cause such a range of disease because there are many different strains of staph. Each strain differs from all others in its genetic makeup. MRSA, for example, is composed of a number of unique strains of staph bacteria, and some cause more serious disease than others. In recent years there have been several cases of healthy people becoming severely ill from MRSA infection, most likely because they were infected by an especially deadly strain of drug-resistant staph.
Ricky Lannetti, for example, was a healthy 21-year-old football player at Lycoming College in Williamsport, Pennsylvania. “He was strong as an ox and he ran like a deer,” says his mother, Theresa Drew. In early December 2003, Ricky came down with a bout of flu. He wasn’t recovering, and on the morning of December 6, Drew drove her son to Williamsport Hospital. By the time he was admitted, his blood pressure was dangerously low and his body temperature was erratic. As each hour passed, his condition worsened. His lungs began to fail. Doctors tried five different antibiotics, all in vain. When his heart began to weaken, his doctors prepared him to be flown to the cardiac center at a bigger hospital in Philadelphia. But it was too late. Ricky died that night.
It was only after an autopsy was performed that doctors discovered what had killed him: MRSA had infected Ricky’s bloodstream and ravaged his insides. Although doctors couldn’t be sure how Ricky contracted MRSA, they suspect that it entered his body through a pimple on his buttocks. From there, it spread to his internal organs.
“Doctors tried every antibiotic imaginable, including vancomycin,” says his father, Rick Lannetti. But the treatment was too late. Ricky’s immune system was already weak because of the flu. When he contracted MRSA, his body was unable to fight back as well as it otherwise would have. “In the end,” his father says, “MRSA had broken every one of his organs beyond repair.”
307