STOPPING SUPERBUGS
Staph bacteria aren’t the only ones that have grown resistant to antibiotics. It is getting harder to treat patients with severe Salmonella food poisoning caused by drug-resistant strains. Neisseria gonorrhoeae, the bacterium that causes gonorrhea, has become resistant to another important group of antibiotics, the fluoroquinolones. And there are now forms of pneumonia caused by strains of Klebsiella that are resistant to every available antibiotic.
Because the very use of antibiotics can drive bacterial populations to evolve resistance, antibiotic resistance is inevitable. But humans have hastened the emergence of drug-resistant strains of bacteria by the haphazard use and overuse of antibiotics. From the moment antibiotics were first introduced, physicians began prescribing them for colds, coughs, and earaches, most of which are caused by viruses that aren’t killed by antibiotics anyway. Antibiotics are frequently overused or misused for many other ailments as well, contributing to an environment that promotes resistance.
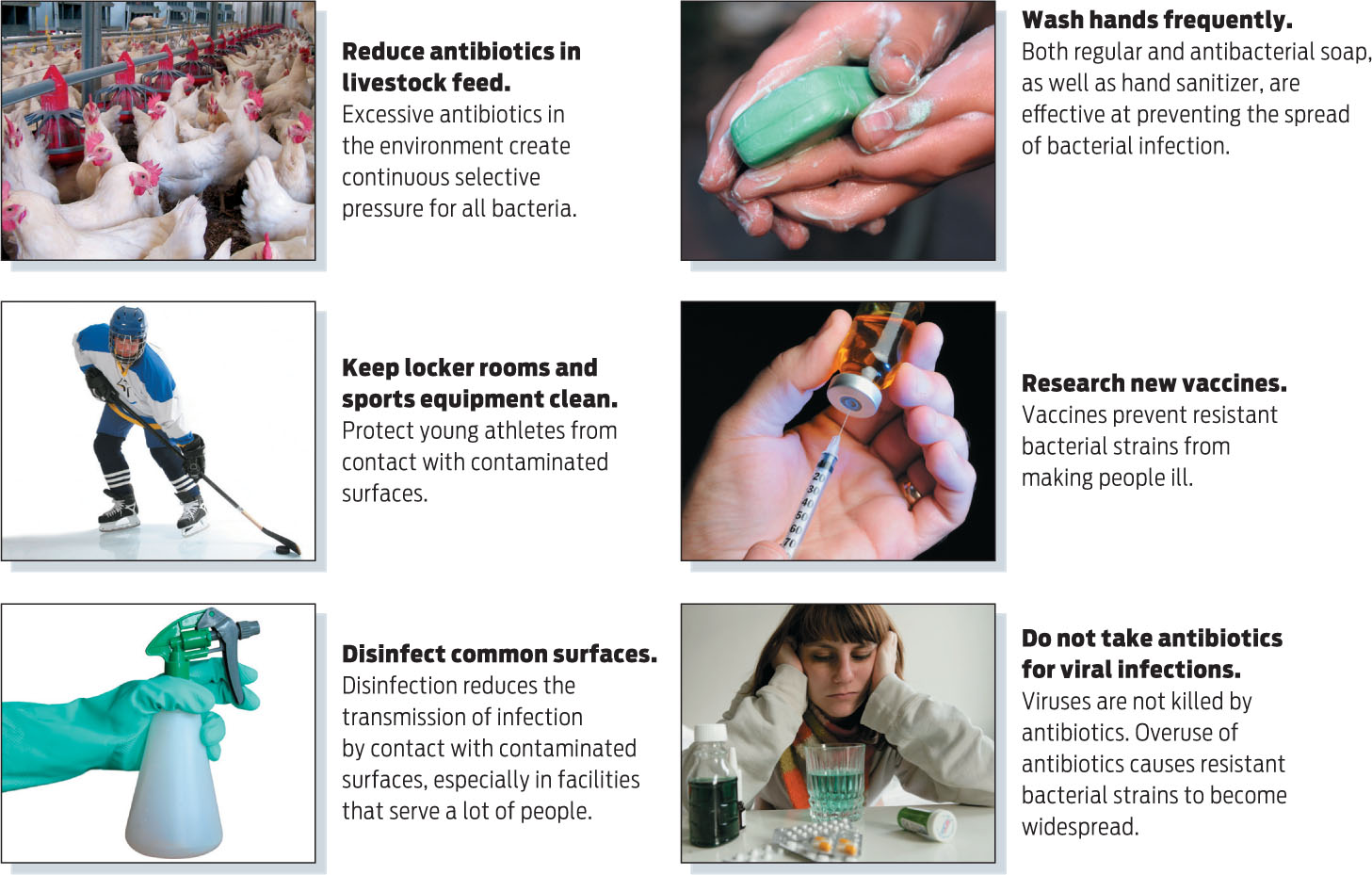
Doctors aren’t the only culprits. Farmers give antibiotics in low doses to poultry, swine, and cattle to promote growth. This practice can cause food-borne pathogens such as Salmonella or Campylobacter to develop antibiotic resistance. Undigested antibiotics in animal manure can contaminate the environment through groundwater or when manure is used as fertilizer. In this environment drug-resistant bacteria are more fit and will therefore be selected for and become more prevalent over time.
“We really have to be careful about how we use antibiotics because antibiotic use is the biggest driver of antibiotic resistance,” says Lynfield, of the Minnesota Health Department.
Some public health officials are concerned that increased use of so-called antibacterial soaps that contain the bacteria-killing chemical triclosan might be contributing to the emergence of antibiotic-resistant superbugs. Although triclosan is not used as an antibiotic, some researchers worry that bacteria that become resistant to triclosan might also be able to resist antibiotics by a phenomenon known as cross-resistance. So far, there is no conclusive evidence that triclosan leads to antibiotic resistance in populations. Nevertheless, most experts agree that using antibacterial soaps is overkill: multiple studies have failed to find any benefit to washing with antibacterial soaps over and above washing with plain old soap.
315
Alcohol-based sanitizers are not thought to contribute to cross-resistance because the alcohol quickly evaporates, leaving no bacteria-killing residue. In contrast, soaps that contain triclosan can linger on surfaces like sinks, providing a possible opportunity for bacteria to adapt to the presence of the chemical.
Clearly, developing stronger antibiotics isn’t the only or the best solution to the problem of resistance because bacteria will ultimately adapt to those, too. Perhaps the best way to control resistance, say experts, is to change practices that enable resistant strains to thrive. Careful hygiene and prevention of infection through vaccination are important tools. It is also important that when an antibiotic is prescribed it is taken precisely as prescribed, for the full course of treatment, no matter how much better the patient may be feeling. If bacteria are exposed to antibiotics at low levels or for short durations, the entire population may not be eradicated. The remaining bacteria may be resistant to the antibiotic and proliferate. And anyone taking antibiotics exposes all the bacteria in his or her body to the antibiotics, possibly enabling other drug resistant bacteria to emerge. These drug-resistant bacteria might then be transmitted to other people.
At the community level, the more antibiotics that are used, the more resistance that will emerge. So doctors are heavily discouraged from prescribing antibiotics unnecessarily. And efforts are being made to crack down on the practice of feeding livestock low levels of antibiotics (INFOGRAPHIC 14.8) .
316
Of course, these measures won’t fight resistant strains that are already circulating. But there are ways to reduce and perhaps prevent infections in this case, too. Because MRSA is more prevalent in certain environments, they present opportunities for health care workers to intervene. Prisons and jails, for example, are hot spots for infection because inmates often have limited access to soap and other forms of hygiene, are housed close together, and may not receive prompt medical care. When infected prisoners are released, they can then spread their germs to relatives and friends. “People go in, they pick up MRSA, they take it home, and then I see the kids come in sick,” says Daum. By preventing transmission in correctional settings, health care workers may be able to prevent infections in the larger community.
A vaccine would be another way to prevent staph infections. A vaccine for children against Streptococcus pneumoniae introduced in 2000 caused the rate of infection—and especially the rate of drug-resistant infections—to drop dramatically. And not only did the rate of infection drop in vaccinated children, but other age groups benefited as well because the bacteria were not being transmitted as frequently. As another example of the impact that vaccines have on infections, Daum points to the bacterium Haemophilus influenzae, which frequently caused pneumonia, meningitis, and other serious diseases in children. Today, children are vaccinated against it. “When I was an intern we used to see 60 to 80 Haemophilus infections a month,” he says. “Today we see none, it’s gone. And MRSA needs to be gone, too.” 