Codominance
 Who can be a universal blood donor?
Who can be a universal blood donor?
ANSWER: When someone needs a blood transfusion, the donated blood cannot come from just anyone. The transfused blood must be compatible in ways that are determined by genetics. The two most important genetic attributes are ABO blood type and Rhesus (Rh) factor, both of which must be compatible between donor and recipient. Mixing incompatible blood causes blood cells to clump, a life-threatening condition.
CODOMINANCE A form of inheritance in which both alleles contribute equally to the phenotype.
Your blood type indicates the presence or absence of specific protein markers, or “flags,” on your red blood cells. For example, if you have type A blood, your cells display A markers. There are three basic blood type alleles: A, B, and O. Since we inherit one allele from each parent, the possible combinations of the three alleles are OO, AO, BO, AB, AA, and BB.
Blood type is an example of codominance—both maternal and paternal alleles contribute equally and separately to the phenotype. Unlike incomplete dominance, in which heterozygotes have an intermediate phenotype, codominant alleles share the limelight: heterozygotes express both traits.
Blood type alleles A and B are codominant, while O is recessive to both A and B. Consequently, if you have blood type A, your genotype will be either AA homozygous or AO heterozygous. The same goes for blood type B: you will have a genotype of either BB or BO. People with type AB blood have an AB genotype and express both A and B markers on their cells (INFOGRAPHIC 12.7).
In codominant inheritance, heterozygotes display the effects of both alleles in their phenotype. Human blood type is an example. Alleles for blood type code for different surface markers on red blood cells. A person with type AB blood, for example, displays both A and B markers, while type O blood displays no surface markers. A person’s blood type must be considered when he or she gives or receives blood.
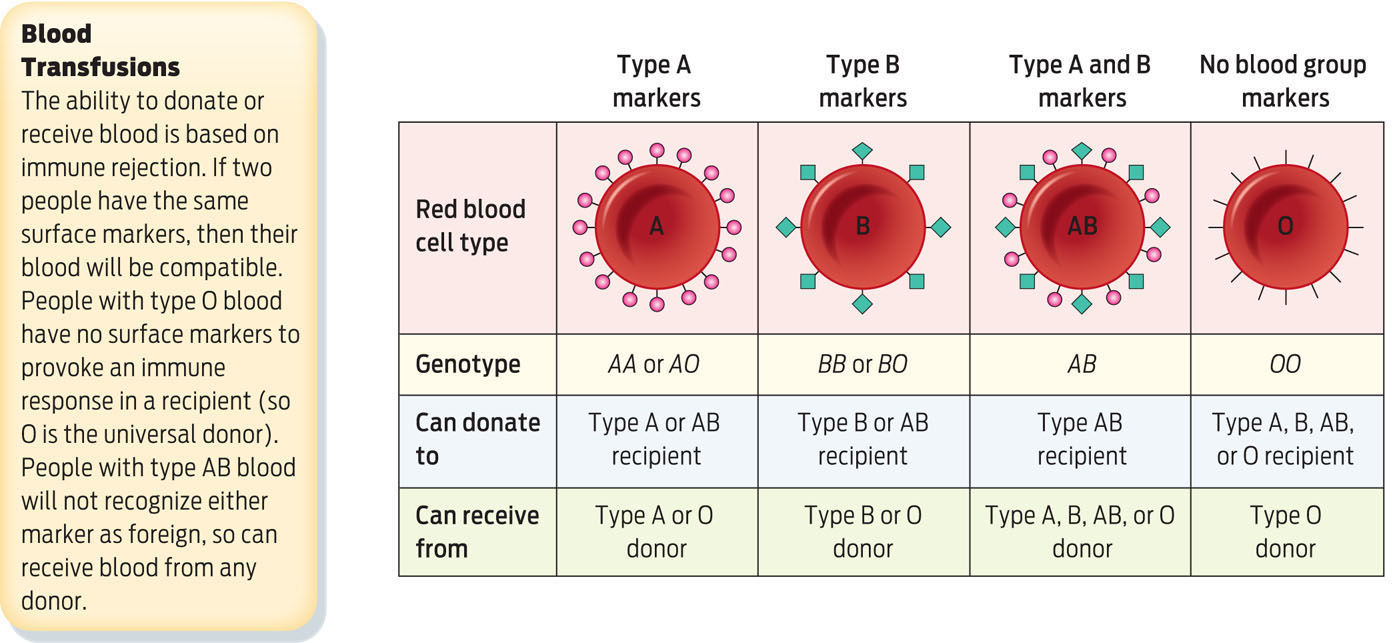
Blood Transfusions
The ability to donate or receive blood is based on immune rejection. If two people have the same surface markers, then their blood will be compatible. People with type O blood have no surface markers to provoke an immune response in a recipient (so O is the universal donor). People with type AB blood will not recognize either marker as foreign, so can receive blood from any donor.

Your Rh status, (+) or (−), indicates the presence or absence of Rh proteins on the surface of your red blood cells. Rh factor genes are inherited in a dominant and recessive fashion: the positive Rh factor allele (Rh+) is dominant over the negative Rh factor allele (Rh-). So if a person carries one positive and one negative allele, the positive allele will dominate and that person will have an Rh-positive phenotype.
Type O Rh-negative donors are known as universal donors because their blood can be transfused to patients of any other blood type; red blood cells from these donors lack surface markers and so will not trigger an immune response in a recipient. Because any patient can receive O Rh-negative blood, “O negative” donors are always in demand. Blood banks can fall short of O negative blood during such disasters as earthquakes or hurricanes in which many people are hurt and require blood (INFOGRAPHIC 12.8).
If donor and recipient are not compatible in ABO blood type and Rh factor, a recipient can have a life-threatening immune reaction to donated blood. A person with type A blood, for example, cannot donate blood to a person with type B blood.
