NO FUEL LEFT TO BURN
GLYCOGEN An energy-storing carbohydrate found in liver and muscle.
PANCREAS An organ that secretes the hormones insulin and glucagon, as well as digestive enzymes.
Although the body is able to cope with cold temperatures for some time through vasoconstriction and shivering, it cannot do so indefinitely. Thermoregulation is work, and work takes energy—roughly 150–300 Calories per hour for a 150-pound man. Eventually, if the body is not consuming food, it will run out of fuel.
INSULIN A hormone secreted by the pancreas that causes a decrease in blood sugar.
The main fuel the body uses in times of intense activity is the sugar glucose, a breakdown product of carbohydrate digestion. When we eat carbohydrates, sugars are released and absorbed into the circulation, and “blood sugar” (the concentration of glucose in the blood) increases (see Chapter 4). Some of this sugar may be used immediately as fuel for aerobic respiration in cells of the body (see Chapter 6). Whatever is not needed right away will be converted into glycogen, which is stored in muscles and the liver.
GLUCAGON A hormone produced by the pancreas that causes an increase in blood sugar.
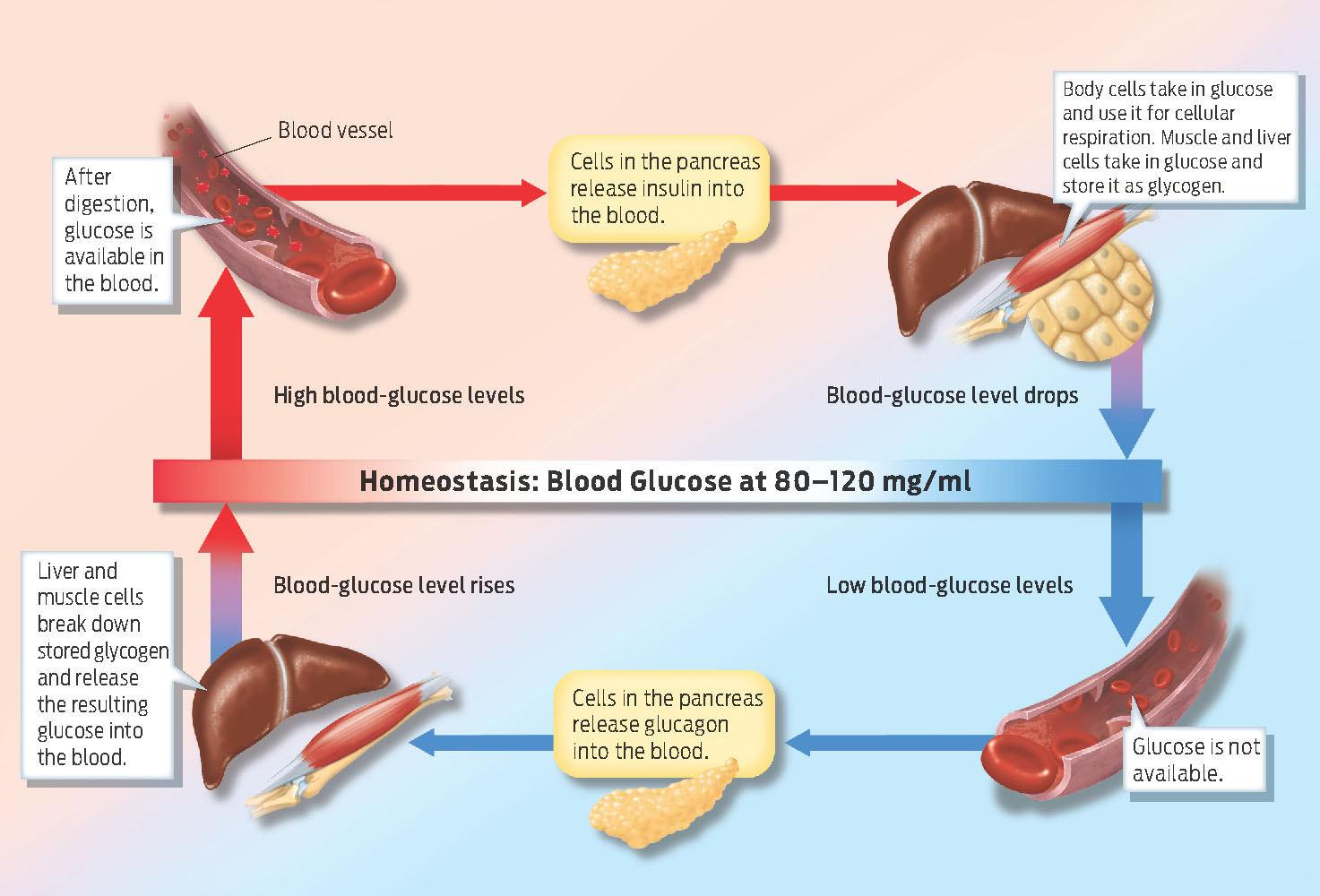
Blood sugar is monitored and controlled by the pancreas, a small organ near the stomach that functions in both the endocrine and digestive systems (see Milestone 7). In response to high blood sugar, endocrine tissue in the pancreas produces the hormone insulin, which acts on liver and muscle cells, signaling them to remove sugar from the blood. The glucose taken up from the blood will either be used immediately for cellular respiration or stored as glycogen. Like many hormones, insulin acts by binding to receptors on target cells, much as a key fits into a lock.
559
When blood sugar is low, the body first prompts us to eat by sending a signal to the hypothalamus, which cues hunger. If eating isn’t an option, the body begins to break down its stored glycogen. The key signal here is the hormone glucagon, which is released by the pancreas in response to low blood sugar and triggers liver and muscle cells to break down their stored glycogen into glucose. The liver can release this glucose into the blood, providing fuel for other tissues, particularly the brain. The breakdown of glycogen in skeletal muscle helps provide energy for the muscle itself.
The amount of glucose in the blood is therefore tightly regulated: when blood-sugar levels are high, excess glucose is stored in cells as glycogen (in response to insulin). The stored glycogen represents a source of glucose to be released into the blood during periods of starvation (in response to glucagon). The opposing effects of insulin (reducing blood glucose) and glucagon (increasing blood glucose) illustrate another example of homeostasis, in this case maintaining a relatively stable blood-sugar level (INFOGRAPHIC 25.5).
The pancreas responds to variation in blood-glucose levels by secreting insulin, inducing cells to take in excess glucose, or by secreting glucagon, inducing liver and muscle cells to release stored glucose.
The trapped climbers hadn’t eaten in hours, which meant they were operating on stored energy. Glycogen is the main stored fuel that is tapped during vigorous exercise. But the human body can store only so much glycogen. Eventually, after hiking and shivering for many hours, you will exhaust this fuel supply. Without this fuel, your body will struggle to remain active and shiver. And if you can’t remain active and shiver, then you can’t generate heat and your body temperature will fall. That’s when hypothermia can set in.
560
The average adult has enough stored glycogen to power about 12 to 14 hours of routine activity. When a person is exercising strenuously—say, running or hiking—glycogen stores can be depleted in as little as 2 hours. Marathon runners often refer to this point, which occurs at about mile 20, as “hitting the wall.” Then, in order to continue exercising, you must eat something—preferably something with carbohydrates.
“A lot of mountaineering communities think you need fat,” says Kenefick. “And that’s true—fat has more Calories per gram—9 kcals per gram compared to 4 kcals per gram of protein or carbohydrate. But when you’re doing things like shivering, those types of contractions, especially, use a lot of glucose.” Fats—though a good source of stored energy—are not as readily available for immediate use. And glucose is the primary fuel for the brain.
OSMOLARITY The concentration of dissolved solutes in blood and other bodily fluids.
Fitness also likely played a role in how the Everest climbers fared. Being fit means having more muscle mass relative to fat for a given body weight. Having more muscle mass means you have more glycogen and can exercise longer and generate more heat through cellular respiration. Someone who is less fit, or who simply has less muscle mass, will tire sooner, need to sit down and rest, and continue to lose heat to the environment. This is likely what happened to the climbers who were too weak to hike back to camp: they ran out of their glycogen stores sooner than other climbers.
OSMOREGULATION The maintenance of relatively stable volume, pressure, and solute concentration of bodily fluids, especially blood.
Another exacerbating factor would have been dehydration—a little-known cold-weather risk. In cold conditions, our bodies must work harder under the extra weight of heavy clothing, and sweat evaporates quickly in cold, dry air. We also lose a significant amount of water as water vapor when we exhale. The human body is about 65% water by weight, and when the total amount of water drops by only a few percent, we become dehydrated—which can cause dangerous side effects like delirium, confusion, and convulsions. Kenefick points out that people do not feel as thirsty when it’s cold, and thus become even more dehydrated. “We’re really tropical animals,” says Kenefick. “We came from the Sub-Sahara. We do much better in the heat.”
KIDNEY An organ involved in osmoregulation, filtration of blood to remove wastes, and production of several important hormones.
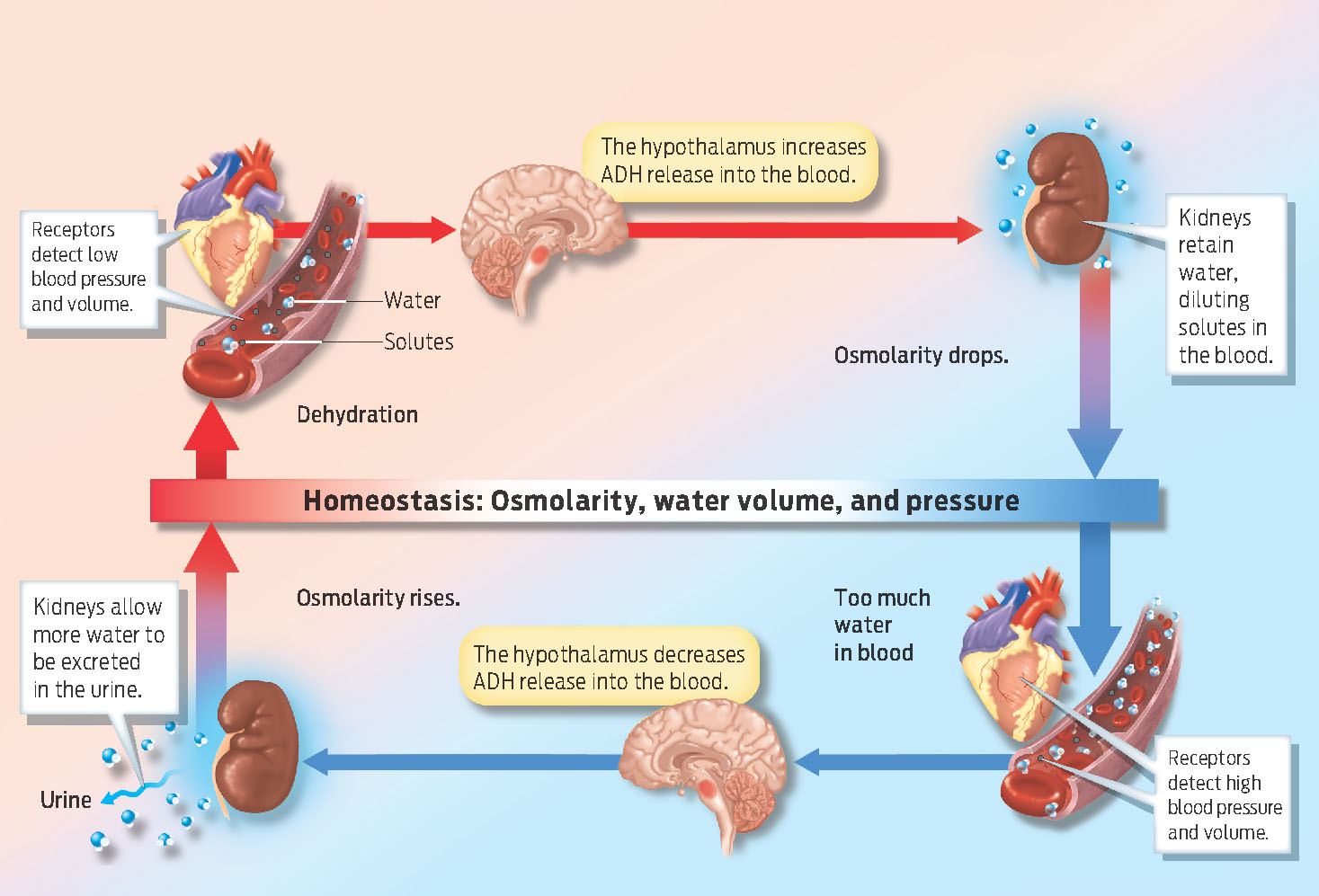
Our body’s sense of thirst relies on osmolarity, the concentration of dissolved solutes in the blood. Among the solutes dissolved in blood are electrolytes—ions such as sodium and potassium that are critical for nerve signaling and muscle contraction. Osmolarity is monitored by the hypothalamus as part of osmoregulation. When you are dehydrated—when you have less fluid in your blood—the concentration of dissolved solutes is higher. If the hypothalamus registers that the concentration of solutes in the blood is high, it will trigger a sense of thirst, encouraging you to drink. At the same time, it triggers the release of antidiuretic hormone (ADH) from the pituitary, which travels through the bloodstream and acts on the kidneys. ADH signals the kidneys to excrete less water in the urine. By reducing the amount of water lost in urine, ADH causes more water to be reabsorbed by the kidneys back into the bloodstream. Water in the bloodstream dilutes dissolved solutes and lowers the osmolarity. That’s why people who are dehydrated have darker urine—it contains less water and so is more highly concentrated.
Osmoregulation also depends on sensors that detect changes in blood volume and pressure. Sensors in the heart, for example, sense how full the heart’s chambers are; sensors in blood vessels sense how stretched the vessels are. When low blood volume and pressure are detected, the hypothalamus responds by triggering the release of ADH from the pituitary into the blood, which acts on the kidneys to help retain water (INFOGRAPHIC 25.6).
The amount of water in the bloodstream controls the concentration of dissolved molecules in the blood and also determines blood volume and blood pressure. The kidneys control water availability by responding to a variety of signals.
With these multiple sensors for detecting dehydration, why do we feel less thirsty in the cold? The reason, says Kenefick, is that peripheral vasoconstriction pushes blood toward the core. All that blood pushed centrally is sensed by the body as a normal amount of hydration. As a result, the sensation of thirst is reduced, despite the fact that you’re dehydrated. This is why it’s very important to drink adequate amounts of water in winter, even when you aren’t thirsty.
561
“Because water plays such a large role in cellular function,” says Kenefick, “being dehydrated is going to put a greater stress on your body.” Dehydration can alter the concentration of electrolytes in the blood, and therefore alter nerve function and muscle contraction. Dehydration also lowers blood pressure and thus makes the heart work harder. Together, these effects can have dangerous consequences, impairing thinking and coordination—two things that matter a great deal when you’re navigating the treacherous terrain of the world’s tallest mountain during a blizzard.