CHAPTER 26 Test Your Knowledge
DRIVING QUESTION 1
What is the anatomy of the digestive system?
By answering the questions below and studying Infographics 26.1, 26.2,26.3, 26.6, and 26.7, you should be able to generate an answer for the broader Driving Question above.
KNOW IT
 Place the following structures of the digestive system in order from the entry of food (1) to the exit of waste (5).
Place the following structures of the digestive system in order from the entry of food (1) to the exit of waste (5).
________ Esophagus
________ Large intestine
________ Stomach
________ Mouth
________ Small intestine
(1) mouth; (2) esophagus; (3) stomach; (4) small intestine; (5) large intestine
 Which part of the digestive tract has the most acidic pH?
Which part of the digestive tract has the most acidic pH?
a. esophagus
b. colon
c. small intestine
d. stomach
e. mouth
d
 Why is it helpful to have an expandable stomach?
Why is it helpful to have an expandable stomach?
By having an expandable stomach you can eat more at one time than you can immediately process. The stomach will expand to store the extra food until there is room in the small intestine. If the stomach were not expandable, we would have to continuously eat small amounts of food throughout the day.
USE IT
 What do the gallbladder, liver, and pancreas have in common with respect to the digestive system? How do they differ from the mouth, stomach, and small intestine?
What do the gallbladder, liver, and pancreas have in common with respect to the digestive system? How do they differ from the mouth, stomach, and small intestine?
The gallbladder, liver, and pancreas all produce or store and release secretions (e.g., digestive enzymes, bile, bicarbonate) that aid in digestion. They are not part of the main tube of the digestive tract and food does not pass through the gallbladder, liver, or pancreas. The mouth, stomach, and small intestine are all part of the main tube of the digestive tract through which food passes as it is digested.
 Muscle paralysis in the digestive tract would compromise which digestive function?
Muscle paralysis in the digestive tract would compromise which digestive function?
a. chemical digestion in the stomach
b. chemical digestion in the small intestine
c. absorption in the small intestine
d. chemical digestion in the mouth
e. movement of food from the mouth to the stomach
e
 Pepsin is most effective at a pH of about 2. Digestive enzymes in the small intestine are most effective at a pH of or near 7. If the pancreas were unable to secrete bicarbonate (the basic component of pancreatic secretions), what would you predict about the waste eliminated from the large intestine?
Pepsin is most effective at a pH of about 2. Digestive enzymes in the small intestine are most effective at a pH of or near 7. If the pancreas were unable to secrete bicarbonate (the basic component of pancreatic secretions), what would you predict about the waste eliminated from the large intestine?
If the pancreas were unable to secrete bicarbonate, the acidic chyme from the stomach would not be neutralized (it would remain acidic). The digestive enzymes of the small intestine cannot work at this pH, so the digestion that normally takes place in the small intestine would not occur. This would mean that eliminated waste would contain food that is only partially digested.
DRIVING QUESTION 2
How is food broken down and utilized as it moves through the digestive tract?
By answering the questions below and studying Infographics 26.4 and 26.5, you should be able to generate an answer for the broader Driving Question above.
KNOW IT
 Where does the majority of chemical digestion take place?
Where does the majority of chemical digestion take place?
a. small intestine
b. esophagus
c. mouth
d. stomach
e. colon
a
 What do pepsin and salivary amylase have in common? How do their activities differ?
What do pepsin and salivary amylase have in common? How do their activities differ?
They are both digestive enzymes. Pepsin digests proteins in the stomach, an environment with an acidic pH. Salivary amylase digests carbohydrates in the mouth, an environment with a neutral pH.
 What organ produces lipase?
What organ produces lipase?
Lipase is produced by the pancreas.
USE IT
 A person who has had the gallbladder surgically removed will have trouble processing
A person who has had the gallbladder surgically removed will have trouble processing
a. fats.
b. carbohydrates.
c. minerals.
d. vitamins.
e. proteins.
a
 Compare and contrast the roles of bile salts and lipase.
Compare and contrast the roles of bile salts and lipase.
Both are involved in the processing of fats. Bile salts emulsify fats into small droplets that lipase can digest.
 Why would someone with a blocked duct between the pancreas and the small intestine experience pancreatic inflammation (pancreatitis)? Note that in this case inflammation is a response to tissue damage.
Why would someone with a blocked duct between the pancreas and the small intestine experience pancreatic inflammation (pancreatitis)? Note that in this case inflammation is a response to tissue damage.
The duct between the pancreas and the small intestine allows digestive enzymes from the pancreas to reach the small intestine. If that duct is blocked, the digestive enzymes will remain in the pancreas and begin to digest the pancreatic tissue.
 If you stand on your head, can processed food still pass from your small intestine into your large intestine? Explain your answer.
If you stand on your head, can processed food still pass from your small intestine into your large intestine? Explain your answer.
Yes. Food will still pass from the small intestine into the large intestine because the movement of food through the digestive tract is propelled by peristalsis, not gravity.
MINI CASE
 Alicia has had her gallbladder removed. She must be careful not to eat high-fat meals, or else she is likely to experience greasy diarrhea. Her friend Tammy, who is taking Alli, must also avoid high-fat meals, in order to avoid oily stools, a possible side effect of the drug. Why are both Alicia and Tammy at risk for similar digestive upsets when their situations are different (gallbladder removal, taking Alli)?
Alicia has had her gallbladder removed. She must be careful not to eat high-fat meals, or else she is likely to experience greasy diarrhea. Her friend Tammy, who is taking Alli, must also avoid high-fat meals, in order to avoid oily stools, a possible side effect of the drug. Why are both Alicia and Tammy at risk for similar digestive upsets when their situations are different (gallbladder removal, taking Alli)?
Alicia cannot store bile salts because her gallbladder has been removed. This means that if she eats a high-fat meal, she will not have enough bile salts to emulsify the fat. If the fat is not properly emulsified, it cannot be completely digested, and so will pass into the stool. Tammy can emulsify fat but then can’t fully digest it because Alli inhibits the enzyme lipase. Thus, both Alicia and Tammy are unable to completely digest fats. If they eat a high-fat meal, undigested fat will pass into their stool.
DRIVING QUESTION 3
What are the risks and benefits of bariatric surgery?
By answering the questions below and studying Infographics 26.3, 26.6, and 26.8, you should be able to generate an answer for the broader Driving Question above.
KNOW IT
 Gastric bypass surgery causes the ________ to become ______.
Gastric bypass surgery causes the ________ to become ______.
a. stomach; smaller
b. small intestine; larger
c. stomach; less acidic
d. small intestine; less acidic
e. stomach; larger
a
 Compare and contrast gastric banding and gastric bypass.
Compare and contrast gastric banding and gastric bypass.
Gastric banding reduces the size of the stomach by an adjustable band, producing a small pouch. This pouch cannot hold much food, restricting the amount that a person can eat. The food still passes from the stomach pouch to the small intestine in a normal fashion. In gastric bypass, a small pouch at the top of the stomach is surgically created, and surgery reroutes the passage of food directly from the stomach to the portion of the small intestine that is past the duodenum.
 Which of the following is the best first option for someone who wishes to lower a BMI of 32?
Which of the following is the best first option for someone who wishes to lower a BMI of 32?
a. gastric banding
b. gastric bypass
c. dietary modification
d. more exercise
e. all of the above
f. c and d
f
USE IT
 Several studies have found that gastric bypass has a greater impact on several conditions (e.g., cardiovascular disease and diabetes) than gastric banding. Why might this be?
Several studies have found that gastric bypass has a greater impact on several conditions (e.g., cardiovascular disease and diabetes) than gastric banding. Why might this be?
Because gastric bypass reroutes food, bypassing most of the stomach and part of the small intestine, not only is less food taken in, but less food (and fewer nutrients) are digested and absorbed. Thus, fewer Calories and nutrients (e.g., fatty acids) are absorbed. This can have a dramatic impact on conditions such as diabetes and cardiovascular disease.
BRING IT HOME
 If a morbidly obese person who is considering gastric bypass surgery asked for your opinion on the procedure, what would you say about its known risks, benefits, and any unknowns? Would you say the same to someone considering the surgery who is simply overweight, not morbidly obese? Explain your answer.
If a morbidly obese person who is considering gastric bypass surgery asked for your opinion on the procedure, what would you say about its known risks, benefits, and any unknowns? Would you say the same to someone considering the surgery who is simply overweight, not morbidly obese? Explain your answer.
The surgery has risks, and even if the procedure is successful, patients have to make permanent changes in the way they eat in order to avoid symptoms that range from uncomfortable to painful. There are risks for vitamin deficiencies following the surgery. While almost everyone who undergoes this surgery loses weight at first, many gain some or even all of the weight back. For those who are extremely overweight, the weight loss associated with the surgery can reduce the risk of conditions such as diabetes and cardiovascular disease. Anyone considering this surgery should consult with a surgeon who specializes in weight-loss surgery, should get a second opinion, and should carefully read materials on the risks and benefits. Those who are overweight (but not morbidly obese) may want to consider consulting with a physician to discuss their general health, the risks associated with their current weight, the risks and challenges associated with the surgery, and nonsurgical options for weight management.
INTERPRETING DATA
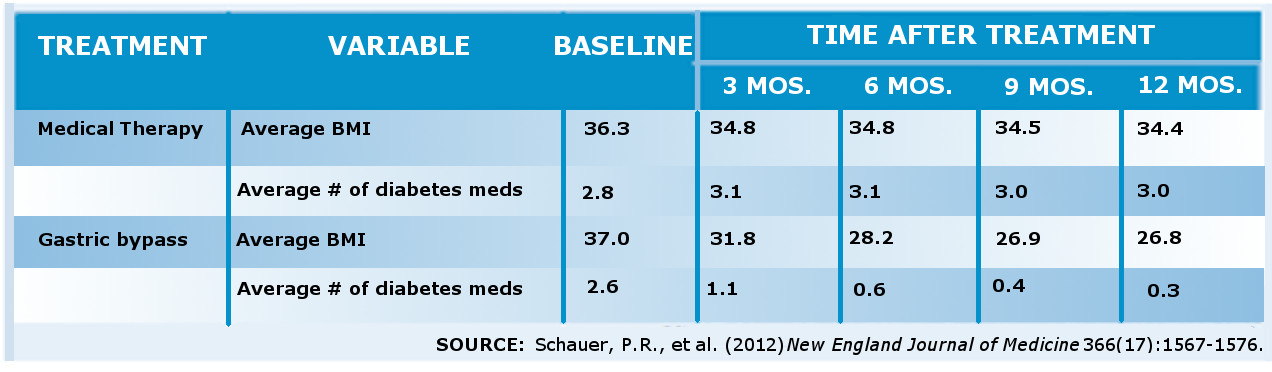
 A 2012 study compared the impacts of medical therapy and bariatric surgery in obese people with uncontrolled type 2 diabetes. Patients were randomly assigned to receive aggressive medical therapy for their diabetes (including medications and diet and lifestyle modifications) or bariatric surgery. Several dependent variables were measured for 1 year. Two of these—average BMI and average number of diabetes medications—are shown in the table below.
A 2012 study compared the impacts of medical therapy and bariatric surgery in obese people with uncontrolled type 2 diabetes. Patients were randomly assigned to receive aggressive medical therapy for their diabetes (including medications and diet and lifestyle modifications) or bariatric surgery. Several dependent variables were measured for 1 year. Two of these—average BMI and average number of diabetes medications—are shown in the table below.
a. Draw two graphs, one plotting the average diabetes medications over time for the group receiving medical therapy and for the group receiving surgery, and one plotting the change in BMI from baseline for the two groups (set the baseline values at 0 on the time axis because by definition no change can have taken place yet).
b. From these graphs, how does gastric bypass compare to medical therapy for diabetes management in obese patients with type 2 diabetes?
c. The data shown in the table are for 41 patients who had medical therapy and 50 patients who had gastric bypass. From this additional information and any other limitations you can identify, are these data sufficient to make a recommendation of surgery for diabetes management? Why or why not?
a: Graphs are not included in answer key. b: Those who had gastric bypass were able to reduce their average number of diabetes medications in 1 year. Those who received medical therapy for their diabetes did not appear to have a substantial change in the number of diabetes medications that they took in the 12 months of the study. c: While the results are encouraging for the impact of gastric bypass on diabetes management in obese individuals who have diabetes, this was a small study, and there has been only a 1-year follow-up. The weight loss seemed to be leveling off at the end of the study, and we don't know what will happen with respect to diabetes management in participants who regain the weight. It would be important to see this study replicated with more participants and a longer follow-up period before making any recommendations regarding the role of gastric bypass in diabetes management.