
 DRIVING QUESTIONS
DRIVING QUESTIONS
- What structural features are shared by all cells, and what are the key differences between prokaryotic and eukaryotic cells?
- How do solutes and water cross membranes, and what determines the direction of movement of solutes and water in different situations?
- How do antibiotics target bacteria, and in what situations is antibiotic therapy indicated?
- What are some key eukaryotic organelles and their functions?
In-Class Activity
Click here to access Lecture ppt specifically designed for chapter 3.
Click here to access Clicker Questions specifically designed for chapter 3.
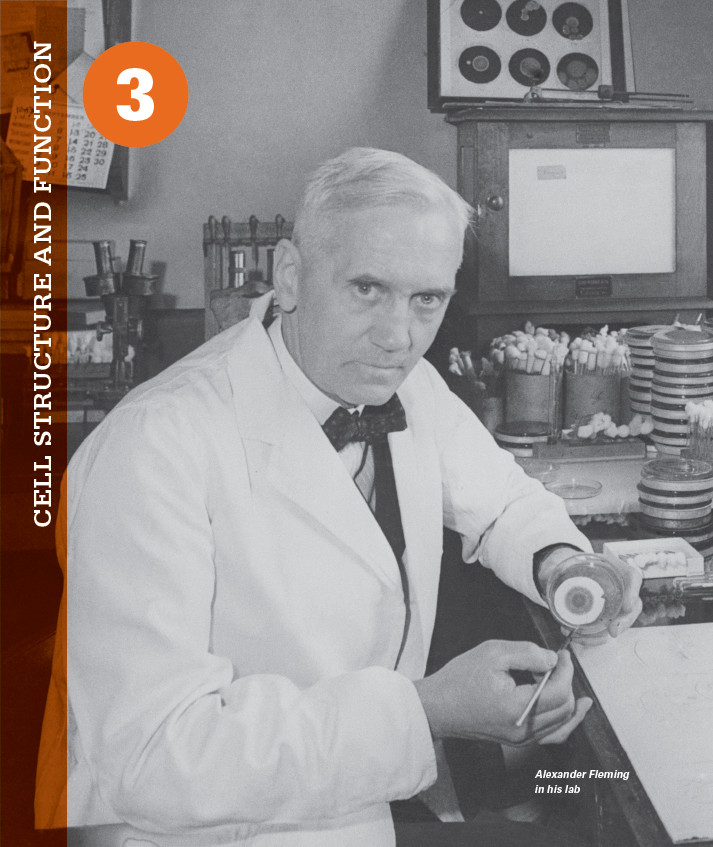
 N A SEPTEMBER MORNING IN 1928, BIOLOGIST ALEXANDER Fleming returned to his laboratory at St. Mary’s Hospital in London after a short summer vacation. As usual, the place was a mess. Flasks were scattered everywhere, and his bench was strewn with the petri plates on which he was growing bacteria. On this day, as Fleming sorted through the plates, he noticed that one was growing a patch of fluffy white mold. It had been contaminated, likely by a rogue mold spore that had drifted in from a neighboring laboratory.
N A SEPTEMBER MORNING IN 1928, BIOLOGIST ALEXANDER Fleming returned to his laboratory at St. Mary’s Hospital in London after a short summer vacation. As usual, the place was a mess. Flasks were scattered everywhere, and his bench was strewn with the petri plates on which he was growing bacteria. On this day, as Fleming sorted through the plates, he noticed that one was growing a patch of fluffy white mold. It had been contaminated, likely by a rogue mold spore that had drifted in from a neighboring laboratory.
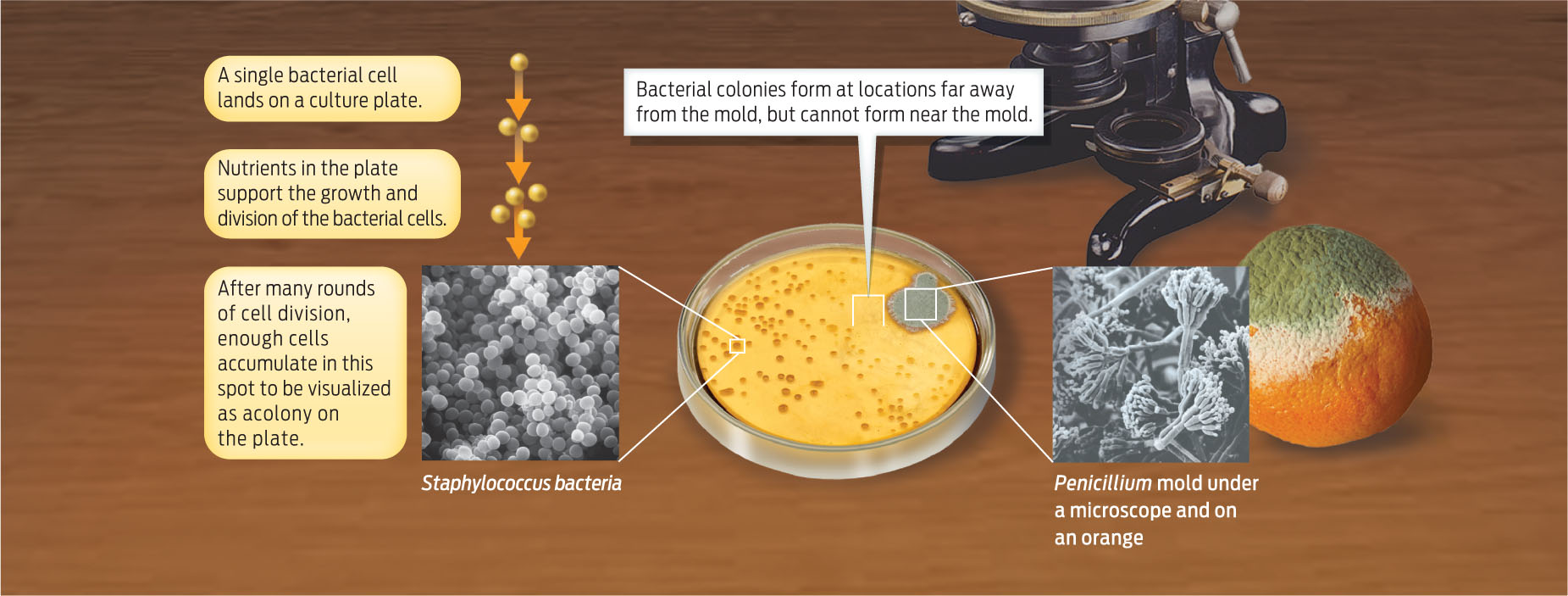
Fleming was about to toss the plate in the sink when he noticed something unusual: wherever mold was growing, there was a zone around the mold where the bacteria did not seem to grow. Curious, he looked under a microscope and saw that the bacterial cells near the mold had burst, or lysed. Something in the mold was killing the bacteria.
ANTIBIOTIC A chemical that can slow or stop the growth of bacteria; many antibiotics are produced by living organisms.
Fleming scooped a bit of mold from the plate, grew it in culture broth, then tested the liquid in a slew of additional experiments. The results were clear and dramatic: even when diluted 800 times, this “mold juice”—Fleming’s term—was a potent killer of many different kinds of bacteria. Moreover, no other fungus that he tested–including one obtained from a pair of moldy old shoes–had this remarkable killing power. Fleming published his results in 1929 in the British Journal of Experimental Pathology. He named the antibacterial substance “penicillin,” after the fungus that produces it, Penicillium notatum. It was the birth of the first antibiotic (INFOGRAPHIC 3.1).
A fortuitous observation by Fleming led to the discovery of the first antibiotic. He realized that the fungus on his culture plate was somehow inhibiting the reproduction of bacteria.
Fleming was not the first to notice the bacteria-killing property of Penicillium, but he was the first to study it scientifically and publish the results. In fact, Fleming had been looking for bacteria-killing substances for a number of years, ever since he had served as a medical officer in World War I and witnessed soldiers dying from bacteria-caused infections. He had already discovered one such antibacterial agent–the chemical lysozyme–which he detected in his own tears and nasal mucus. Nevertheless, his 1928 discovery was serendipitous: “Penicillin started as a chance observation,” Fleming said many years later. “My only merit is that I did not neglect the observation and that I pursued the subject as a bacteriologist.”
Most people have seen the Penicillium fungus growing on a piece of moldy bread or rotting fruit. It doesn’t look very impressive, but the chemical it produces ushered in a whole new age of medicine. For the first time, doctors had a way to treat such deadly bacteria-caused illnesses as pneumonia, syphilis, gonorrhoea, and meningitis. Before penicillin, there was nothing much doctors could do for a patient with a serious bacterial infection. Now, they had a powerful weapon on their side. As physician and author Lewis Thomas recalled in his 1992 memoir, The Fragile Species, “We could hardly believe our eyes on seeing that bacteria could be killed off without at the same time killing the patient. It was not just amazement, it was a revolution.”