4.5 The Body Senses: More Than Skin Deep
Vision and audition provide information about the world at a distance. By responding to light and sound energy in the environment, these “distance” senses allow us to identify and locate the objects and people around us. In comparison, the body senses, also called somatosenses (soma from the Greek for “body”), are up close and personal. Haptic perception is the active exploration of the environment by touching and grasping objects with our hands. We use sensory receptors in our muscles, tendons, and joints as well as a variety of receptors in our skin to get a feel for the world around us (see FIGURE 4.26).
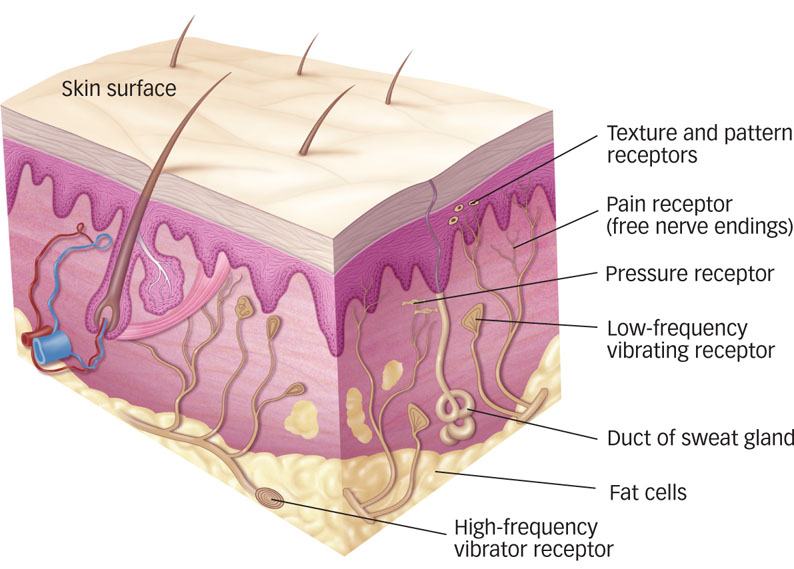
 Figure 4.26: Touch Receptors Specialized sensory neurons form distinct groups of haptic receptors that detect pressure, temperature, and vibrations against the skin. Touch receptors respond to stimulation within their receptive fields, and their long axons enter the brain via the spinal or cranial nerves. Pain receptors populate all body tissues that feel pain; they are distributed around bones and within muscles and internal organs as well as under the skin surface. Both types of pain receptors (the fibers that transmit immediate, sharp pain sensations quickly and those that signal slow, dull pain that lasts and lasts) are free nerve endings.
Figure 4.26: Touch Receptors Specialized sensory neurons form distinct groups of haptic receptors that detect pressure, temperature, and vibrations against the skin. Touch receptors respond to stimulation within their receptive fields, and their long axons enter the brain via the spinal or cranial nerves. Pain receptors populate all body tissues that feel pain; they are distributed around bones and within muscles and internal organs as well as under the skin surface. Both types of pain receptors (the fibers that transmit immediate, sharp pain sensations quickly and those that signal slow, dull pain that lasts and lasts) are free nerve endings.
Touch

Touch begins with the transduction of skin sensations into neural signals. Four types of receptors located under the skin’s surface enable us to sense pressure, texture, pattern, or vibration against the skin (see FIGURE 4.26). The receptive fields of these specialized cells work together to provide a rich tactile (from Latin, “to touch”) experience when you explore an object by feeling it or attempting to grasp it. In addition, thermoreceptors, nerve fibers that sense cold and warmth, respond when your skin temperature changes. All these sensations blend seamlessly together in perception, of course, but detailed physiological studies have successfully isolated the parts of the touch system (Hollins, 2010; Johnson, 2002).
Why might discriminating spatial detail be important for fingertips and lips?

There are three important principles regarding the neural representation of the body’s surface. First, the left half of the body is represented in the right half of the brain and vice versa. Second, just as more of the visual brain is devoted to foveal vision where acuity is greatest, more of the tactile brain is devoted to parts of the skin surface that have greater spatial resolution. Regions such as the fingertips and lips are very good at discriminating fine spatial detail, whereas areas such as the lower back are quite poor at that task. Think back to the homunculus you read about in the Neuroscience and Behavior chapter; you’ll recall that different locations on the body project sensory signals to different locations in the somatosensory cortex in the parietal lobe. Third, there is mounting evidence for a distinction between “what” and “where” pathways in touch analogous to similar distinctions we’ve already considered for vision and audition. The “what” system for touch provides information about the properties of surfaces and objects; the “where” system provides information about a location in external space that is being touched or a location on the body that is being stimulated (Lederman & Klatzky, 2009). fMRI evidence suggests that the “what” and “where” touch pathways involve areas in the lower and upper parts of the parietal lobe, respectively (Reed, Klatzky, & Halgren, 2005).
164
Touch information can have a powerful effect on our decisions and judgments. For example, recent research has shown that merely touching an object that we don’t already own can increase our feeling of ownership and lead us to value the object more highly than when we view it but don’t touch it (Peck & Shu, 2009); the longer we touch an object, the more highly we value it (Wolf, Arkes, & Muhanna, 2008). You might keep this “mere touch” effect in mind next time you are in a shop and considering buying an expensive item. Retailers are probably aware of this effect: During the 2003 holiday shopping season the office of the Illinois state attorney general warned shoppers to be cautious in stores that encouraged them to touch the merchandise (Peck & Shu, 2009).
Pain
Does the possibility of a life free from pain seem appealing? Although pain is arguably the least pleasant of sensations, this aspect of touch is among the most important for survival: Pain indicates damage or potential damage to the body. Without the ability to feel pain, we might ignore infections, broken bones, or serious burns. Congenital insensitivity to pain, a rare inherited disorder that specifically impairs pain perception, is more of a curse than a blessing: Children who experience this disorder often mutilate themselves (e.g., biting into their tongues or gouging their skin while scratching) and are at increased risk of dying during childhood (Nagasako, Oaklander, & Dworkin, 2003).
Tissue damage is transduced by pain receptors, the free nerve endings shown in Figure 4.26. Researchers have distinguished between fast-
As you’ll remember from the chapter on Neuroscience and Behavior, the pain withdrawal reflex is coordinated by the spinal cord. No brainpower is required when you touch a hot stove; you retract your hand almost instantaneously. But neural signals for pain—
Pain typically feels as if it comes from the site of the tissue damage that caused it. If you burn your finger, you will perceive the pain as originating there. But we have pain receptors in many areas besides the skin: around bones and within muscles and internal organs as well. When pain originates internally, in a body organ, for example, we actually feel it on the surface of the body. This kind of referred pain occurs when sensory information from internal and external areas converges on the same nerve cells in the spinal cord. One common example is a heart attack: Victims often feel pain radiating from the left arm rather than from inside the chest.
165

Pain intensity cannot always be predicted solely from the extent of the injury that causes the pain (Keefe, Abernathy, & Campbell, 2005). For example, turf toe sounds like the mildest of ailments; it is pain at the base of the big toe as a result of bending or pushing off repeatedly, as a runner or football player might do during a sporting event. This small-
Some recent evidence indicates subjective pain intensity may differ among ethnic groups (Campbell & Edwards, 2012). For example, a study that examined responses to various kinds of experimentally induced pain, including heat pain and cold pain, found that compared to White young adults, African American young adults had a lower tolerance for several kinds of pain and rated the same pain stimuli as more intense and unpleasant (Campbell, Edwards, & Fillingim, 2005).
Why does rubbing an injured area sometimes help alleviate pain?
One influential account of pain perception is known as gate-control theory of pain, which holds that signals arriving from pain receptors in the body can be stopped, or gated, by interneurons in the spinal cord via feedback from two directions (Melzack & Wall, 1965). Pain can be gated by the skin receptors, for example, by rubbing the affected area. Rubbing your stubbed toe activates neurons that “close the gate” to stop pain signals from traveling to the brain. Pain can also be gated from the brain by modulating the activity of pain-
The neural feedback comes from a region in the midbrain called the periaqueductal gray (PAG). Under extreme conditions, such as high stress, naturally occurring endorphins can activate the PAG to send inhibitory signals to neurons in the spinal cord that then suppress pain signals to the brain, thereby modulating the experience of pain. The PAG is also activated through the action of opiate drugs, such as morphine.
A different kind of feedback signal can increase the sensation of pain. This system is activated by events such as infection and learned danger signals. When we are quite ill, what might otherwise be experienced as mild discomfort can feel quite painful. This pain facilitation signal presumably evolved to motivate people who are ill to rest and avoid strenuous activity, allowing their energy to be devoted to healing.
Although some details of the gate-
166
Body Position, Movement, and Balance
It may sound odd, but one aspect of sensation and perception is knowing where parts of your body are at any given moment. Your body needs some way to sense its position in physical space other than moving your eyes constantly to visually check the location of your limbs. Sensations related to position, movement, and balance depend on stimulation produced within our bodies. Receptors in the muscles, tendons, and joints signal the position of the body in space, whereas information about balance and head movement originates in the inner ear.

Sensory receptors provide the information we need to perceive the position and movement of our limbs, head, and body. These receptors also provide feedback about whether we are performing a desired movement correctly and how resistance from held objects may be influencing the movement. For example, when you swing a baseball bat, the weight of the bat affects how your muscles move your arm as well as the change in sensation when the bat hits the ball. Muscle, joint, and tendon feedback about how your arms actually moved can be used to improve performance through learning.
Maintaining balance depends primarily on the vestibular system, the three fluid-
Why is it so hard to stand on one foot with your eyes closed?
Vision also helps us keep our balance. If you see that you are swaying relative to a vertical orientation, such as the contours of a room, you move your legs and feet to keep from falling over. Psychologists have experimented with this visual aspect of balance by placing people in rooms that can be tilted forward and backward (Bertenthal, Rose, & Bai, 1997; Lee & Aronson, 1974). If the room tilts enough—
 Sensory receptors on the body send neural signals to locations in the somatosensory cortex, a part of the parietal lobe, which the brain translates as the sensation of touch.
Sensory receptors on the body send neural signals to locations in the somatosensory cortex, a part of the parietal lobe, which the brain translates as the sensation of touch. The experience of pain depends on signals that travel along two distinct pathways. One sends signals to the somatosensory cortex to indicate the location and type of pain, and another sends signals to the emotional centers of the brain that result in unpleasant feelings that we wish to escape. The experience of pain varies across individuals, which is explained by bottom-
The experience of pain depends on signals that travel along two distinct pathways. One sends signals to the somatosensory cortex to indicate the location and type of pain, and another sends signals to the emotional centers of the brain that result in unpleasant feelings that we wish to escape. The experience of pain varies across individuals, which is explained by bottom-up and top- down aspects of the gate- control theory of pain.  Balance and acceleration depend primarily on the vestibular system, but are also influenced by vision.
Balance and acceleration depend primarily on the vestibular system, but are also influenced by vision.
167