9.3 Back to Basics: Hunger
STARVING IN SOMALIA

 Mohamed has never suffered from extreme hunger, but he is very familiar with topics like famine, food shortages, and starvation. Like many Somali Americans, he regularly sends money back home to relatives in need. Without money from family members living in more prosperous countries like the United States, many Somalis would not be able to afford food, medicine, and other necessities. As Mohamed says, “You can’t just leave your family back home to starve.”
Mohamed has never suffered from extreme hunger, but he is very familiar with topics like famine, food shortages, and starvation. Like many Somali Americans, he regularly sends money back home to relatives in need. Without money from family members living in more prosperous countries like the United States, many Somalis would not be able to afford food, medicine, and other necessities. As Mohamed says, “You can’t just leave your family back home to starve.”
In the spring of 2011, the Horn of Africa was hit by a drought that caused Somalia to plunge into one of the greatest humanitarian crises of our time—a famine responsible for the starvation deaths of 250 children every day, or 1 child every 6 minutes (British Broadcasting Company [BBC], 2011, July 22). Refugees poured out of Somalia by the thousands. Desperate for food, they walked for weeks to reach refugee camps in neighboring countries. Aid workers said they encountered wounded children, dehydrated and malnourished, arriving at the camps with no shoes (BBC, 2011, June 28). According to a 2011 report, nearly half of Somalia’s population was in need of “lifesaving assistance” (United Nations, 2011). The situation has since improved, but the country is still reeling from the crisis (Caspani, 2012, January 23).
In the coming pages, we will explore hunger, one of the most powerful motivators of human behavior. You will learn what happens in the brain and body when a person is in dire need of food, either because of external circumstances (a famine) or deep-seated psychological factors (an eating disorder). We will also investigate the causes of overeating. So fasten your waist belt and get ready for a journey into the psychological realm of hunger.
Hungry Brain, Hungry Body
It’s midnight; you are struggling to get through the final pages of your psychology chapter. Suddenly, your stomach lets out a desperate gurgling cry. “Feed me!” Time to heat up that frozen burrito, you say to yourself as you head into the kitchen. But wait! Are you really hungry?
The Stomach and Hunger
LO 8 Discuss how the stomach and the hypothalamus make us feel hunger.
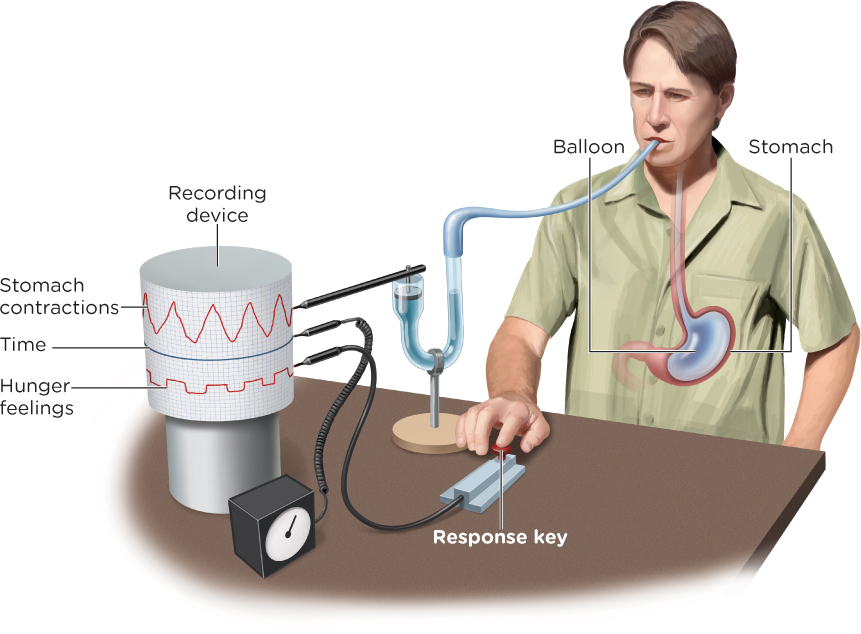
In a classic study, Walter Cannon and A. L. Washburn (1912) sought to answer this question (well, not this exact question, but they did want to learn what causes stomach contractions). Here’s a brief synopsis of the experiment: To help monitor and record his stomach contractions, Washburn swallowed a balloon that the researchers could inflate. The researchers also kept track of Washburn’s hunger levels, having him push a button anytime he felt “hunger pangs” (Figure 9.2). What did the experiment reveal? Anytime he felt hunger, his stomach contracted.
Blood Chemistry and Hunger
Washburn’s experiment demonstrates that the stomach plays an important role in hunger, but it’s just one piece of the puzzle. For example, we know this because people who have had their stomachs surgically removed because of cancer do not differ from people with their stomachs intact in regard to feelings of satiety (that is, feeling full) or the amount of food eaten during a meal (Bergh, Sjöstedt, Hellers, Zandian, & Södersten, 2003). We also must consider the chemicals in the blood, such as glucose, or blood sugar. When glucose levels dip, the stomach and liver send signals to the brain that something must be done about this reduced energy situation. The brain, in turn, will initiate a sense of hunger.
The Hypothalamus and Hunger
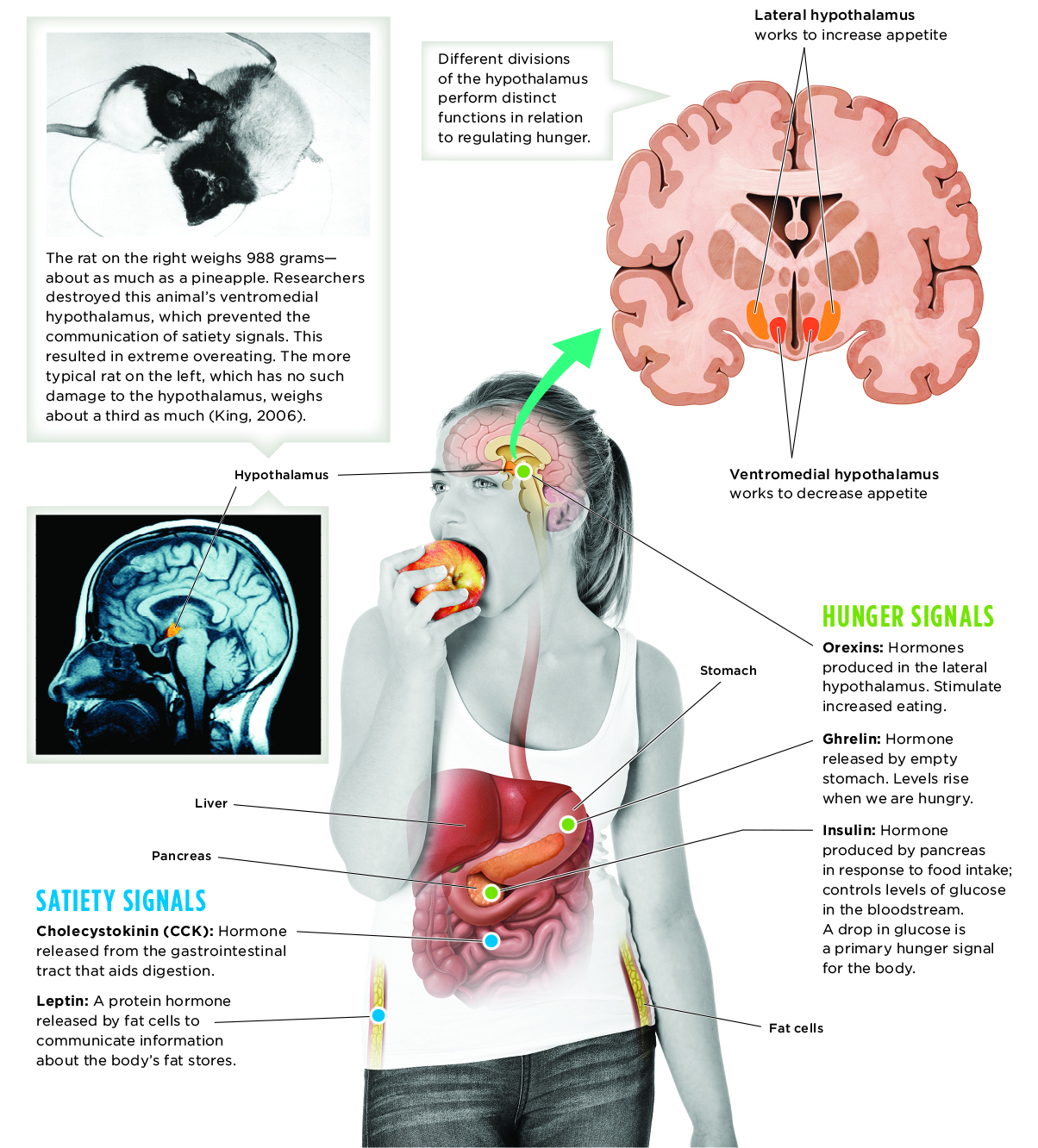
One part of the brain that helps regulate hungry feelings is the hypothalamus, which can be divided into functionally distinct areas. When the lateral hypothalamus is activated, appetite increases. This occurs even in well-fed animals if this region is stimulated electrically. Destroy this area of the brain, and animals lose interest in food, even to the point of starvation. The lateral hypothalamus is also involved in motivating behavior, ultimately helping to preserve the balance between energy supply and demand (Leinninger, 2011).
If the ventromedial hypothalamus becomes activated, appetite declines, causing an animal to stop eating. Disable this region of the brain, and the animal will overeat to the point of obesity. The ventromedial hypothalamus receives information about levels of blood glucose and other feeding-related stimuli, as it too works to maintain the body’s energy balance (King, 2006).
CONNECTIONS
In Chapter 2, we described hormones as chemical messengers released in the bloodstream. Hormones do not act as quickly as neurotransmitters, but their messages are more widely spread throughout the body. Here, we see how hormones are involved in communicating information about hunger and feeding behaviors.
The hypothalamus has a variety of sensors that react to information about appetite and food intake. Once this input is processed, appropriate responses are communicated via hormones in the bloodstream (Infographic 9.2). One such hormone is leptin, a protein emitted by fat cells that plays a role in suppressing hunger. Another is insulin, a pancreatic hormone involved in controlling levels of glucose in the bloodstream. With input from these and other hormones, the brain can monitor energy levels and respond accordingly. This complex system enables us to know when we are hungry, full, or somewhere in between.
Let’s Have a Meal: Cultural and Social Context
CONNECTIONS
In Chapter 1, we discussed naturalistic observation, a form of descriptive research that studies participants in their natural environments. One important feature of this type of study is that researchers do not disturb participants or their environment. Here, we assume the researchers were able to measure and record the meals chosen without interfering in the participants’ natural behaviors.
Biology is not the only factor influencing eating habits. We must also consider the culture and social context in which we eat. In the United States, most of our social activities, holidays, and work events revolve around food. We may not even be hungry, but when presented with a spread of food, we find ourselves eating. All too often we eat too fast, rushing to our next event, class, or meeting, not taking the time to experience the sensation of taste. We tend to match our food intake to those around us, although we may not be aware of their influence (Herman, Roth, & Polivy, 2003; Howland, Hunger, & Mann, 2012). Gender plays a role in eating habits as well. Using naturalistic observation, researchers found that women choose lower-calorie meals when eating with a man than when eating with another woman (Young, Mizzau, Mai, Sirisegaram, & Wilson, 2009).
INFOGRAPHIC 9.2: Mechanisms in Hunger Regulation
We are all aware—sometimes uncomfortably so—when our stomachs are grumbling. But most hunger signals are communicated in an imperceptable cycle throughout our bodies. Feelings of hunger and satisfaction are the result of many independent signals. Different organs are involved in monitoring blood chemistry, prompting the communication of hunger or satiety signals to the brain. These messages are received by the hypothalamus, which regulates basic physiological needs. Separate areas of the hypothalamus then send signals to other parts of the brain, motivating us to increase or decrease eating.
Portion Distortion
A variety of factors drive our decisions to begin or stop eating, including hunger, satiety, and food taste (Vartanian, Herman, & Wansink, 2008). But more subtle variables, such as portion size, come into play, too. In one study, participants at a movie theater were given free popcorn, some in medium-sized buckets and others in large buckets. Some of the buckets contained popcorn that was fresh, and others were filled with popcorn that was 14 days old. Participants given large buckets consistently ate 33% more than those given medium-size buckets, regardless of whether the popcorn was fresh or stale. The stale popcorn was described as “soggy” or “terrible,” yet the participants still ate more of it when given larger portions (Wansink & Kim, 2005). Remember this the next time you sit down in front of the TV with an entire bag of snack food.
Portion size is just one factor influencing food intake. Visual cues are also important, especially when they provide feedback about how much you have eaten. Researchers gave college students tubes of potato chips to eat while watching a movie. In some of the tubes, every 7th chip was dyed red. Participants given tubes with the occasional red chips consumed 50% less than those given tubes with no red chips. Thus we see, interrupting mindless eating (Wait a second, that’s a red chip) can decrease the amount of food consumed in one sitting (Geier, Wansink, & Rozin, 2012).
Perhaps the healthiest approach is to eat small portions throughout the day rather than consuming three huge meals. Dividing up the day with meal breaks may also promote better decision making. At least this appears to be the case in the courtroom.
from the pages of SCIENTIFIC AMERICAN
Lunchtime Leniency
Judges’ rulings are harsher when they are hungrier
Lawyers quip that justice is what the judge ate for breakfast. New research suggests that justice might actually depend onwhen the judge ate breakfast.
Researchers at Ben Gurion University in Israel and Columbia University examined more than 1,000 decisions by eight Israeli judges who ruled on convicts’ parole requests. Judges granted 65 percent of requests they heard at the beginning of the day’s session and almost none at the end. Right after a snack break, approvals jumped back to 65 percent again.
Jonathan Levav, associate professor of business at Columbia, said that the judges could just be grumpy from hunger. But they probably also suffer from mental fatigue. Previous studies have shown that repeated decisions make people tired, and they start looking for simple answers. For instance, after making a slew of choices, car buyers will start accepting the standard options rather than continuing to customize. As sessions drag on, judges may find it easier to deny requests and let things stand as they are.
Levav says he suspects a similar effect occurs in hospitals, university admissions offices or anywhere people make repeated decisions. So if you’re thinking about asking the boss for something special, you might want to do it right after a nice lunch. Kurt Kleiner. Reproduced with permission. Copyright © 2011 Scientific American, a division of Nature America, Inc. All rights reserved.
Obesity
Our discussion on strategies for cutting down food intake provides particularly relevant lessons in today’s world, where a growing number of people struggle with obesity. According to one study, nearly 70% of adults in the United States are overweight, and over 30% meet the criteria for obesity, defined as having a body mass index (BMI) of 30 or higher (Flegal, Carroll, Ogden, & Curtin, 2010). Adults aren’t the only ones battling the bulge; one third of America’s children and teens are overweight (American Heart Association, 2011).
Set Point, Settling Point, and Heredity
Surprisingly, there is relatively little fluctuation in adult weight over time. The communication between the brain and the appetite hormones help regulate the body’s set point, or stable weight that we tend to maintain despite variability in day-to-day exercise and intake of food. If you don’t consume enough calories and your weight falls below this set point, metabolism decreases, causing you to gain weight and return to your set point. Exceed the set point, and metabolism increases, once again moving you back toward your stable weight (Keesey & Hirvonen, 1997). The set point acts like a thermostat, helping to maintain a consistent weight in part through changes in metabolism.

Some critics of the set point model suggest that it fails to appreciate the importance of social and environmental influences (Stroebe, van Koningsbruggen, Papies, & Aarts, 2013). These theorists suggest we should consider a settling point, which is less rigid and can explain how the “set” point can actually change based on the relative amounts of food consumed and energy used. A settling point can help us understand how body weight may shift to a newly maintained weight, and why so many people are overweight as a result of environmental factors, such as bigger meal portions, calorie-dense foods, increased dining at restaurants, and eating while engaged in another activity like watching television—all of which tend to make us eat more and gain weight. Nevertheless, there does seem to be a genetic component of body weight. Studies suggest that the heritability of BMI is around 65% (Speakman et al., 2011). More research is needed, but it seems we may be genetically predisposed to stay within a certain weight range.
CONNECTIONS
In Chapter 7, we presented heritability, the degree to which heredity is responsible for a particular characteristic in a population. The heritability for BMI is 65%, indicating that around 65% of the variation in BMI can be attributed to genes, and 35% to environmental influences.
Overeating, Sleep, and Screen Time
As you well know, deciding what and when to eat does not always come down to being hungry or full. Overeating clearly can have a strong connection to obesity, but there are a variety of reasons why people overeat, including psychological issues (such as depression, anxiety, obsessive-compulsive disorder, and poor impulse control). We must consider how motivation plays a role in what and when we eat. Some people eat not because they are hungry, but because they are bored, sad, or anxious. Others eat simply because the clock indicates that it is mealtime. Higher brain regions involved in eating decisions can override the hypothalamus, driving you to devour that cheesy burrito even when you don’t need the calories.
If our set point works to help us maintain a certain weight, how does this impact people who struggle with obesity? Obesity represents both a physiological and psychological issue. There is some evidence that genes play a role, and we also know some illnesses can lead to obesity (Anis et al., 2010; Plomin et al., 2013). But one often overlooked lifestyle factor related to obesity is sleep. Preliminary research suggests that inadequate sleep is linked to weight problems (a negative correlation between sleep and weight gain). In contrast, individuals who sleep between 6 and 8 hours are more likely to lose weight. A positive correlation exists between screen time and weight gain: the more screen time, the more weight gain. When screen time interferes with making healthy eating choices and getting regular physical exercise, weight loss is not as successful (Elder et al., 2012).
To lose weight, one must eat less and move more (TABLE 9.2). You must use more calories than you are taking in. Our ancestors didn’t have to worry about this. They didn’t have a Starbucks on every street corner to tempt them with that delicious cup of calories. They had to choose foods rich in calories to give them the energy to sustain themselves. Although this was a very efficient means of survival for them, it doesn’t work out so well for us. When experiencing a “famine” (or a decrease in the caloric intake our bodies are accustomed to), our metabolism naturally slows down, requiring fewer calories and making it harder to lose weight.
| Strategies | Description |
|---|---|
| Set realistic goals. | Set goals and expectations that are specific, realistic, and flexible. |
| Get regular exercise. | Exercising just 30 minutes a day 5 times a week can help with weight loss. Add a variety of physical activity to your daily routines. |
| Eat regularly and track intake. | Eat on a set schedule to minimize mindless eating. Eat only when hungry, and write down what and how much you consume by using a food diary. |
| Control portions. | Watch your portions. This is the amount you decide to eat. Read labels to determine the recommended serving size. |
| Drink water. | Eliminate sweetened beverages. |
| Join a weight loss support group. | Social support helps promote healthier coping strategies and accountability. |
| Losing weight is not an easy task, but it doesn’t have to be painful. Making basic lifestyle changes in your daily routines can have significant benefits. | |
| SOURCE: KRUGER, BLANCK, AND GILLESPIE (2006). | |
In response to the obesity problem in the United States, policies have been implemented to raise awareness and discourage overeating. One such intervention is requiring information about calories to be clearly visible, which can serve as a visual cue or reminder. Providing this information can impact healthy food choices. However, accessibility to comparably priced healthy alternatives must be increased (in vending machines, for example)—but this too may require changes in policy (Stroebe et al., 2013).
Eating Disorders
LO 9 Outline the major eating disorders.
Although many people deal with obesity, others struggle with food in a different way. Eating disorders are serious dysfunctions in eating behavior that can involve restricting food consumption, obsessing over weight or body shape, eating too much, and purging (American Psychiatric Association [APA], 2013). Eating disorders usually begin in the early teens and typically affect girls. That doesn’t mean boys do not struggle with eating disorders; 1 in 4 children ages 5–13 with an eating disorder is male (Madden, Morris, Zurynski, Kohn, & Elliot, 2009). However, the causes of body image distortions often differ according to gender. Females desire to be smaller and thinner, whereas males seek an “idealized masculine shape” (Darcy et al., 2012). Let’s take a look at three of the most recognized eating disorders.
Anorexia Nervosa
One of the most commonly known eating disorders is anorexia nervosa, which is characterized by self-imposed restrictions on calories needed to maintain a healthy weight. These restrictions lead to extremely low body weight in relation to age, sex, development, and physical health. Someone with this disorder has an extreme fear of gaining weight and getting fat, even though her body weight is extremely low. Often there is an altered and distorted sense of body weight and figure, as well as no realization of the “seriousness” of her low body weight (APA, 2013). In some cases, women experience an absence of menstrual periods, a condition called amenorrhea (Attia & Roberto, 2009). Other severe symptoms may include brain damage, multi-organ failure, infertility, and thinning of the bones (National Institute of Mental Health [NIMH], 2011). Anorexia is associated with the highest death rates of all psychological disorders (Darcy et al., 2012; Harris & Barraclough, 1998; Smink, van Hoeken, & Hoek, 2012). Approximately 20% of those deaths are due to suicide (Smink et al., 2012). Although anorexia nervosa affects mostly women and adolescent girls, males can also be affected by it (in particular, males involved in wrestling, running, or dancing, who are required to maintain a certain weight).

Bulimia Nervosa
Another eating disorder is bulimia nervosa, which involves recurrent episodes of binge eating, consuming a large amount of food in a short period of time (with that amount being greater than most people would eat in the same time frame). While bingeing, the person feels a lack of control and thus engages in purging behaviors to prevent weight gain (for example, self-induced vomiting, misuse of laxatives, fasting, or excessive exercise; APA, 2013). Like anorexia, bulimia more often affects women and girls (Stice, Marti, Shaw, & Jaconis, 2009). Bulimia also has serious health risks, such as high blood pressure, heart disease, and Type 2 diabetes (Haedt-Matt & Keel, 2011). Other symptoms include decaying teeth, damage to the throat, gastrointestinal disorders, and electrolyte imbalance from vomiting, which can lead to cardiac failure (NIMH, 2011). Research has found that 23% of deaths associated with bulimia nervosa result from suicide (Smink et al., 2012).
Binge-Eating Disorder
You may have also heard of binge-eating disorder (APA, 2013), characterized by episodes of excessive food consumption (eating more than most people would eat in the same amount of time and in similar situations). As in bulimia, the individual feels unable to control her eating during that period of time, but the difference is that she does not engage in excessive weight control or purging behaviors. Some psychological effects could include feelings of embarrassment about how much food has been consumed, depression, and guilt after overeating.
We know that eating disorders are apparent in America—we see evidence of them on television, in magazines, and in everyday life. But are these disorders also observed in India, South Africa, and Egypt? Let’s take a look at eating disorders across the world.
across the WORLD
A Cross-Cultural Look at Eating Disorders
 Close your eyes and imagine the stereotypical beauty queen. Is she curvy like a Coke bottle or long and lean like a Barbie doll? We suspect the image that popped into your mind’s eye looked more like the famed plastic doll. Let’s face it: Western concepts of beauty, particularly female beauty, often go hand-in-hand with thinness.
Close your eyes and imagine the stereotypical beauty queen. Is she curvy like a Coke bottle or long and lean like a Barbie doll? We suspect the image that popped into your mind’s eye looked more like the famed plastic doll. Let’s face it: Western concepts of beauty, particularly female beauty, often go hand-in-hand with thinness.
With all this pressure to be slender, it’s no wonder eating disorders like anorexia and bulimia are most commonly diagnosed and treated in Western societies such as the United States (TABLE 9.3; Keel & Klump, 2003; Littlewood, 2004). Psychologists once believed eating disorders only occurred in regions of the world influenced by Western culture. Anorexia and bulimia were thought to be psychological disorders unique to certain societies. But evidence suggests it is not that simple.
| Treatment Options | Description |
|---|---|
| Counseling and psychotherapy | Treatment may involve individual, group, or family counseling. The focus of counseling and psychotherapy can be on nutrition, psychological issues, or thoughts and behaviors surrounding the eating disorder. |
| Health care and medical monitoring | Many eating disorders result in serious medical crises. Medical monitoring and care are critical when it comes to the patient’s health. |
| Drug therapies | Although drugs will not prevent, cure, or restore an individual to a normal weight, drug therapies may be useful in treating the mood issues (often anxiety and depression) that can accompany eating disorders. |
| Effective treatment of eating disorders often involves a combination of approaches tailored to the individual. This tends to be more effective than one type of treatment alone. | |
| SOURCE: ADAPTED FROM NIMH (2011). | |
Keel and Klump (2003) conducted a large review of studies and concluded that anorexia occurs throughout the non-Western world, from Hong Kong to Malaysia to Iran. They also found evidence of people, particularly young women, starving themselves since medieval times—long before Barbie dolls and runway models began making “normal” people feel “fat.” Fear of fat may be an important factor driving self-starvation, but it is not necessarily the only one. There are other reasons people forgo food—a desire for some type of control, for instance (Simpson, 2002).
THEY…FOUND EVIDENCE OF PEOPLE, PARTICULARLY YOUNG WOMEN, STARVING THEMSELVES SINCE MEDIEVAL TIMES….

However, Keel and Klump (2003) found no evidence of bulimia (based on strict criteria) existing in regions isolated from Western culture. They also determined that the prevalence of the disorder dramatically increased during the second half of the 1900s, just as the fixation with thin was beginning to take hold. This pattern might not be as strong outside of Western culture, but such a fixation with body image is becoming more prevalent across cultures.
We have now explored the many facets of motivation, from basic physiological drives to transcendent needs for achievement. As you may have guessed from the title of this chapter, all these motivations are intimately tied to emotions. To understand motivated behaviors, you can’t ignore emotion. In the sections to come, we will explore the complex world of human emotion, with a focus on fear and happiness.
show what you know
Question 9.9
1. Washburn swallowed a special balloon to record his stomach contractions. He also pressed a button to record his feelings of hunger. The findings indicated that whenever he felt hunger, his:
- stomach was contracting.
- stomach was still.
- blood sugar went up.
- ventromedial hypothalamus was active.
a. stomach was contracting.
Question 9.10
2. Bulimia nervosa is an eating disorder characterized by
- restrictions of energy intake.
- extreme fear of gaining weight, although one’s body weight is extremely low.
- a distorted sense of body weight and figure.
- extreme overeating followed by purging.
d. extreme overeating followed by purging.
Question 9.11
3. Describe how the hypothalamus triggers hunger and its relationship to eating.
When glucose levels dip, the stomach and liver send signals to the brain that something must be done about this reduced energy source. The brain, in turn, initiates a sense of hunger. Signals from the digestive system are sent to the hypothalamus, which then transmits signals to higher regions of the brain. When the lateral hypothalamus is activated, appetite increases. On the other hand, if the ventromedial hypothalamus becomes activated, appetite declines, causing an animal to stop eating.