Video transcript
REPORTER: If you're among millions of Americans who can't get enough sleep, you should know that it could be the root of other health issues, such as obesity. Relief can come in the form of unconventional and non-invasive therapy.
RAE TATTENBAUM: We're going to do a little baseline.
REPORTER (VOICEOVER): Insomnia lead Myron Congdon to seek another alternative to taking sleep medication.
MYRON CONGDON: Sometimes I would get out for a couple of hours, and sometimes I would just simply stay awake and toss around in bed.
REPORTER (VOICEOVER): That would lead to three to four hours of sleep a night.
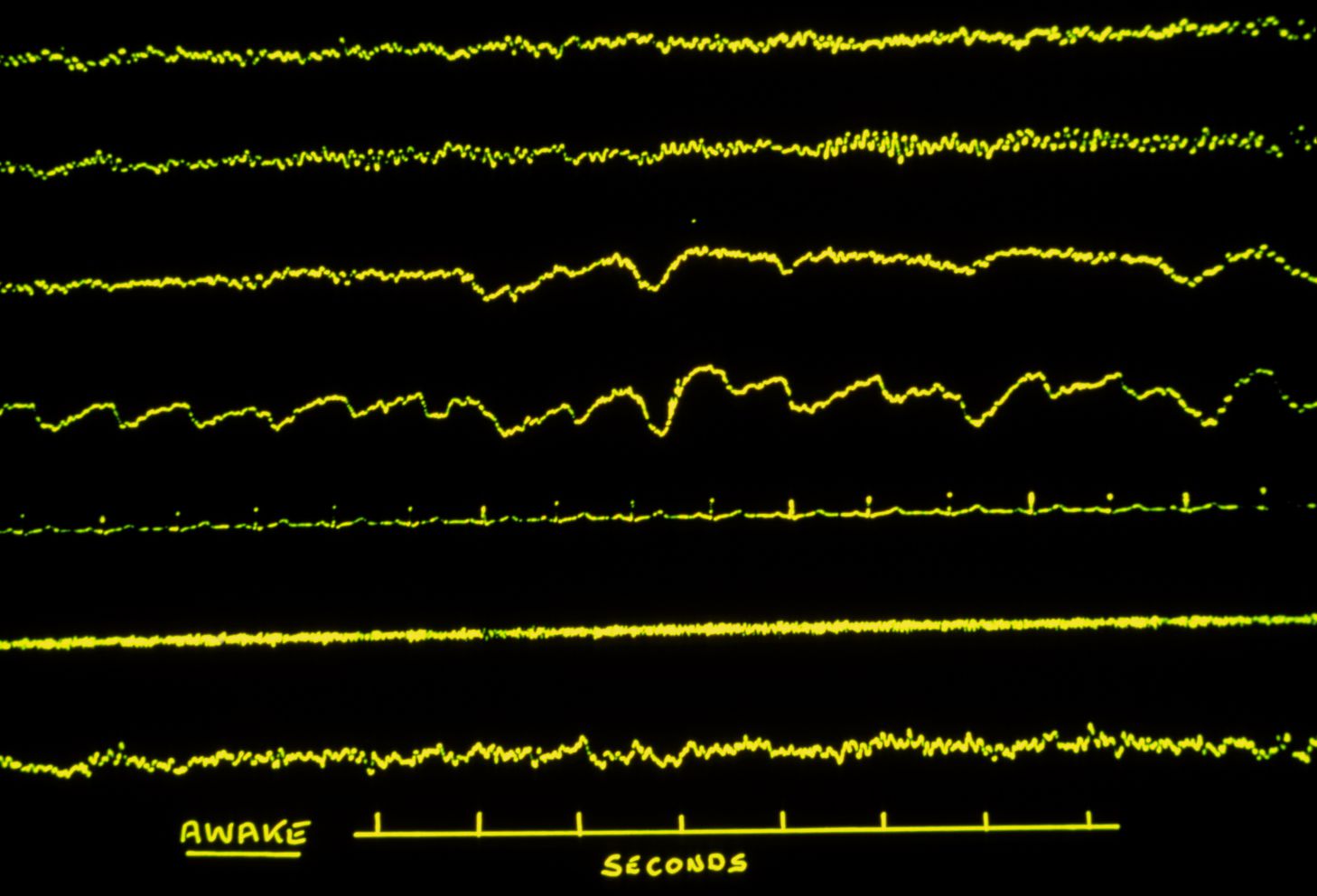
RAE TATTENBAUM: The software is giving his central nervous system feedback.
REPORTER (VOICEOVER): Now Myron is undergoing a mix of neuro and biofeedback
RAE TATTENBAUM: Let the background noise just be background.
REPORTER (VOICEOVER): training perfected by psychotherapist Rae Tattenbaum in West Hartford. Relaxation techniques, she says, can only go so far.
RAE TATTENBAUM: Relaxation is good. However, what we really need is balance. And most people are too tense to practice the relaxation exercises.
REPORTER (VOICEOVER): This technology
RAE TATTENBAUM: He's creating a complete state of balance.
REPORTER (VOICEOVER): monitors the turbulence causing the imbalance in his central nervous system.
RAE TATTENBAUM: What causes turbulence? Worry, aggravation, habits.
REPORTER (VOICEOVER): That turbulence triggers an interruption.
RAE TATTENBAUM: He's hearing an interruption, and what he's feeling is a sense of well-being and relaxation
REPORTER (VOICEOVER): a feeling Myron was deprived of, due to the lack of sleep.
MYRON CONGDON: Fuzzy during the day time, at times. Yawning at times when you don't want to be yawning, when you're supposed to be paying attention to someone else.
REPORTER (VOICEOVER): Weekly sessions have lead to sleeping better.
MYRON CONGDON: What I'm getting is going back to sleep much more often than I was able to before.
RAE TATTENBAUM: With this technology, you sleep an hour longer, and you return to sleep faster.
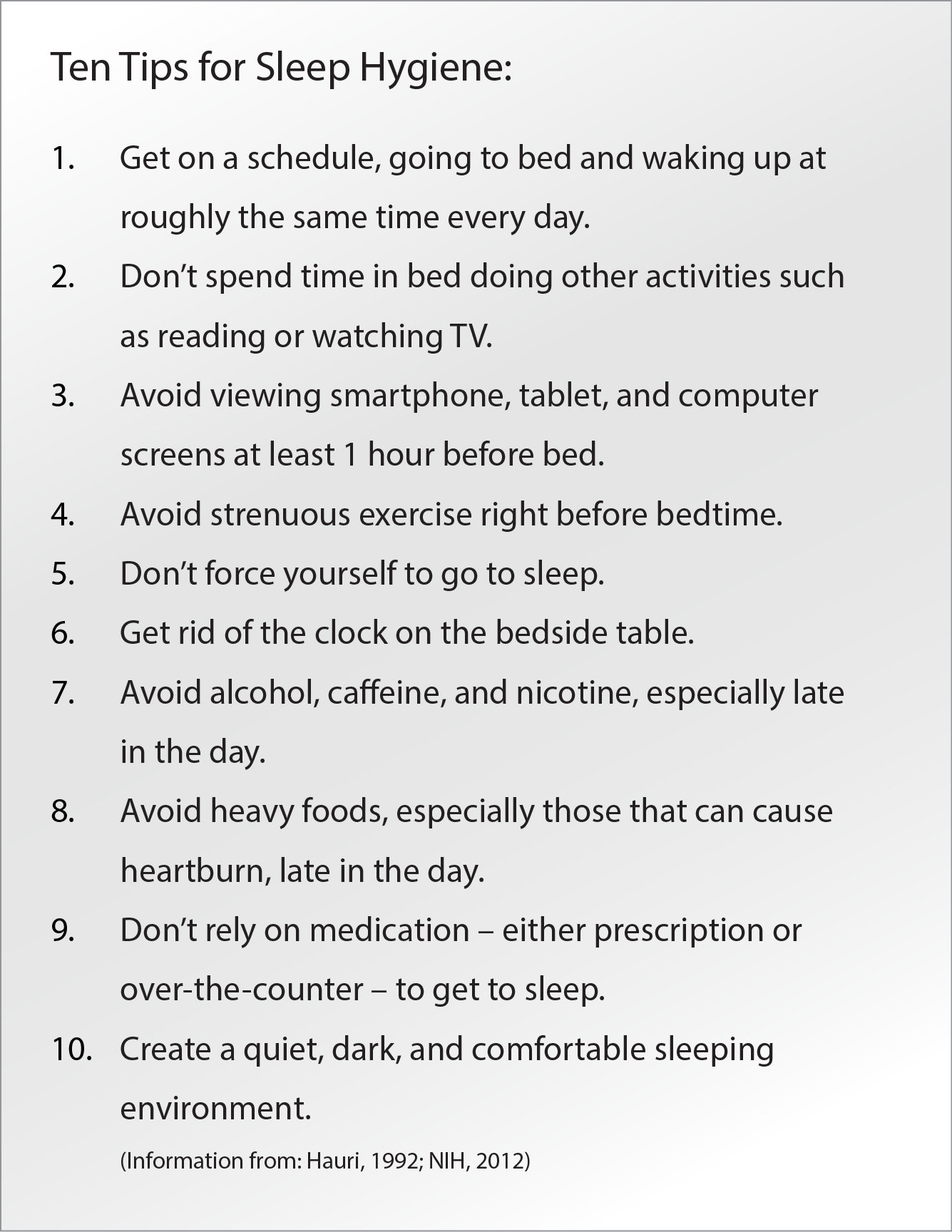
REPORTER (VOICEOVER): Also part of the process-- getting ready to go to sleep.
RAE TATTENBAUM: Breathing patterns, what you watch, what you read before you go to sleep.
REPORTER: The success rate for this training is about 75%.