12.5 Disorders of Personality and Identity
LO 10 Differentiate between antisocial and borderline personality disorders.
personality disorders A group of psychological disorders that can include impairments in cognition, emotional responses, interpersonal functioning, and impulse control.
Before reading this chapter, you probably knew something about depression, bipolar disorder, and schizophrenia. But you may have been less familiar with a somewhat common group of disorders relating to personality. Approximately 1 in 10 adults in the United States has a personality disorder (Lenzenweger, Lane, Loranger, & Kessler, 2007). People with personality disorders exhibit “an enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is stable over time, and leads to distress or impairment” (American Psychiatric Association, 2013, p. 645). Specifically, someone with a personality disorder behaves in a way that deviates substantially in the following areas: (1) cognition, including perceptions of self, others, and events; (2) emotional responses; (3) interpersonal functioning; and (4) impulse control. In order to be diagnosed with a personality disorder, one must struggle in at least two of these four categories. In addition, these problems must be resistant to change and have far-
Like personality traits in general, the core qualities of people with personality disorders (as well as the problems that result) are fairly stable over a lifetime and across situations. When diagnosing this type of disorder, the clinician must focus on troublesome personality traits—
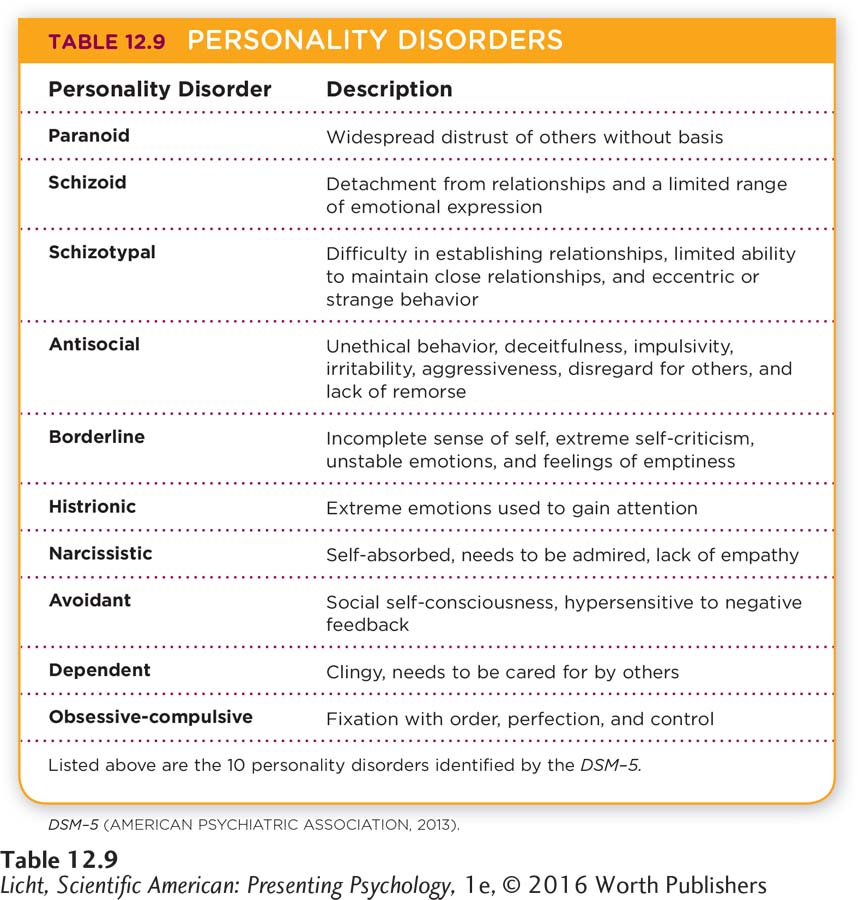
The DSM–
Antisocial Personality Disorder
Swedish actress Noomi Rapace plays the role of Lisbeth Salander in The Girl with the Dragon Tattoo (2009). Salander displays some of the hallmark characteristics of antisocial personality disorder: She seems to feel no remorse about violating social norms, hurting others, and breaking laws. Yet she appears to care about those she avenges, making it hard to place her in this category (Burkley, 2012, January 3).
antisocial personality disorder A psychological disorder distinguished by unethical behavior, deceitfulness, impulsivity, irritability, aggressiveness, disregard for others, and lack of remorse.
Synonyms
antisocial personality disorder psychopathy, sociopathy
Many films, including The Girl with the Dragon Tattoo and The Silence of the Lambs, feature characters who behave in ways most people find incomprehensible. The qualities of these characters often parallel a diagnosis of antisocial personality disorder.
People with antisocial personality disorder may seek personal gratification even when it means violating ethical standards and breaking laws. They sometimes lie or con others, and exhibit aggressive, impulsive, or irritable behaviors. These individuals have difficulty feeling empathy, and may not show concern for others or feel remorse upon hurting them. Other common behavior patterns include carelessness in sexual relationships, and the use of intimidation to control others (American Psychiatric Association, 2013). Around 1% of American adults are diagnosed with antisocial personality disorder, which is more common in men than women (Lenzenweger et al., 2007).
How does antisocial personality disorder develop? There is some evidence for family risk factors, but it is unclear how much of this risk is transmitted through genes, and how much results from learning. Heredity does appear to play a role, as first-
CONNECTIONS
In Chapter 7, we noted that executive functioning is involved in planning, maintaining focus, and suppressing automatic responses. In Chapter 2, we learned that the frontal lobes are critical in processing emotions and controlling impulses. If these areas in the brain are not functioning properly, one may exhibit antisocial behavior.
You may be wondering what is unique about the brain of a person with antisocial personality disorder. Some studies point to irregularities in the frontal lobes, a region of the brain that is crucial for executive functioning. For example, reduced tissue volume in the prefrontal cortex (11% less than expected) is apparent in some men with antisocial personality disorder. This deficit might be linked to reduced morality, and problems in decision making, planning, and learning in relation to fear, all potentially associated with antisocial behavior. The fact that the prefrontal cortex plays a role in controlling arousal may explain why people with this disorder tend to seek out stimulation, including aggressive and antisocial activities (Raine, Lencz, Bihrle, LaCasse, & Colletti, 2000).
Borderline Personality Disorder
Winona Ryder plays the part of ex-
borderline personality disorder A psychological disorder distinguished by an incomplete sense of self, extreme self-
Borderline personality disorder is distinguished by an incomplete sense of self and feelings of emptiness. People with this disorder tend to be emotionally unstable and extremely needy. They may exhibit intense anger, have difficulty controlling their temper, and get into physical fights. They can be impulsive when it comes to sexual activity, substance abuse, and spending money, and may threaten or attempt suicide on a recurring basis. Developing intimacy may also be a struggle, and relationships tend to be unstable, tainted with feelings of mistrust and fear of abandonment. Those with borderline personality disorder may see the world in terms of black and white, rather than different shades of gray. This tendency to perceive extremes may lead a person to become overinvolved or totally withdrawn in relationships (American Psychiatric Association, 2013).
According to the DSM–
Seventy-
As you now know, personality disorders stem from well-
Dissociative Disorders
LO 11 Identify differences among dissociative disorders.
dissociative disorders Psychological disorders distinguished by disturbances in normal psychological functioning; may include problems with memory, identity, consciousness, perception, and motor control.
dissociation A disturbance in the normally integrated experience of psychological functions involved in memory, consciousness, perception, or identity.
Dissociative disorders are disturbances in normal psychological functioning that can include problems with memory, identity, consciousness, perception, and motor control. The main feature of these disorders is dissociation, or a disturbance in the normally unified experience of psychological functions involved in memory, consciousness, perception, or identity (Spiegel et al., 2011). Dissociation may lead to difficulty recalling personal information (for example, where I live, who I am), or the feeling of being detached from one’s body.
In North America and Europe, the prevalence of dissociative disorders imposes a high financial burden (Brand, Classen, McNary, & Zaveri, 2009), in part because of lengthy treatment times. Dissociative disorders generally do not resolve with a simple drug prescription or a couple of therapy sessions. Here, we focus our discussion on two dissociative disorders: dissociative amnesia and dissociative identity disorder.

A young man in São Paulo, Brazil, dances in a trance state during a religious ceremony. Behaviors observed in this type of context may resemble those of dissociative identity disorder, but it is important to differentiate between religious practices and disordered behaviors (Moreira-
dissociative amnesia A psychological disorder marked by difficulty remembering important personal information and life events.
DISSOCIATIVE AMNESIA People suffering from dissociative amnesia have difficulty remembering important personal information. Often the lost memories center on traumatic or stressful events. In some cases the amnesia is localized, or fixed around a certain event; other times it may span a lifetime. Those with dissociative amnesia typically report a great deal of distress or impairment in relationships, work, and other important areas of life, and put a lot of effort into managing the mundane details of daily existence (Staniloiu & Markowitsch, 2012).
dissociative fugue (fyüg) A condition in which a person with dissociative amnesia wanders about in a confused and unexpected manner.
A person with dissociative amnesia who wanders in a confused and unexpected manner may also be experiencing dissociative fugue (fyüg; Spiegel et al., 2011). Consider this example from a case study: A 62-
dissociative identity disorder A psychological disorder that involves the occurrence of two or more distinct personalities within an individual.
DISSOCIATIVE IDENTITY DISORDER Perhaps the most commonly known dissociative disorder is dissociative identity disorder (often referred to as multiple personality disorder), which is characterized by the presence of two or more distinct personalities. Dissociative identity disorder is considered the most complicated and persistent of the dissociative disorders (Sar, 2011). One of its key features is a lack of connection among behavior, awareness, memory, and cognition. There is often a reported gap in remembering day-
Clinicians must be mindful of cross-
WHAT CAUSES DISSOCIATIVE DISORDERS? A great deal of controversy surrounds the apparent increase in diagnoses of dissociative identity disorder in the United States. One possible explanation is that clinicians are reinforcing the development of these dissociations. In other words, by suggesting the possibility of alternate personalities or using hypnosis to “recover” lost memories, the clinician “cues” the individual to believe an alternate personality is responsible for behaviors (Lynn, Lilienfeld, Merckelbach, Giesbrecht, & van der Kloet, 2012). These disorders are difficult to substantiate when they are based on self-
show what you know
Question 1
1. The personality disorders include impairments concerning:
contact with reality.
manic episodes.
developmental processes.
the self and interpersonal relationships.
the self and interpersonal relationships.
Question 2
2. Individuals with ____________ are likely to feel a sense of emptiness, become angry easily, and maintain intense but unstable relationships.
borderline personality disorder
Question 3
3. ____________ is a disturbance in the normally integrated experiences of memory, consciousness, perception, or identity.
Dissociation
Question 4
4. Describe the similarities and differences between dissociative amnesia and dissociative identity disorder.
Answers will vary, but can be based on the following information. The commonality in this group of disorders is dissociation, or disturbance in the normally unified experience of psychological functions involved in memory, consciousness, perception, or identity. Dissociative identity disorder is a psychological disorder that involves the occurrence of two or more distinct personalities within one individual, whereas dissociative amnesia is a psychological disorder that includes a lack of ability to remember important personal information and memories. Both disorders interfere with relationships, memory, work, and other important areas of life.
 DEFYING STIGMA: ROSS LEARNS TO THRIVE After graduating from high school, Ross started college at American University in Washington, DC. But he didn’t have much of a plan for managing his disorder. “What I did was essentially the equivalent of showing up to college in a wheelchair, and hoping they would have ramps,” he recalls in his book Behind Happy Faces (Szabo & Hall, 2007, p. 100).
DEFYING STIGMA: ROSS LEARNS TO THRIVE After graduating from high school, Ross started college at American University in Washington, DC. But he didn’t have much of a plan for managing his disorder. “What I did was essentially the equivalent of showing up to college in a wheelchair, and hoping they would have ramps,” he recalls in his book Behind Happy Faces (Szabo & Hall, 2007, p. 100).
Three weeks into freshman year, Ross had his stomach pumped for alcohol poisoning and, within 2 months, a major relapse with bipolar disorder. He returned to Pennsylvania and was hospitalized. After this, Ross felt like a failure: “I used to sleep on my couch for 18 hours a day or sit out in my backyard and stare out at nothing,” he remembers. “I felt like bipolar disorder had won out, and that there was nothing more I could do about it” (Szabo & Hall, 2007, p. 101).
But then Ross did something. He found employment and began taking classes at a community college, which led to his enrollment at a local 4-
What followed were years of hard work. Ross quit using alcohol and caffeine and smoking cigarettes and marijuana. He imposed structure on his life, waking up and going to sleep at the same time each day, eating regular meals, and exercising. He started being open and honest in his relationships with friends, family, and his therapist. And most important, he confronted his self-

Ross celebrates graduation day at the center for people with disabilities where he worked in Botswana, Africa. After completing his service with the Peace Corps, Ross returned to the United States and founded a consulting group, which designs mental health curricula for middle and high schools.
In 2002 Ross graduated cum laude from American University, and then he picked up where he left off that day he spoke to his high school class about his experience with bipolar disorder. He became a mental health advocate, giving presentations at high schools and colleges across America. As director of youth outreach for the National Mental Health Awareness Campaign, Ross started The Heard (now part of Active Minds), a speakers’ bureau that includes other young presenters who have battled disorders.
After 8 years of working as a mental health advocate, Ross traveled to the African nation of Botswana to serve in the Peace Corps. Upon returning to the United States in 2012, he launched his own consulting group, Human Power Project, which designs cutting-
 OUTSMARTING OCD: MELISSA FINDS A THERAPY THAT WORKS Shortly after leaving the hospital, Melissa found out about a study on OCD treatments at the University of Pennsylvania. She decided to participate and got acquainted with the lead investigator, who became her therapist. “He taught me how to live with OCD,” says Melissa. “He basically saved my life.”
OUTSMARTING OCD: MELISSA FINDS A THERAPY THAT WORKS Shortly after leaving the hospital, Melissa found out about a study on OCD treatments at the University of Pennsylvania. She decided to participate and got acquainted with the lead investigator, who became her therapist. “He taught me how to live with OCD,” says Melissa. “He basically saved my life.”
Melissa had been taking medications since she was 12, but she only experienced a dramatic improvement when she combined her medication with cognitive behavioral therapy (CBT), an approach you can learn about in Chapter 13 on psychological therapies.
Like Ross, Melissa discovered she had a gift for public speaking. At age 19, she decided to share her story, speaking about her battle with OCD as part of a panel hosted by her college, Immaculata University in Pennsylvania. Her presentation moved some of the audience members to tears. From that point forward, Melissa decided to do everything in her power to dispel the stigma of psychological disorders. She started a mental health awareness group on her campus, opening a chapter of the national organization Active Minds, and later joined Ross Szabo’s speakers’ bureau and became a presenter for the mental health organization Minding Your Mind. In 2013, Melissa published a book, The People You Meet in Real Life, which relates the stories of those who have inspired her along the way. She hopes these tales of resiliency and optimism will help readers understand they are not alone in their struggles.

As a presenter for the mental health organization Minding Your Mind, Melissa travels across the country, educating students about mental health issues. She has also published a book, The People You Meet in Real Life, which provides first-
Melissa is now in her late twenties. She still has OCD, but it’s under control. Instead of walking through a doorway 20 times, she now passes through it twice. And the time she once spent sitting alone in her room meticulously touching objects in sets of 2s she now spends talking to classrooms full of students, shattering the stigma surrounding psychological disorders. 