13.4 Biomedical Therapies
Earlier in the chapter, we described Dr. Foster’s work with Chepa, the young woman with schizophrenia. In addition to receiving psychotherapy, Chepa goes to the medical clinic for monthly injections of drugs to control her psychosis. Prescribing medications for psychological disorders is generally the domain of psychiatrists, physicians who specialize in treating people with psychological disorders (psychiatrists are medical doctors, whereas clinical psychologists have PhDs and generally cannot prescribe medication).

Psychotropic medications are typically prescribed by psychiatrists, but a small number of psychologists have prescription privileges as well. New Mexico, Louisiana, and Illinois have passed laws giving psychologists the green light to prescribe, provided they have a master’s degree in psychopharmacology and adequate in-
LO 8 Summarize the biomedical interventions and identify their common goal.
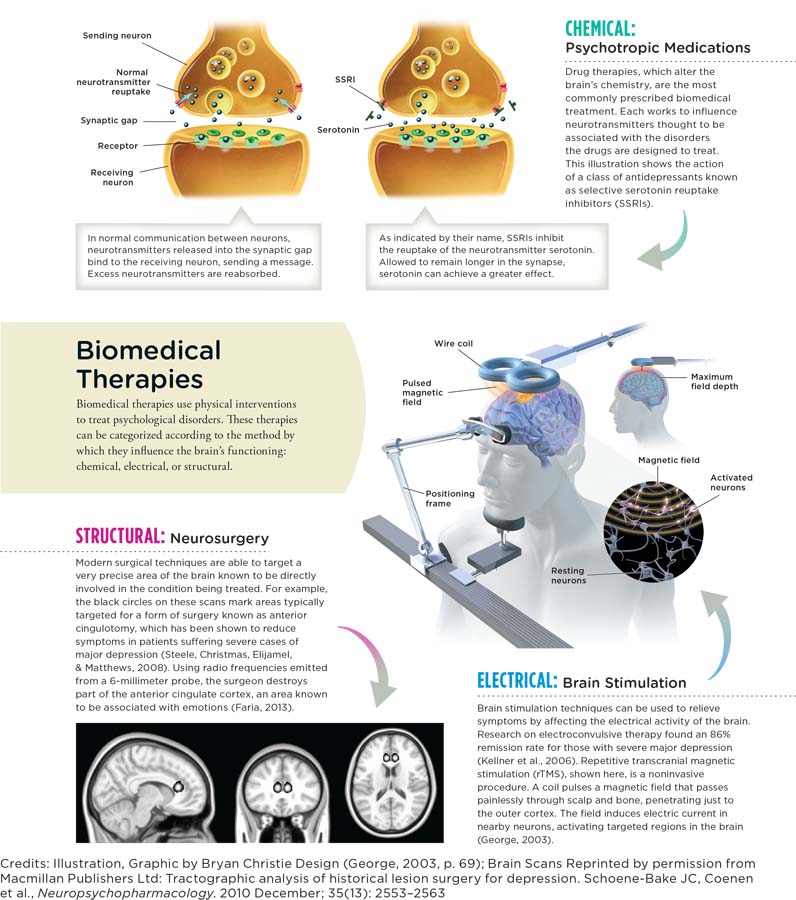
People with severe disorders like depression, schizophrenia, and bipolar disorder often benefit from biomedical therapy, a type of treatment that targets the biological processes underlying psychological disorders. There are three basic biological approaches to treating psychological disorders: (1) the use of drugs, or psychotropic medications; (2) the use of electroconvulsive therapy; and (3) the use of surgery.
Medicines That Help: Psychopharmacology
Psychotropic medications are used to treat psychological disorders and their symptoms. Psychopharmacology is the scientific study of how these medications alter perceptions, moods, behaviors, and other aspects of psychological functioning. These drugs can be divided into four categories: antidepressant, mood-
ANTIDEPRESSANT DRUGS The most common mental health problem plaguing Dr. Foster’s clients is major depressive disorder. Commonly referred to as depression, it is one of the most prevalent psychological disorders in America and a common cause of disability in young adults (National Institute of Mental Health, 2013, October 1). Major depressive disorder affects around 7% of the population in any given year (American Psychiatric Association, 2013), resulting in a high demand for ways to lessen its symptoms.
antidepressant drugs Psychotropic medications used for the treatment of depression.
CONNECTIONS
In Chapter 2, we described how neurons communicate with each other. Sending neurons release neurotransmitters into the synaptic gap, where they bind to receptors on the receiving neuron. Neurotransmitters not immediately attached are reabsorbed by the sending neuron (reuptake) or are broken down in the synapse. Here, we see how medications can influence this process.
Major depressive disorder is commonly treated with antidepressant drugs, a category of psychotropic medication used to improve mood (and to treat anxiety and eating disorders in certain individuals). Essentially, there are three classes of antidepressant drugs: monoamine oxidase inhibitors (MAOIs), such as Nardil; tricyclic antidepressants, such as Elavil; and selective serotonin reuptake inhibitors (SSRIs), such as Prozac. All these antidepressants are thought to work by influencing the activity of neurotransmitters that are hypothesized to be involved in depression and other disorders (Infographic 13.3, below). (Keep in mind, no one has pinpointed the exact neurological mechanisms underlying depression.)
INFOGRAPHIC 13.3
A growing number of children and teenagers are taking SSRIs to combat depression, but these medications may increase the risk of suicidal behaviors and thoughts for a small percentage of youth. For this reason, the U.S. Food and Drug Administration (FDA) requires manufacturers to include a “black box” warning on the packaging of these drugs (National Institute of Mental Health, n.d., para. 3).
The monoamine oxidase inhibitors (MAOIs), developed in the 1950s, help people with major depressive disorder by slowing the breakdown of norepinephrine, serotonin, and dopamine in synapses. These neurotransmitters are categorized as monoamines, and the natural role of the enzyme monoamine oxidase is to break down the monoamines when they are in the synaptic gap. MAOIs extend the amount of time these neurotransmitters linger in the gap by hindering the normal activity of monoamine oxidase. Again, the cause of depression is not entirely clear, but low levels of norepinephrine and serotonin could play a role. By making these neurotransmitters more available (that is, allowing them more time in the synapse), MAOIs might lessen symptoms of depression. Even so, this class of drugs has fallen out of use due to safety concerns and side effects, as they require great attention to diet. MAOIs can trigger a life-
The tricyclic antidepressants, named as such because of their three-
Doctors relied heavily on monoamine oxidase inhibitors and tricyclics until newer, more popular pharmaceutical interventions were introduced in the 1980s. These selective serotonin reuptake inhibitors (SSRIs)—brands such as Prozac, Paxil, and Zoloft—
SSRIs are generally safer and have fewer negative effects than the older generation of antidepressants, which helps explain why they have become so popular in recent decades. But they are far from perfect. Weight gain, fatigue, hot flashes and chills, insomnia, nausea, and sexual dysfunction are all possible side effects. Some research suggests that they work no better than a placebo when it comes to treating mild to moderate depression (Fournier et al., 2010). But these drugs can be very beneficial in reducing the potentially devastating symptoms of depression. Improvement is generally noticed within 3–
CONNECTIONS
In Chapter 1, we stated that a placebo is a “pretend” treatment used to explore the effectiveness of a “true” treatment. The placebo effect is the tendency to feel better if we believe we are being treated with a medication. Expectations about getting better can change treatment outcomes.
mood-
MOOD-
Synonyms
mood-
traditional antipsychotic medications first-
atypical antipsychotics second-
Scientists have yet to determine the cause of bipolar disorder and how its symptoms might be lessened with lithium. But numerous theories exist, some pointing to imbalances in neurotransmitters such as glutamate and serotonin (Cho et al., 2005; Dixon & Hokin, 1998). Lithium also seems to be effective in lowering suicide risk among people with bipolar disorder (Angst, Angst, Gerber-
Anticonvulsant medications are also used to treat bipolar disorder. They were originally created to alleviate symptoms of seizure disorders, but scientists discovered they might also be used as mood stabilizers, and some research suggests that they can reduce the symptoms of mania (Bowden et al., 2000). Unfortunately, certain anticonvulsants may increase the risk of suicide or of possible suicide masked as violent death through injury or accident (Patorno et al., 2010). For this reason, the U.S. Food and Drug Administration (FDA, 2008) requires drug companies to place warnings on their labels.
antipsychotic drugs Psychotropic medication used in the treatment of psychotic symptoms, such as hallucinations and delusions.
ANTIPSYCHOTIC DRUGS The hallucinations and delusions of people with disorders like schizophrenia can be subdued with antipsychotics. Antipsychotic drugs are designed to block neurotransmitter receptors. Although it is not entirely clear how neurotransmitter activity causes the symptoms of schizophrenia, blocking these receptor sites reduces the firing of neurons presumably associated with psychotic symptoms.
CONNECTIONS
In Chapter 2, we described how drugs influence behavior by changing what is happening in the synapse. Agonists increase the normal activity of a neurotransmitter, and antagonists block normal neurotransmitter activity. Here we see how psychotropic medications alter activity in the synapse.
Two kinds of medications can be used in these cases: traditional antipsychotic medications and atypical antipsychotics (each with about a half-
First rolled out in the 1950s, traditional antipsychotics, such as Haldol, made it possible for scores of people to transition out of psychiatric institutions and into society. These new drugs reduced hallucinations and delusions for many patients, but doctors soon realized that they had other, not-
These problems were partially solved with the development of the atypical antipsychotics, such as Risperdal (risperidone), which reduce psychotic symptoms and usually do not cause tardive dyskinesia (Correll, Leucht, & Kane, 2004). But there are other potential side effects, such as weight gain, increased risk for Type 2 diabetes, sexual dysfunction, and heart disease (Ücok & Gaebel, 2008). And although these drugs reduce the symptoms in 60–
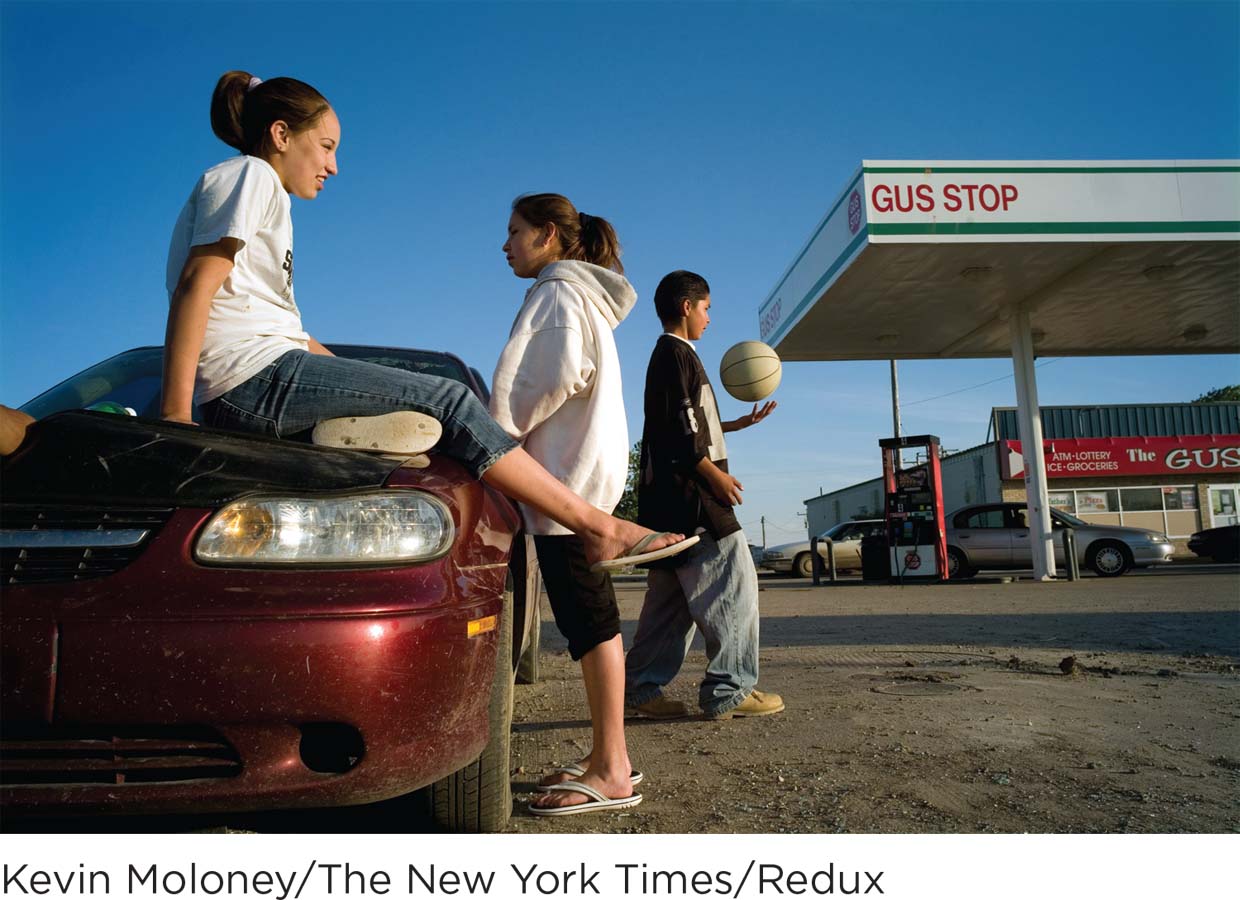
Teenagers Ariel Farmer (left), Kyla Sharp Butte, and Will Sharp Butte relax at a gas station on the Rosebud Indian Reservation. This photo appeared in a 2007 New York Times article about the shocking rates of suicide among reservation youth (Nieves, 2007, June 9). Suicides, homicides, and alcohol-
ANTIANXIETY DRUGS Anxiety disorders are the second most common class of conditions Dr. Foster encounters on the reservation. Like many impoverished areas, Rosebud has a high rate of trauma (for example, alcohol-
antianxiety drugs Psychotropic medications used for treating the symptoms of anxiety.
Antianxiety drugs are used to treat the symptoms of anxiety and anxiety disorders, including panic disorder, social phobia, and generalized anxiety disorder. Most of today’s antianxiety medications are benzodiazepines, such as Xanax and Ativan, also called “minor tranquilizers.” These drugs are used for a continuum of anxiety, from fear of flying to extreme panic attacks. And since they promote sleep in high doses, they can also be used to treat insomnia. Doctors often prescribe benzodiazepines in combination with other psychotropic medications.
CONNECTIONS
In Chapter 4, we discussed psychoactive drugs. Physiological dependence can occur with constant use of some drugs, indicated by tolerance and withdrawal symptoms. Psychological dependence is apparent when a strong desire or need to continue using a substance occurs, but without tolerance or withdrawal symptoms.
Valium is one of the most commonly used minor tranquilizers, and it was the first psychotropic drug to be used by people who were not necessarily suffering from serious disorders. For most of the 1970s, Valium was so popular among white collar businessmen and women that it came to be called “Executive Excedrin.” But then people began to realize how dependent they had become on Valium, both physically and psychologically, and its popularity diminished (Barber, 2008). Nevertheless, medications such as Valium and Xanax are still the most commonly abused antianxiety drugs (Phillips, 2013).
A key benefit of benzodiazepines is that they are fast-
PSYCHOTROPIC MEDICATION PLUS PSYCHOTHERAPY Psychotropic medications have helped countless people get back on their feet and enjoy life, but many believe that drugs alone don’t produce the best long-
Indeed, studies suggest that psychotropic drugs are most effective when used alongside psychotherapy. Researchers have shown that combining medication with an integrative approach to psychotherapy, including cognitive, behavioral, and psychodynamic perspectives, reduces major depressive symptoms faster than either approach alone (Manber et al., 2008).
Another key point to remember: Medications affect people in different ways. An antidepressant that works for one person may have no effect on another; this is also the case for side effects. We metabolize (break down) drugs at different rates, which means dosages must be assessed on a case-
When Drugs Aren’t Enough: The Other Biomedical Therapies
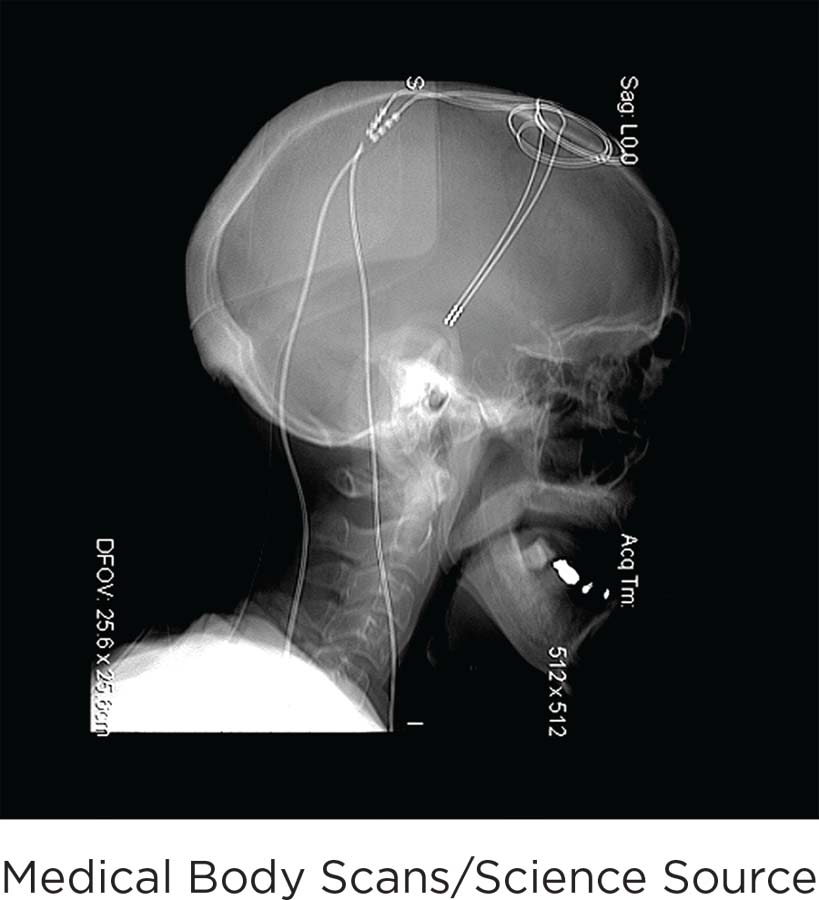
An X-
As you may already realize, psychotropic drugs are not a cure-
electroconvulsive therapy (ECT) A biomedical treatment of severe depression that induces seizures in the brain through electrical currents.
CONNECTIONS
In Chapter 6, we discussed amnesia, which is memory loss resulting from physical or psychological conditions. Retrograde amnesia is the inability to access old memories; anterograde amnesia is the inability to make new memories. ECT can cause these types of amnesia, which is one reason the American Psychiatric Association developed guidelines for its use (2001).
ELECTROCONVULSIVE THERAPY One biomedical approach that essentially causes seizures in the brain is electroconvulsive therapy (ECT), which is used with severely depressed people who have not responded to psychotropic medications or psychotherapy. If you’ve ever seen ECT, or “shock therapy,” portrayed in movies, you might think it’s a barbaric form of abuse. Truth be told, ECT was a brutal and overly used treatment in the mid-
Scientists don’t know exactly how ECT reduces the symptoms of depression, although a variety of theories have been proposed (Cyrzyk, 2013). And despite its enduring “bad rap,” ECT can be an effective treatment for depression, bipolar disorder, and schizophrenia in people who haven’t responded well to psychotherapy or drugs (Baker, 2009, January 8; Glass, 2001). Yet in the United States, the number of patients admitted to a hospital for ECT treatment in 2009 was 7.2 per 100,000 adults, which represented a substantial decline over the years (Case et al., 2013). The major downside of ECT is its tendency to induce confusion and memory loss, including anterograde and retrograde amnesias (American Psychiatric Association, 2001; Fink & Taylor, 2007; Read & Bentall, 2010).
Synonyms
neurosurgery psychosurgery, brain surgery
neurosurgery A biomedical therapy that involves the destruction of some portion of the brain or connections between different areas of the brain.
NEUROSURGERY One extreme option for patients who don’t show substantial improvement with psychotherapy or psychotropic drugs is neurosurgery, which destroys some portion of the brain or connections between different areas of the brain. Like ECT, neurosurgery is tarnished by an unethical past. During the 1930s, 1940s, and 1950s, doctors performed prefrontal lobotomies, destroying part of the frontal lobes or disconnecting them from lower areas of the brain (Kucharski, 1984). But lobotomies can lead to severe side effects, including permanent impairments to everyday functioning. In the past, this procedure had no precision, often resulting in personality changes and diminished function. The consequences of lobotomy were often worse than the disorders they aimed to fix. The popularity of this surgery plummeted in the 1950s when the first-
CONNECTIONS
In Chapter 2, we discussed the use of the split-
Brain surgeries are only used to treat psychological disorders as a last resort, and they are far more precise than the archaic lobotomy. Surgeons home in on a small target, destroying only tiny tracts of tissue. One of these surgeries has been a lifesaver for a select few suffering from a severe, drug-
TAKING STOCK: AN APPRAISAL OF BIOMEDICAL THERAPY Medications and other biomedical treatments can reduce the symptoms of major psychological disorders. In fact, psychotropic drugs work so well that their introduction led to the deinstitutionalization of thousands of people. But it would be a mistake to think of these biological interventions as a cure-
show what you know
Question 1
1. A young man is taking psychotropic medications for major depression, but the drugs do not seem to be alleviating his symptoms. Which of the following biomedical approaches might his psychiatrist try next?
split-
brain operation tardive dyskinesia
prefrontal lobotomy
electroconvulsive therapy
d. electroconvulsive therapy
Question 2
2. Psychotropic drugs can be divided into four categories, including mood-
mood normalizers.
antidepressants.
antagonists.
atypical antipsychotics.
b. antidepressants.
Question 3
3. How do biomedical interventions differ from psychotherapy? Compare their goals.
Answers will vary. Biomedical therapies use physical interventions to treat psychological disorders. These therapies can be categorized according to the method by which they influence the brain’s functioning: chemical, electrical, or structural. Psychotherapy is a treatment approach in which a client works with a mental health professional to reduce psychological symptoms and increase his or her quality of life. These approaches share common features: The relationship between the client and the treatment provider is of utmost importance, as is a sense of hope that things will get better. Psychotherapy generally seeks to reduce symptoms and increase the quality of life, whether a person is struggling with a psychological disorder or simply wants to be more fulfilled.