16.3 Fructose and Galactose Are Converted into Glycolytic Intermediates
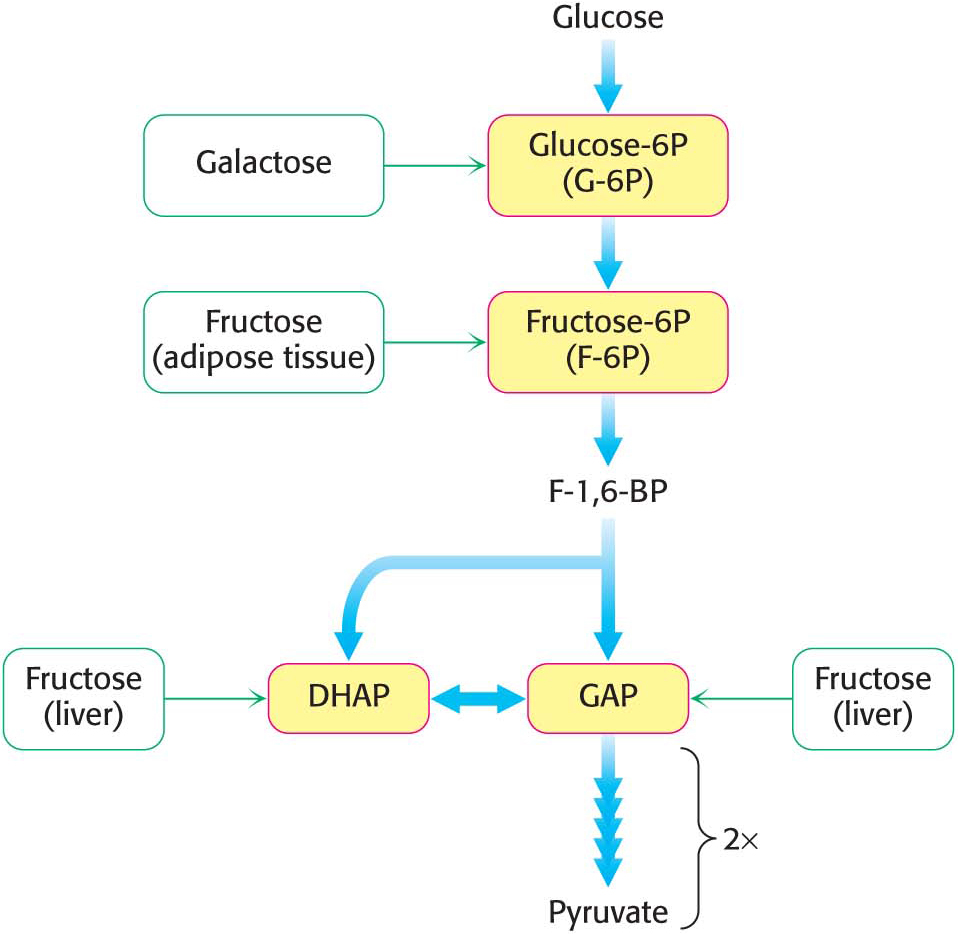
Although glucose is the monosaccharide most commonly used as an energy source, others also are important fuels. Let us consider how two common sugars—fructose and galactose—can be funneled into the glycolytic pathway (Figure 16.7). Fructose is a component of sucrose, or table sugar, as well as high-fructose corn syrup, which is used as a sweetener in many foods and drinks. Galactose is a component of lactose, or milk sugar. There are no catabolic pathways dedicated to metabolizing fructose or galactose as there is for glucose, and so the strategy is to convert these sugars into an intermediate in glycolysis.
Page 295
Fructose Is Converted into Glycolytic Intermediates by Fructokinase
Fructose can take one of two pathways to enter the glycolytic pathway. Much of the ingested fructose is metabolized by the liver, using the fructose 1-phosphate pathway(Figure 16.8). The first step is the phosphorylation of fructose to fructose 1-phosphate by fructokinase. Fructose 1-phosphate is then split into glyceraldehyde and dihydroxyacetone phosphate, an intermediate in glycolysis. This aldol cleavage is catalyzed by a specific fructose 1-phosphate aldolase. Dihydroxyacetone phosphate continues into stage 2 of glycolysis, whereas glyceraldehyde is then phosphorylated to glyceraldehyde 3-phosphate, a glycolytic intermediate, by triose kinase. In other tissues, such as adipose tissues, fructose can be phosphorylated to the glycolytic intermediate fructose 6-phosphate by hexokinase.
 CLINICAL INSIGHT
CLINICAL INSIGHTExcessive Fructose Consumption Can Lead to Pathological Conditions
Fructose is a common sweetener, as mentioned above. Epidemiological as well as clinical studies have linked excessive fructose consumption to obesity, fatty liver, and insulin insensitivity. These conditions may eventually result in type 2 diabetes (non-insulin-dependent diabetes). Studies have shown that these disorders are not necessarily the result of simple excess energy consumption. What aspects of fructose metabolism are the contributing factors then? Note that, as shown in Figure 16.8, the actions of fructokinase and triose kinase bypass the most important regulatory step in glycolysis, the phosphofructokinase-catalyzed reaction. The fructose-derived glyceraldehyde 3-phosphate and dihydroxyacetone phosphate are processed by glycolysis to pyruvate and subsequently to acetyl CoA in an unregulated fashion. As we will see in Chapter 28, this excess acetyl CoA is converted to fatty acids, which can be transported to adipose tissue, resulting in obesity. The liver also begins to accumulate fatty acids, resulting in fatty liver. The activity of the fructokinase and triose kinase can deplete the liver of ATP and inorganic phosphate, compromising liver function.
Page 296
Galactose Is Converted into Glucose 6-phosphate
Like fructose, galactose is an abundant sugar that must be converted into metabolites of glucose (Figure 16.7). Galactose is converted into glucose 6-phosphate in four steps. The first reaction in the galactose–glucose interconversion pathway is the phosphorylation of galactose to galactose 1-phosphate by galactokinase:
Galactose 1-phosphate then acquires a uridyl group from uridine diphosphate glucose (UDP-glucose), which activates the sugar phosphate so that it can be converted into glucose (Figure 16.9). UDP-monosaccharides are another example of an activated intermediate and are used as an intermediate in the synthesis of glycosidic linkages, the bonds between monosaccharides. The products of this reaction, which is catalyzed by galactose 1-phosphate uridyl transferase, are UDP-galactose and glucose 1-phosphate. The galactose moiety of UDP-galactose is then epimerized to glucose by UDP-galactose 4-epimerase. The epimerase inverts the hydroxyl group at carbon 4 to create glucose.
The sum of the reactions catalyzed by galactokinase, the transferase, and the epimerase is
Page 297
Note that UDP-glucose is not consumed in the conversion of galactose into glucose, because it is regenerated from UDP-galactose by the epimerase. This reaction is reversible, and the product of the reverse direction also is important. The conversion of UDP-glucose into UDP-galactose is essential for the synthesis of complex polysaccharides and glycoproteins (Chapter 10). Ordinarily, galactose fills this role, but, if the amount of galactose in the diet is inadequate to meet these needs, UDP-galactose is used.
Finally, glucose 1-phosphate, formed from galactose, is isomerized to glucose 6-phosphate by phosphoglucomutase:
We shall return to this reaction when we consider the synthesis and degradation of glycogen, which proceeds through glucose 1-phosphate, in Chapters 24 and 25.
 CLINICAL INSIGHT
CLINICAL INSIGHTMany Adults Are Intolerant of Milk Because They Are Deficient in Lactase
Many adults are unable to metabolize the milk sugar lactose and experience gastrointestinal disturbances if they drink milk. Lactose intolerance, or hypolactasia, is most commonly caused by a deficiency of the enzyme lactase, which cleaves lactose into glucose and galactose:
“Deficiency” is not quite the appropriate term, because a decrease in lactase is normal in the course of development in all mammals. As children are weaned and milk becomes less prominent in their diets, lactase activity normally declines to about 5 to 10% of the level at birth. This decrease is not as pronounced with some groups of people, most notably people of Northern European ancestry, who can continue to ingest milk without gastrointestinal difficulties (Figure 16.10). With the appearance of milk-producing domesticated animals, an adult with active lactase would hypothetically have had a selective advantage in being able to consume calories from the readily available milk. Because dairy farming originated only about 10,000 years ago, the evolutionary selective pressure on lactase persistence must have been substantial, attesting to the biochemical value of being able to use milk as an energy source into adulthood.
Page 298
What happens to the lactose in the intestine of a lactase-deficient person? The lactose is a good energy source for microorganisms in the colon, and they ferment it to lactic acid while also generating methane (CH4) and hydrogen gas (H2). The gas creates the uncomfortable feeling of gut distension and the annoying problem of flatulence. The lactate produced by the microorganisms draws water into the intestine, as does any undigested lactose, resulting in diarrhea. If severe enough, the gas and diarrhea hinder the absorption of other nutrients such as fats and proteins. The simplest treatment is to avoid the consumption of products containing much lactose. Alternatively, the enzyme lactase can be ingested with milk products.
 CLINICAL INSIGHT
CLINICAL INSIGHTGalactose Is Highly Toxic If the Transferase Is Missing
Less common than lactose intolerance are disorders that interfere with the metabolism of galactose. The disruption of galactose metabolism is referred to as galactosemia. The most common form, called classic galactosemia, is an inherited deficiency in galactose 1-phosphate uridyl transferase activity. Afflicted infants fail to thrive. They vomit or have diarrhea after consuming milk, and enlargement of the liver and jaundice are common, sometimes progressing to cirrhosis. Cataracts will form, and lethargy and retarded mental development also are common. The blood-galactose level is markedly elevated, and galactose is found in the urine. The absence of the transferase in red blood cells is a definitive diagnostic criterion.
The most common treatment is to remove galactose (and lactose) from the diet. An enigma of galactosemia is that, although elimination of galactose from the diet prevents liver disease and cataract development, most patients still suffer from central nervous system malfunction, most commonly a delayed acquisition of language skills. Female patients also display ovarian failure.
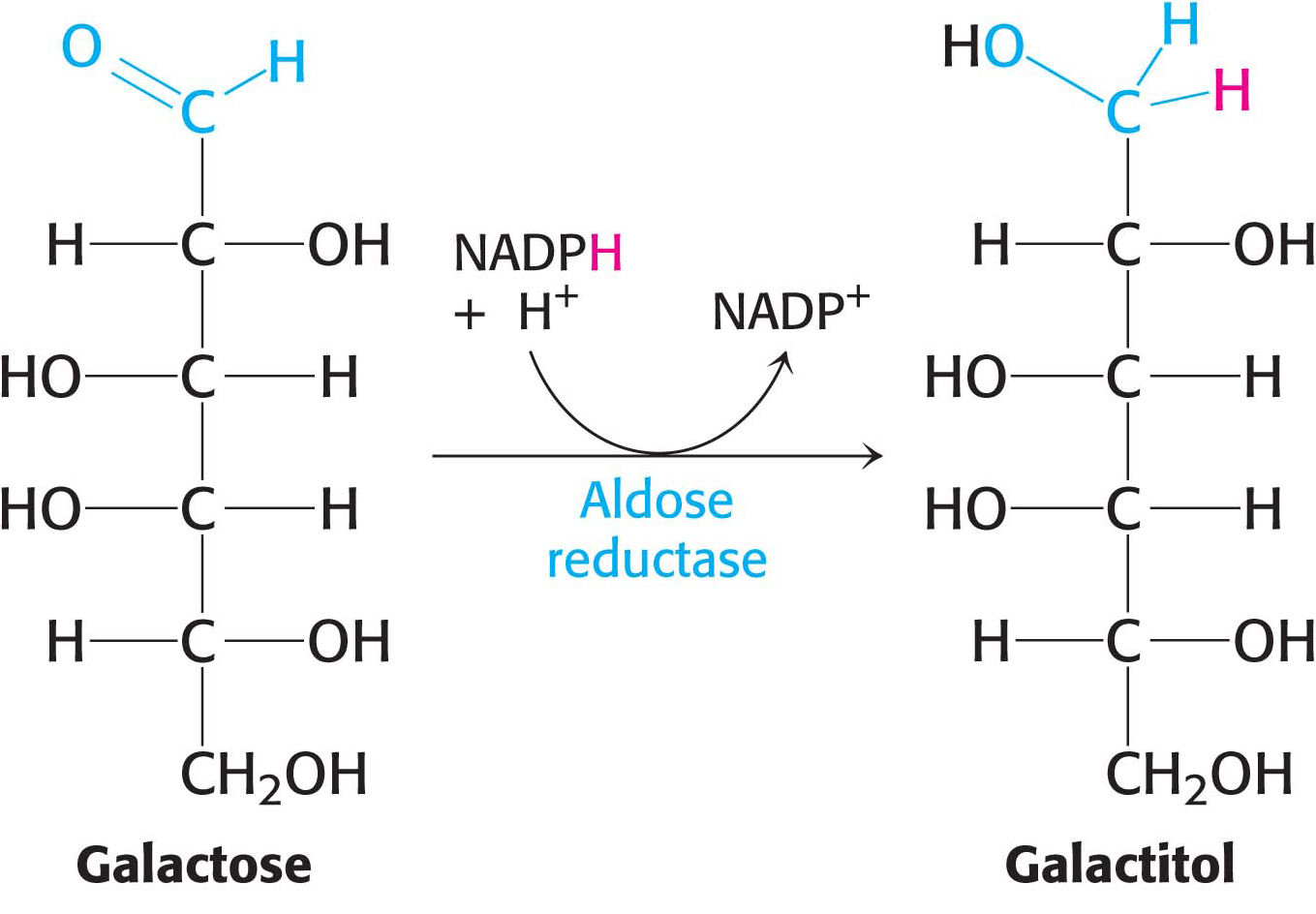
Cataract formation is better understood. A cataract is the clouding of the normally clear lens of the eye (Figure 16.11). If the transferase is not active in the lens of the eye, the presence of aldose reductase causes the accumulating galactose to be reduced to galactitol:
Galactitol is poorly metabolized and accumulates in the lens. Water will diffuse into the lens to maintain osmotic balance, instigating the formation of cataracts. In fact, even among those without galactosemia, there is a high incidence of cataract formation with age in populations that consume substantial amounts of milk into adulthood.
Page 299


 CLINICAL INSIGHT
CLINICAL INSIGHT



 CLINICAL INSIGHT
CLINICAL INSIGHT


 CLINICAL INSIGHT
CLINICAL INSIGHT