16.5 Metabolism in Context: Glycolysis Helps Pancreatic Beta Cells Sense Glucose
Insulin is a polypeptide hormone secreted by the ß cells of the pancreas in response to an increase in blood-glucose concentration, as would be the case after a meal. The function of insulin is to stimulate the uptake of glucose by tissues, notably muscle and adipose tissue. Although many of the details of how glucose stimulates insulin secretion remain to be elucidated, the general outline of the process is becoming clear.
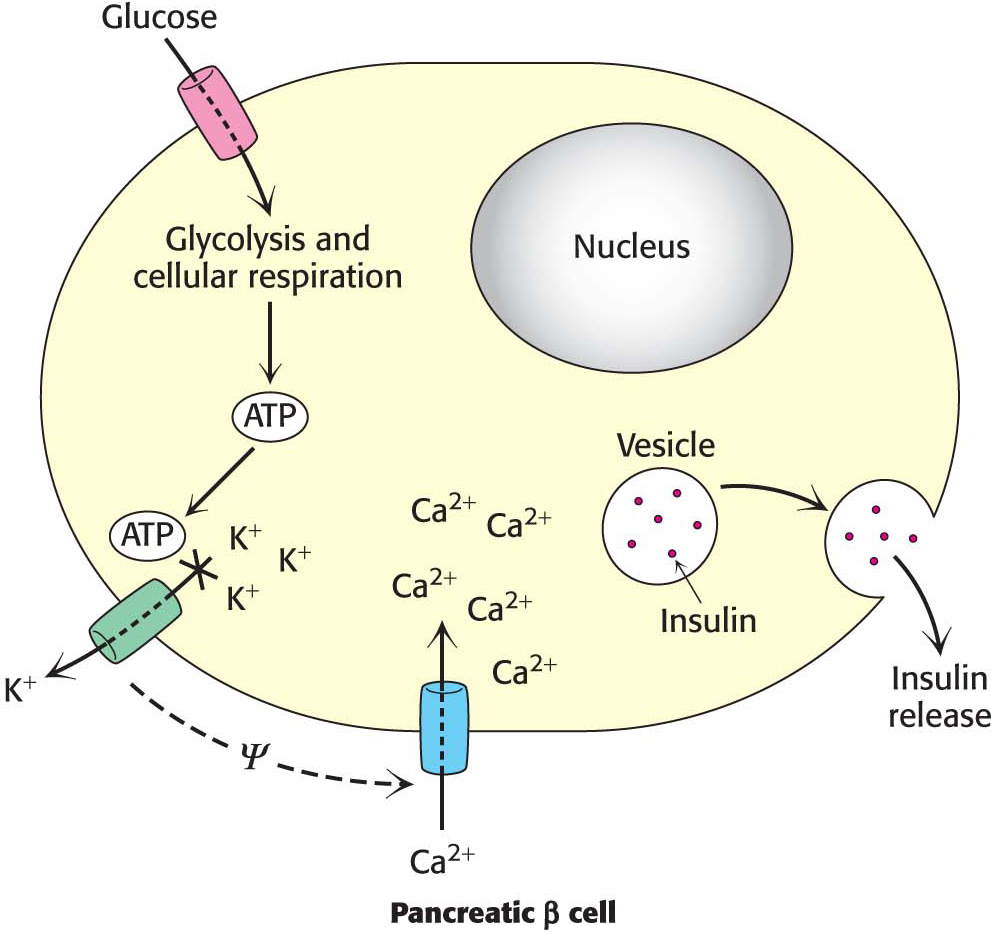
Glucose enters the ß cells of the pancreas through the glucose transporter GLUT2. As already discussed, GLUT2 will allow glucose entry only when blood glucose is plentiful. The ß cell metabolizes glucose glycolytically to pyruvate, which is subsequently processed by cellular respiration to CO2 and H2O (Sections 8 and 9). This metabolism generates ATP, as we have already seen for glycolysis (Figure 16.19). The resulting increase in the ATP/ADP ratio closes an ATP-sensitive K+ channel that, when open, allows potassium to flow out of the ß cell. The resulting alteration in the cellular ionic environment results in the opening of a Ca2+ channel. The influx of Ca2+ causes insulin-containing secretory vesicles to fuse with the cell membrane and release insulin into the blood. Thus, the increase in energy charge resulting from the metabolism of glucose has been translated by ion channels into a physiological response—the secretion of insulin and the subsequent removal of glucose from the blood.