E.2 Choices in Dying
Do you recoil at the heading “Choices in Dying”? If so, you may be living in the wrong century. Every twenty-
A Good Death
Especially For Relatives of a Person Who Is Dying Why would a healthy person want the attention of hospice caregivers?
Response for Relatives of a Person Who Is Dying: Death affects the entire family, including children and grandchildren. I learned this myself when my mother was dying. A hospice nurse not only gave her her pain medication (which made it easier for me to be with her) but also counseled me. At the nurse’s suggestion, I asked for forgiveness. My mother indicated that there was nothing to forgive. We both felt a peace that would have eluded us without hospice care.
People everywhere hope for a good death (Vogel, 2011), one that is:
- At the end of a long life
- Peaceful
- Quick
- In familiar surroundings
- With family and friends present Without pain, confusion, or discomfort
Many would add that control over circumstances and acceptance of the outcome are also characteristic of a good death, but cultures and individuals differ. Some dying individuals willingly cede control to doctors or caregivers, and others fight every sign that death is near.
Modern Medicine
In some ways, modern medicine makes a good death more likely. The first item on the list has become the norm: Death usually occurs at the end of a long life. Younger people still get sick, but surgery, drugs, radiation, and rehabilitation typically mean that, in developed countries, the ill go to the hospital and then return home. If young people die, death is typically quick (before medical intervention could save them), which, although it does not meet the criteria set out above, may actually be a painless death for them, if not for their loved ones.
In other ways, however, contemporary medical advances have made a bad death more likely. When a cure is impossible, physical and emotional comfort may deteriorate (Kastenbaum, 2012). Instead of acceptance, people fight death with surgery and drugs that prolong pain and confusion. Hospitals may exclude visitors at the most critical point, and patients may become delirious or unconscious, unable to die in peace.
The underlying problem may be medical care itself, which is so focused on life-
769
Honest Conversation
In about 1960, researcher Elisabeth Kübler-
From ongoing interviews, Kübler-
- Denial (“I am not really dying.”)
- Anger (“I blame my doctors, or my family, or God for my death.”)
- Bargaining (“I will be good from now on if I can live.”)
- Depression (“I don’t care about anything; nothing matters anymore.”)
- Acceptance (“I accept my death as part of life.”)
Another set of stages of dying is based on Abraham Maslow’s hierarchy of needs; as applied to the dying, Maslow’s hierarchy can be characterized as follows (Zalenski & Raspa, 2006):
- Physiological needs (freedom from pain)
- Safety (no abandonment)
- Love and acceptance (from close family and friends)
- Respect (from caregivers)
- Self-
actualization (appreciating one’s unique past and present)
[Lifespan Link: Maslow’s hierarchy of needs is discussed in Chapter 2.]
Maslow later suggested a possible sixth stage, self-
Other researchers have not found these sequential stages. Remember the woman dying of a sarcoma, cited earlier? She said that she would never accept death and that Kübler-
Nevertheless, both lists remind caregivers that each dying person has strong emotions and needs that may be unlike that same person’s emotions and needs a few days or weeks earlier. Furthermore, those emotions may differ from those of the caregivers, who themselves may each have their own emotions.
It is important for everyone—
Most dying people want to be with loved ones and to talk honestly with medical and religious professionals. Individual differences continue, of course. Some people do not want the whole truth, some want every possible medical intervention to occur, some do not want many visitors. In many Asian families, telling people they are dying is thought to destroy hope (Corr & Corr, 2013).
770
Better Ways to Die
Several practices have become more prevalent since the contrast between a good death and the usual hospital death has become clear. The hospice and the palliative-
Hospice
hospice An institution or program in which terminally ill patients receive palliative care to reduce suffering; family and friends of the dying are helped as well.
In 1950s London, Cecily Saunders opened the first modern hospice, where terminally ill people could spend their last days in comfort (Saunders, 1978). Thousands of other hospices have opened in many nations, and hundreds of thousands of hospice caregivers bring medication and care to dying people where they live. In the United States, half of all hospice deaths occur at home (National Center for Health Statistics, 2011).

Hospice professionals relieve discomfort, avoiding measures that merely delay death; their aim is to make dying easier. There are two principles for hospice care:
- Each patient’s autonomy and decisions are respected. For example, pain medication is readily available, not on a schedule or minimal dosage. Most hospice patients use less medication than a doctor might prescribe, but they decide.
- Family members and friends are counseled before the death, taught to provide care, and guided in mourning. Their needs are as important as those of the patient. Death is thought to happen to a family, not just to an individual.
Unfortunately, hospice does not reach many dying people (see Table EP.2), even in wealthy nations, much less in developing ones (Kiernan, 2010). Hospice care is more common in England than in mainland Europe, more common in the western part of the United States than the southeastern part, and rare in poor nations. Everywhere, those of higher SES are more likely to receive hospice care. In the U.S. there are ethnic differences as well. For example, when African Americans enter hospice, they are more often admitted from a hospital than a home and are likely to die relatively quickly (one week, on average) (K. S. Johnson et al., 2011).
Currently in the United States, 60 percent of people die without hospice; of the 40 percent in hospice, one-
| ■ | Hospice patients must be terminally ill, with death anticipated within six months, but predictions are difficult. For example, in one study of noncancer patients, physician predictions were 90 percent accurate for those who died within a week but only 13 percent accurate when death was predicted in three to six weeks (usually the patients died sooner) (Brandt et al., 2006). |
| ■ | Patients and caregivers must accept death. Traditionally, entering a hospice meant the end of curative treatment (chemotherapy, dialysis, and so on). This is no longer true. Now treatment can continue, and death is estimated to occur within six months without treatment. That means many hospice patients survive for longer than six months, and some get so much better that they are discharged (Salpeter et al., 2012). |
| ■ | Hospice care is costly. Skilled workers— |
| ■ | Availability varies. Hospice care is more common in England than in mainland Europe and is a luxury in poor nations. In the United States, western states have more hospices than southern states do. Even in one region (northern California) and among clients of one insurance company (Kaiser), the likelihood that people with terminal cancer will enter hospice depends on exactly where they live (N. L. Keating et al., 2006). |
771
Entering hospice means that comfort takes precedence over cure, but sometimes that itself extends life. In fact, 16 percent of U.S. hospice patients are discharged alive. Comfort can include measures that some hospitals forbid: acupuncture, special foods, flexible schedules, visitors when the patient wants them (which could be 2 A.M.), massage, aromatic oils, and so on (Doka, 2013).
Hospice care is expensive if it occurs in a separate institution where many skilled workers—
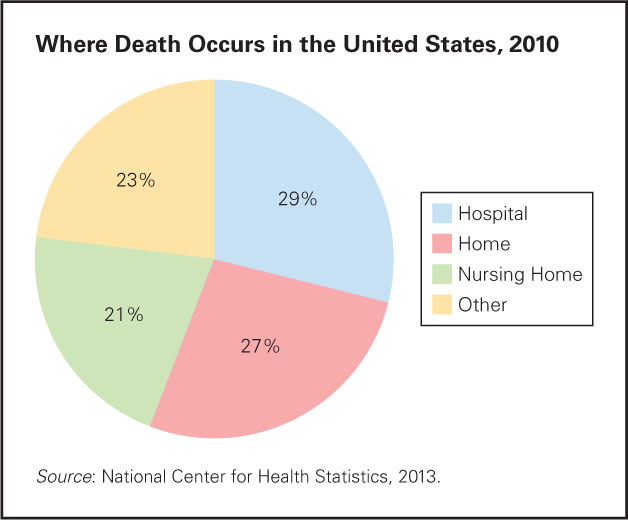
Home hospice care is less expensive, but it requires family or friends trained by hospice workers to provide care. Although this has led to an increase of “good deaths” at home, most deaths still occur in hospitals, and many others occur in nursing homes (see Figure EP.4).
Palliative Care
palliative care Care designed not to treat an illness but to provide physical and emotional comfort to the patient and support and guidance to his or her family.
In 2006 the American Medical Association approved a new specialty, palliative care, which focuses on relieving pain and suffering. Palliative-
double effect A situation in which an action (such as administering opiates) has both a positive effect (relieving a terminally ill person’s pain) and a negative effect (hastening death by suppressing respiration).
Morphine and other opiates have a double effect: They relieve pain (a positive effect), but they also slow down respiration (a negative effect). A painkiller that reduces both pain and breathing is allowed by law, ethics, and medical practice. In England, for instance, although it is illegal to cause death, even of a terminally ill patient who repeatedly asks to die, it is legal to prescribe drugs that have a double effect. One-
Heavy sedation is another method sometimes used to alleviate pain. Concerns have been raised that this sometimes merely delays death rather than prolonging meaningful life, since the patient becomes unconscious, unable to think or feel (Raus et al., 2011).
Ethical Issues
As you see, the success of medicine has created new dilemmas. Death is no longer the natural outcome of age and disease; when and how death occurs involves human choices.
772
Deciding When Death Occurs
No longer does death necessarily occur when a vital organ stops. Breathing continues with respirators, stopped hearts are restarted, stomach tubes provide calories, drugs fight pneumonia. At what point, if ever, should intervention stop to allow death?
Almost every life-
One physician, a specialist in palliative care, advised his colleagues:
The highway of aggressive medical treatment runs fast, is heavily travelled, but can lack landmarks and the signage necessary to know when it is time to make for the exit ramp…. These signs are there and it is your responsibility to communicate them to patients and families.
[Fins, 2006, p. 73]
Good advice, hard to follow.
Evidence of Death
Historically, death was determined by listening to a person’s chest: No heartbeat meant death. To make sure, a feather was put to the person’s nose to indicate respiration—
Many life-
| Brain death: Prolonged cessation of all brain activity with complete absence of voluntary movements; no spontaneous breathing; no response to pain, noise, and other stimuli. Brain waves have ceased; the electroencephalogram is flat; the person is dead. |
|
Locked- |
| Coma: A state of deep unconsciousness from which the person cannot be aroused. Some people awaken spontaneously from a coma; others enter a vegetative state; the person is not yet dead. |
| Vegetative state: A state of deep unconsciousness in which all cognitive functions are absent, although eyes may open, sounds may be emitted, and breathing may continue; the person is not yet dead. The vegetative state can be transient, persistent, or permanent. No one has ever recovered after two years; most who recover (about 15 percent) improve within three weeks (Preston & Kelly, 2006). After sufficient time has elapsed, the person may, effectively, be dead, although exactly how many days that requires has not yet been determined (Wijdicks et al., 2010). |
773
It is critical to know when people are in a permanent vegetative state (and thus will never regain the ability to think) and when they are merely in a coma but might recover. One crucial factor is whether the person could ever again breathe without a respirator, but that is hard to guarantee if “ever again” includes 10 or 20 years hence.
In 2008, the American Academy of Neurology gathered experts to conduct a meta-
As this article points out, everyone needs to know when a person is brain-
Euthanasia
passive euthanasia A situation in which a seriously ill person is allowed to die naturally, through the cessation of medical intervention.
DNR (do not resuscitate) order A written order from a physician (sometimes initiated by a patient’s advance directive or by a health care proxy’s request) that no attempt should be made to revive a patient if he or she suffers cardiac or respiratory arrest.
Euthanasia, common for pets but rare for people, is very controversial. Many people see a major distinction between active and passive euthanasia (sometimes called mercy killing), although the final result is the same. In passive euthanasia, a person near death is allowed to die. They may have a DNR (do not resuscitate) order, instructing medical staff not to restore breathing or restart the heart if breathing or pulsating stops.
Passive euthanasia is legal everywhere if the dying person chooses it, but many emergency personnel start artificial respiration and stimulate hearts without asking whether a patient has a DNR. That might make passive euthanasia impossible.
active euthanasia A situation in which someone takes action to bring about another person’s death, with the intention of ending that person’s suffering.
Active euthanasia is deliberately doing something to cause death, such as turning off a respirator or giving a lethal drug. Some physicians condone active euthanasia when three conditions occur: (1) suffering that cannot be relieved, (2) incurable illness and (3) a patient who wants to die. Active euthanasia is legal in the Netherlands, Belgium, Luxembourg, and Switzerland, and illegal (but rarely prosecuted) elsewhere.
Attitudes may be changing. For example, over the past decade in Austria doctors in training have increasingly valued patients’ autonomy, which has led to more acceptance of active euthanasia (Stronegger et al., 2011) (see Figure EP.5).
In every nation surveyed, some physicians would never perform active euthanasia, but others have done so. Opinions from the public vary as well, although generally nations in eastern Europe are less accepting than those in western Europe (Cohen et al., 2013).

The Doctor’s Role
physician-
Between passive and active euthanasia is another option: A doctor may provide the means for patients to end their own lives in what is sometimes called physician-
Observation Quiz Where did this rally take place?
Answer to Observation Quiz: Paris, France. Two clues: That is the Eiffel tower in the background, and François Hollande was elected President of France in 2012.
774

For example, some cultures believe that suicide may be noble: Buddhist monks publicly burned themselves to death to advocate Tibetan independence from China; everywhere, some people choose to die for the honor of their nation or themselves. However, in the United States physicians of Asian religions are less likely to condone physician-
Pain: Physical and Psychological
The Netherlands has permitted active euthanasia and physician-
However, a qualitative analysis found that “fatigue, pain, decline, negative feelings, loss of self, fear of future suffering, dependency, loss of autonomy, being worn out, being a burden, loneliness, loss of all that makes life worth living, hopelessness, pointlessness and being tired of living were constituent elements of unbearable suffering” (Dees et al., 2011, p. 727). Obviously, medication cannot alleviate those states of mind.
| Percent of Patients Giving Reason (most had several reasons) | |
| Loss of autonomy | 91.2 |
| Less able to enjoy life | 88.8 |
| Loss of dignity | 82.0 |
| Loss of control over body | 51.6 |
| Burden on others | 38.6 |
| Pain | 23.5 |
| Financial implications of treatment | 2.7 |
| Source: Oregon Public Health Division, 2013. | |
Oregon voters approved physician-
- The dying person must be an Oregon resident, over age 17.
- The dying person must request the lethal drugs twice orally and once in writing.
- Fifteen days must elapse between the first request and the prescription.
- Two physicians must confirm that the person is terminally ill, has less than six months to live, and is competent (i.e., not mentally impaired or depressed).
The law also requires record-
As Table EP.4 shows, Oregon residents requested the drugs primarily for psychological, not biological, reasons—
775
OPPOSING PERSPECTIVES
The “Right to Die”?
slippery slope The argument that a given action will start a chain of events that will culminate in an undesirable outcome.
Many people fear that legalizing euthanasia or physician-
In Oregon and the Netherlands, the oldest-
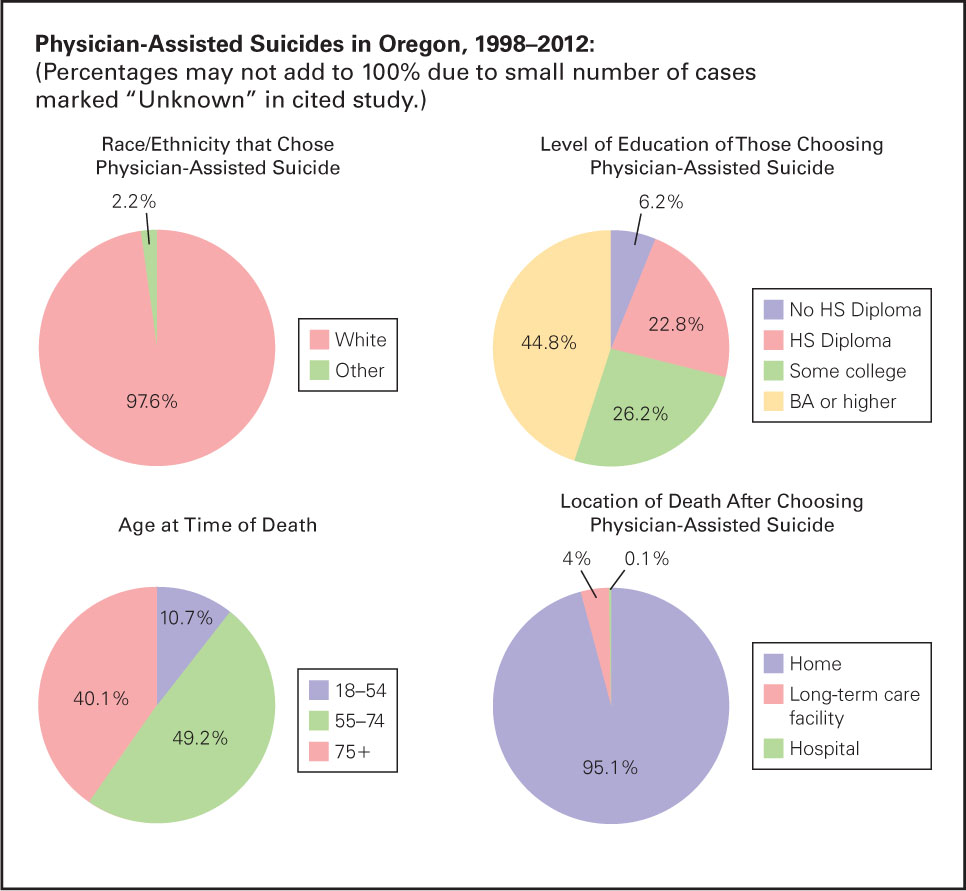
All these statistics refute both the slippery-
The 1980 Netherlands law was revised in 2002 to allow euthanasia not only when a person is terminally ill but also when a person is chronically ill and in pain. The number of Dutch people who choose euthanasia is increasing; it accounted for about 1 in 30 deaths in 2012. Is this a slippery slope? Some people think so, especially those who believe that God alone decides the moment of death and that anyone who interferes is defying God.
Arguing against that perspective, a cancer specialist writes:
To be forced to continue living a life that one deems intolerable when there are doctors who are willing either to end one’s life or to assist one in ending one’s own life, is an unspeakable violation of an individual’s freedom to live—
[Benatar, 2011, p. 206]
Yet not everyone agrees with that cancer specialist. Might the decision to die itself be evidence of depression that should prohibit physicians from prescribing lethal drugs (Finlay & George, 2011)? Declining ability to enjoy life was cited by 89 percent of Oregonians who requested physician-
Acceptance of death signifies mental health in the aged but not necessarily in the young: Should death with dignity be allowed only after age 54? That would have excluded 11 percent of Oregonians who have used the act thus far. Is the idea that only the old should be allowed to choose death an ageist idea, perhaps assuming that the young don’t understand what they are choosing, or that the old are the ones for whom life is over?
The number of people who die by taking advantage of Oregon’s law has increased steadily, from 16 in 1998 (the first year) to 77 in 2012. Some might see that as evidence of a slippery slope. Others consider it proof that the practice is useful though rare—
People with disabling, painful, and terminal conditions who die after choosing futile measures to prolong life are eulogized as “fighters” who “never gave up.” That indicates social approval of such choices. This same attitude about life and death is held by most voters and lawmakers around the world. The majority opposes laws that allow physician-
However, that majority is not evident everywhere. In the state of Washington, just north of Oregon, 58 percent of the voters approved a Death with Dignity law in November 2008; in 2009, Luxembourg joined the Netherlands and Belgium in allowing active euthanasia; in 2011, the Montana senate refused to forbid physician-
All that might seem like a growing trend, but proposals to legalize physician-
776
Advance Directives
advance directives Any description of what people want to happen as they die and after they die. This can include medical measures, choosing whom to allow as visitors, funeral arrangements, cremation, and so on.
Advance directives can describe everything regarding end-
Many people want personal choice about death, and thus approve advance directives in theory, but are uncertain about specifics. For example, few know that restarting the heart may extend life for decades in a young, healthy adult but may result in dementia, or merely prolong dying, in an elderly person whose health is failing.
Added to the complications are personal specifics, such as other morbidities, timing, mobility. For example, sometimes cardio resuscitation is harmful, partly based on how long the heart has stopped (Buss, 2013). Data on overall averages is contradictory (Elliot et al., 2011). Furthermore, data on outcome is usually for survivors, not for those who die after various interventions, so advance directives may be based on faulty assumptions.
Even talking about choices is controversial. Originally, the U.S. health care bill passed in 2010 allowed doctors to be paid for describing treatment options (e.g., Kettl, 2010). Opponents called those “death panels,” an accusation that almost torpedoed the entire package. As a result, that measure was scrapped: Physicians cannot bill for time spent explaining palliative care, options for treatment, or dying.
777
Wills and Proxies
Advance directives often include a living will and/or a health care proxy. Hospitals and hospices strongly recommend both of these. Nonetheless, most people resist: A study of cancer patients in a leading hospital found that only 16 percent had living wills and only 48 percent had designated a proxy (Halpern et al., 2011).
living will A document that indicates what medical intervention an individual prefers if he or she is not conscious when a decision is to be made. For example, some do not want to be given mechanical breathing.
A living will indicates what sort of medical intervention a person wants or does not want in the event that he or she becomes unable to express his or her preferences. (If the person is conscious, hospital personnel ask about each specific procedure, often requiring written consent before surgery. Patients who are conscious and lucid can choose to override any instructions they wrote earlier in their living will.)
The reason that people might want to override their own earlier wishes is that living wills include phrases such as “incurable,” “reasonable chance of recovery,” and “extraordinary measures,” and it is difficult to know what those phrases mean until a specific issue arises. Even then, medical judgments vary. Doctors and family members also disagree about what is “extraordinary” or “reasonable.”
health care proxy A person chosen by another person to make medical decisions if the second person becomes unable to do so.
Some people designate a health care proxy—another person to make medical decisions for them if they become unable to do so. That seems logical, but unfortunately neither a living will nor a health care proxy guarantees that medical care will be exactly what a person would choose. For one thing, proxies often find it difficult to allow a loved one to die. A larger problem is that few people—
Especially for People Without Advance Directives Why do very few young adults have advance directives?
Response for People Without Advance Directives: Young adults tend to avoid thinking realistically about their own deaths. This attitude is emotional, not rational. The actual task of preparing the documents is easy (the forms can be downloaded; no lawyer is needed). Young adults have no trouble doing other future-
Medical professionals advocate advance directives, but they also acknowledge there are problems with them. As one couple wrote:
Working within the reality of mortality, coming to death is then an inevitable part of life, an event to be lived rather than a problem to be solved. Ideally, we would live the end of our life from the same values that have given meaning to the story of our life up to that time. But in a medical crisis, there is little time, language, or ritual to guide patients and their families in conceptualizing or expressing their values and goals.
[Farber & Farber, 2014, p. 109]
The Schiavo Case
A heartbreaking example of the need for a health care proxy occurred with Theresa (Terri) Schiavo, who was 26 years old when her heart suddenly stopped. Emergency personnel restarted her heart, but she fell into a deep coma. Like almost everyone her age, Terri had no advance directives. A court designated Michael, her husband of six years, as her proxy.
Michael attempted many measures to bring back his wife, but after 11 years he accepted her doctors’ repeated diagnosis: Terri was in a persistent vegetative state. He petitioned to have her feeding tube removed. The court agreed, noting the testimony of witnesses who said that Terri had told them that she never wanted to be on life support. Terri’s parents appealed the decision but lost. They then pleaded with the public.

The Florida legislature responded, passing a law that required that the tube be reinserted. After three more years of legal wrangling, the U.S. Supreme Court ruled that the lower courts were correct. By this point, every North American newspaper and TV station was following the case. Congress passed a law requiring that artificial feeding be continued, but that law, too, was overturned as unconstitutional.
778
The stomach tube was removed, and Terri died on March 31, 2005—
Partly because of the conflicts among family members, and between appointed judges and elected politicians, Terri’s case caught media attention, inspiring vigils and protests. Lost in that blitz are the thousands of other mothers and fathers, husbands and wives, sons and daughters, judges and legislators, doctors and nurses who struggle less publicly with similar issues.
Advance directives may help make death “an event to be lived…[with] the same values that have given meaning to the story of our life” (Farber & Farber, 2014, p.109) and provide caregivers some peace. But, as the Schiavo case makes clear, discussion with every family member is needed long before a crisis occurs (Rogne & McCune, 2014).
SUMMING UP
Modern medicine has made some aspects of a good death more likely but has also added complexities. People can be kept alive long after their brains fail, via respirators, feeding tubes, and so on. Honest conversation, hospice care, and palliative medicine have made dying easier than when almost everyone died alone, in hospitals. However, passive and active euthanasia and assisted suicide are controversial. Part of the problem is that it is not always obvious when a dying person cannot recover, or even when death has occurred.
Various advance directives, including living wills and health care proxies in combination with honest conversation, can prevent some family conflicts and help people die as they wish and have their wishes for what happens after death honored. However, others often disagree about what a patient would want, and medical ethics, laws, and religious practices do not always provide guidance.