10.1 Factitious Disorder
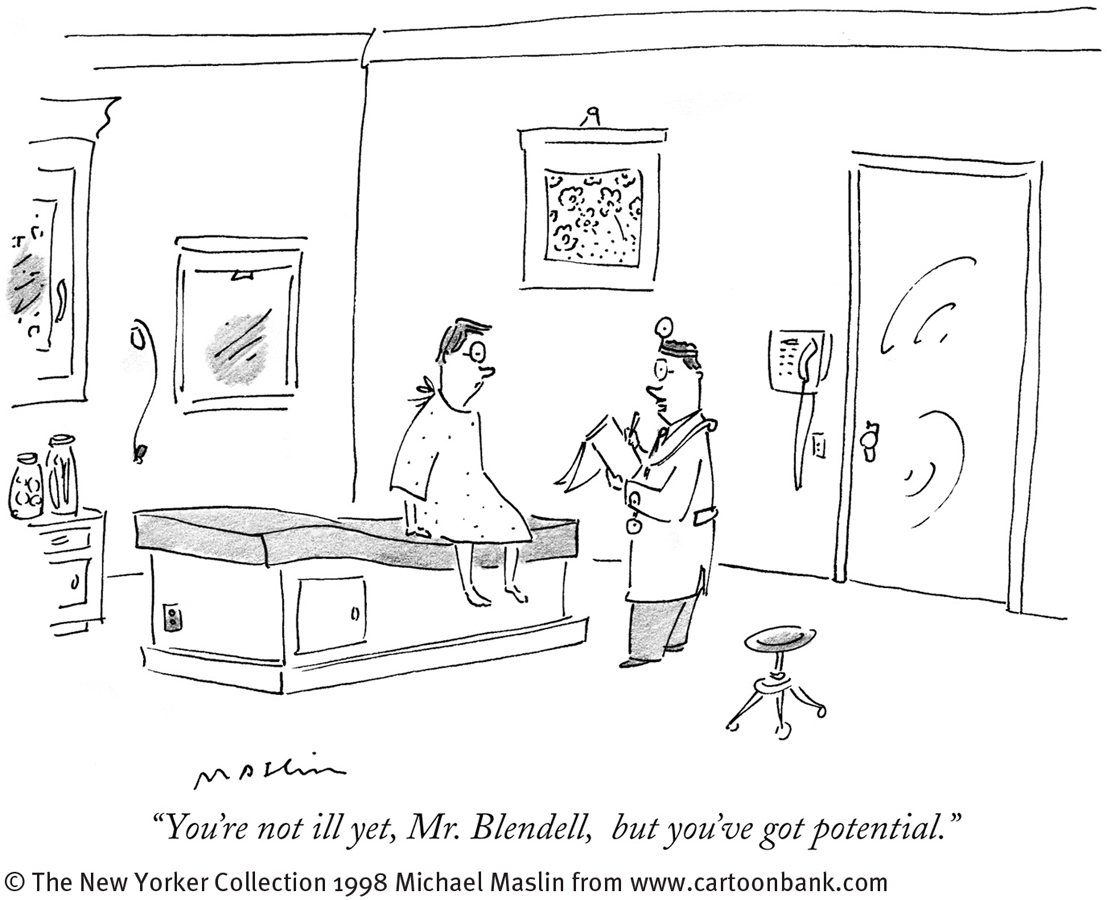
Like Jarell, people who become physically sick usually go to a physician. Sometimes, however, the physician cannot find a medical cause for the problem and may suspect that other factors are involved. Perhaps the patient is malingering—intentionally feigning illness to achieve some external gain, such as financial compensation or deferment from military service (Crighton et al., 2014).
Alternatively, a patient may intentionally produce or feign physical symptoms from a wish to be a patient; that is, the motivation for assuming the sick role may be the role itself (Lela et al., 2013). Physicians would then decide that the patient is manifesting factitious disorder (see Table 10-1). Consider, for example, the symptoms of this lab technician:
 factitious disorder A disorder in which a person feigns or induces physical symptoms, typically for the purpose of assuming the role of a sick person.
factitious disorder A disorder in which a person feigns or induces physical symptoms, typically for the purpose of assuming the role of a sick person.
A 29-
(Spitzer et al., 1981, p. 33)
|
Factitious Disorder Imposed on Self |
|
|---|---|
|
1. |
False creation of physical or psychological symptoms, or deceptive production of injury or disease, even without external rewards for such ailments. |
|
2. |
Presentation of oneself as ill, damaged, or hurt. |
|
Factitious Disorder Imposed on Another |
|
|
1. |
False creation of physical or psychological symptoms, or deceptive production of injury or disease, in another person, even without external rewards for such ailments. |
|
2. |
Presentation of another person (victim) as ill, damaged, or hurt. |
|
(Information from: APA, 2013) |
|
Factitious disorder is known popularly as Munchausen syndrome, a label derived from the exploits of Baron von Münchhausen, an eighteenth-
319
BETWEEN THE LINES
New Pop-
Phantom cell phone vibration syndrome: A false sense that one’s cell phone is vibrating (Archer, 2013)
People with factitious disorder often research their supposed ailments and are impressively knowledgeable about medicine (Miner & Feldman, 1998). Many eagerly undergo painful testing or treatment, even surgery (McDermott et al., 2012). When confronted with evidence that their symptoms are factitious, they typically deny the charges and leave the hospital; they may enter another hospital the same day. Clinical researchers have had a hard time determining the prevalence of factitious disorder, since patients with the disorder hide the true nature of their problem (Kenedi, Sames, & Paice, 2013). Overall, the pattern appears to be more common in women than men. Men, however, may more often have severe cases. The disorder usually begins during early adulthood.
Factitious disorder seems to be particularly common among people who (1) received extensive treatment for a medical problem as children, (2) carry a grudge against the medical profession, or (3) have worked as a nurse, laboratory technician, or medical aide. A number have poor social support, few enduring social relationships, and little family life (McDermott et al., 2012; Feldman et al., 1994).
The precise causes of factitious disorder are not understood (Lawlor & Kirakowski, 2014), although clinical reports have pointed to factors such as depression, unsupportive parental relationships during childhood, and an extreme need for social support that is not otherwise available (McDermott et al., 2012; Ozden & Canat, 1999; Feldman et al., 1994). Nor have clinicians been able to develop dependably effective treatments for this disorder (McDermott et al., 2012; Feldman & Feldman, 1995).
Psychotherapists and medical practitioners often report feelings of annoyance or anger toward people with factitious disorder, feeling that these people are, at the very least, wasting their time. Yet people with the disorder feel they have no control over the problem, and they often experience great distress.
320
Should society treat or punish those parents who produce Munchausen syndrome by proxy in their children?
In a related pattern, factitious disorder imposed on another, known popularly as Munchausen syndrome by proxy, parents or caretakers make up or produce physical illnesses in their children, leading in some cases to repeated painful diagnostic tests, medication, and surgery (Flaherty & Macmillan, 2013; Ayoub, 2010). If the children are removed from their parents and placed in the care of others, their symptoms disappear (see PsychWatch below).
PsychWatch
Munchausen Syndrome by Proxy
Tanya, a mere 8 years old, had been hospitalized 127 times over the past five years and undergone 28 different medical procedures—
“I miss Mommy so much. She’s the best person in the world. She spent all her time with me in the hospital. She’s the one who always took care of me. She always fed me through the tube. She made the doctors pay attention to me. She’s the reason I knew I could get better. Mommy even put up the Facebook page, and that’s why I got all those messages from everyone. People who didn’t even know me told me that they’re praying for me.
“It’s not fair. She’s gone, and they won’t let me see her. I just don’t understand. Daddy doesn’t like her anymore. They say Mommy was making me feel bad, putting bad stuff in my tube. I heard Daddy saying that’s why I feel better now with Mommy away. But I know there’s no way Mommy made me feel that bad. She’d have to hate me, but she loves me. Now that the Facebook page is gone I need her more than ever. Everyone else forgot about me.”
Cases like Tanya’s have horrified the public and called attention to Munchausen syndrome by proxy. This form of factitious disorder is caused by a caregiver who uses various techniques to induce symptoms in a child—

Between 6 and 30 percent of the victims of Munchausen syndrome by proxy die as a result of their symptoms, and 8 percent of those who survive are permanently disfigured or physically impaired (Flaherty & Macmillan, 2013; Ayoub, 2006; Mitchell, 2001). Psychological, educational, and physical development are also affected (Schreier et al., 2010).
The syndrome is very hard to diagnose and may be more common than clinicians once thought (Ashraf & Thevasagayam, 2014; Scheuerman et al., 2013; Feldman, 2004). The parent (usually the mother) seems to be so devoted and caring that others sympathize with and admire her. Yet the physical problems disappear when the child and parent are separated (Scheuerman et al., 2013). In many cases, siblings of the sick child are also victimized (Ayoub, 2010, 2006).
What kind of parent carefully inflicts pain and illness on her own child? The typical Munchausen mother is emotionally needy: she craves the attention and praise she receives for her devoted care of her sick child (Asraf & Thevasagayam, 2014; Ayoub, 2010; Noeker, 2004). She may have little social support outside the medical system. Often the mothers have a medical background of some kind—
Law enforcement authorities approach Munchausen syndrome by proxy as a crime—
321