12.7 PUTTING IT...together
New Wrinkles to a Familiar Story
In some respects, the story of the misuse of drugs is the same today as in the past. Substance use is still rampant, often creating damaging psychological disorders. New drugs keep emerging, and the public goes through periods of believing, naïvely, that the new drugs are “safe.” Only gradually do people learn that these, too, pose dangers. And treatments for substance-
421
Yet there are positive new wrinkles in this familiar story. Researchers have begun to develop a clearer understanding of how drugs act on the brain and body. In treatment, self-
Perhaps the most important insight to be gained from these integrated efforts is that several of the models were already on the right track. Social pressures, personality characteristics, rewards, and genetic predispositions all seem to play roles in substance use disorders, and in fact to operate together. For example, some people may inherit a malfunction of the biological reward center and so may need special doses of external stimulation—
Just as each model has identified important factors in the development of substance use disorders, each has made important contributions to treatment. As you have seen, the various forms of treatment seem to work best when they are combined with approaches from the other models, making integrated treatment the most productive approach.
Yet another new wrinkle to the addiction story is that the clinical field has now formally proclaimed that substances are not the only things to which people may develop an addiction. By grouping gambling disorder with the substance use disorders and targeting Internet gaming disorder for possible inclusion in the future, DSM-
CLINICAL CHOICES
Now that you’ve read about substance use and addictive disorders, try the interactive case study for this chapter. See if you are able to identify Jorge’s symptoms and suggest a diagnosis based on his symptoms. What kind of treatment would be most effective for Jorge? Go to LaunchPad to access Clinical Choices.
DSM-5 CONTROVERSY
Is All Drug Misuse the Same?
DSM-
SUMMING UP
SUBSTANCE MISUSE The misuse of substances (or drugs) may lead to temporary changes in behavior, emotions, or thoughts; this cluster changes is called intoxication. Chronic and excessive use can lead to substance use disorders. Many people with such disorders also develop a tolerance for the substance in question and/or have unpleasant withdrawal symptoms when they abstain from it. pp. 382–
383 DEPRESSANTS Depressants are substances that slow the activity of the central nervous system. Chronic and excessive use of these substances can lead to problems such as alcohol use disorder, sedative-
hypnotic use disorder, or opioid use disorder. 422
Alcoholic beverages contain ethyl alcohol, which is carried by the blood to the central nervous system, depressing its function. Intoxication occurs when the concentration of alcohol in the bloodstream reaches 0.09 percent. Among other actions, alcohol increases the activity of the neurotransmitter GABA at key sites in the brain. The sedative-
hypnotic drugs, which produce feelings of relaxation and drowsiness, include barbiturates and benzodiazepines. These drugs also increase the activity of GABA. Opioids include opium and drugs derived from it, such as morphine and heroin, as well as laboratory- made opioids. They all reduce tension and pain and cause other reactions. Opioids operate by binding to neurons that ordinarily receive endorphins. pp. 383– 392 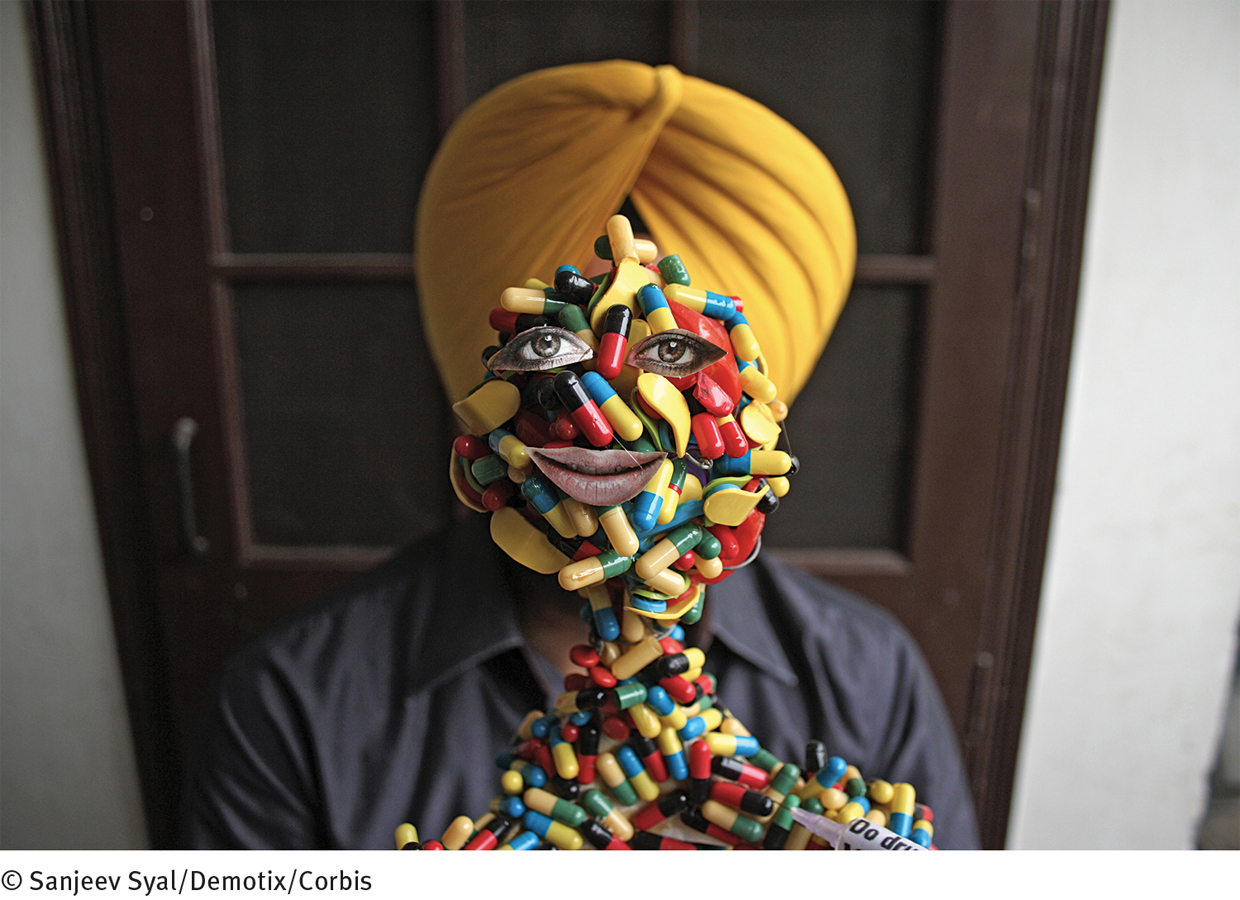 Spreading the word Community drug-
Spreading the word Community drug-prevention programs help increase public awareness about the nature, signs, and dangers of drug abuse. In a particularly innovative effort of this kind, Harwinder Singh Gill, an artist in India, created a model of the human body made up of capsule shells. Gill did this on the eve of the 2012 International Day Against Drug Abuse and Illicit Trafficking. STIMULANTS Stimulants, including cocaine, amphetamines, caffeine, and nicotine, are substances that increase the activity of the central nervous system. Abnormal use of cocaine or amphetamines can lead to stimulant use disorder. Stimulants produce their effects by increasing the activity of dopamine, norepinephrine, and serotonin in the brain. pp. 392–
398 HALLUCINOGENS Hallucinogens, such as LSD, are substances that cause powerful changes primarily in sensory perception. People’s perceptions are intensified and they may have illusions and hallucinations. LSD apparently causes such effects by disturbing the release of the neurotransmitter serotonin. pp. 398–
400 CANNABIS The main ingredient of Cannabis sativa, a hemp plant, is tetra-
hydrocannabinol (THC). Marijuana, the most popular form of cannabis, is more powerful today than it was in years past. It can cause intoxication, and regular use can lead to cannabis use disorder. pp. 401– 404 COMBINATIONS OF SUBSTANCES Many people take more than one drug at a time, and the drugs interact. The use of two or more drugs at the same time—
polysubstance use—has become increasingly common. pp. 404– 405 EXPLANATIONS FOR SUBSTANCE USE DISORDERS Several explanations for substance use disorders have been put forward. Together they are beginning to shed light on the disorders. According to sociocultural theorists, the people most likely to develop these disorders are those living in socioeconomic conditions that generate stress or whose families value or tolerate drug use. In the psychodynamic view, people who develop substance use disorders have excessive dependency needs traceable to the early stages of life. Some psychodynamic theorists also believe that certain people have a substance abuse personality that makes them prone to drug use. In the leading behavioral view, drug use is seen as being reinforced initially because it reduces tensions and raises spirits. According to cognitive theorists, such reductions may also lead to an expectancy that drugs will be comforting and helpful.
The biological explanations are supported by twin, adoptee, genetic linkage, and molecular biology studies, suggesting that people may inherit a predisposition to the disorders. Researchers have also learned that drug tolerance and withdrawal symptoms may be caused by cutbacks in the brain’s production of particular neurotransmitters during excessive and chronic drug use. Biological studies suggest that many, perhaps all, drugs may ultimately lead to increased dopamine activity in the brain’s reward center. pp. 405–
4100 TREATMENTS FOR SUBSTANCE USE DISORDERS Treatments for substance use disorders vary widely. Usually several approaches are combined. Psychodynamic therapies are used to try to help clients become aware of and correct the underlying needs and conflicts that may have led to their use of drugs. A common behavioral technique is aversion therapy, in which an unpleasant stimulus is paired with the drug that the person is abusing. Cognitive and behavioral techniques have been combined in such forms as relapse-
prevention training. Biological treatments include detoxification, antagonist drugs, and drug maintenance therapy. Sociocultural treatments approach substance use disorders in a social context by means of self- help groups (e.g., Alcoholics Anonymous), culture- and gender- sensitive treatments, and community prevention programs. pp. 410– 419 423
OTHER ADDICTIVE DISORDERS DSM-
5 groups gambling disorder along- side the substance use disorders as an addictive disorder. The explanations for this disorder, which are parallel to those for substance use disorders, include genetic factors, dopamine activity, personality styles, and cognitive factors. Treatments for gambling disorder include cognitive- behavioral approaches, narcotic antagonists, and self- help groups. The DSM- 5 task force recommended that another addictive pattern, Internet gaming disorder, receive further study for possible inclusion in future DSM revisions. pp. 419– 420
Visit LaunchPad

www.macmillanhighered.com/