16.2 What Ethical Principles Guide Mental Health Professionals?
Discussions of the legal and mental health systems may sometimes give the impression that clinicians as a group are uncaring and are considerate of patients’ rights and needs only when they are forced to be. This, of course, is not true. Most clinicians care greatly about their clients and strive to help them while at the same time respecting their rights and dignity (Pope & Vasquez, 2016, 2011). In fact, clinicians do not rely exclusively on the legislative and court systems to ensure proper clinical practice. They also regulate themselves by continually developing and revising ethical guidelines for their work and behavior. Many legal decisions do nothing more than place the power of the law behind these already existing professional guidelines.
code of ethics A body of principles and rules for ethical behavior, designed to guide decisions and actions by members of a profession.
Each profession within the mental health field has its own code of ethics. The code of the American Psychological Association (2014, 2010, 2002) is typical. This code, highly respected by other mental health professionals and public officials, includes specific guidelines:
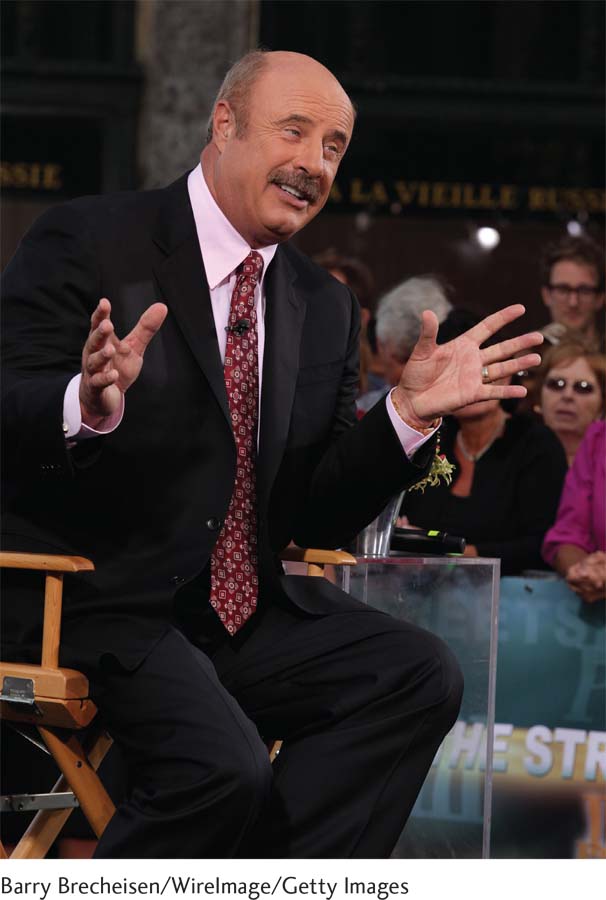
Psychologists are permitted to offer advice in self-
help books, on DVDs, on television and radio programs, in newspaper and magazines, and in other places, provided they do so responsibly and professionally and base their advice on appropriate psychological literature and practices. Psychologists are bound by these same ethical requirements when they offer advice and ideas online, whether on individual Web pages, blogs, bulletin boards, or chat rooms. Internet- based professional advice has proved difficult to regulate, however, because the number of such offerings keeps getting larger and larger and so many advice- givers do not appear to have any professional training or credentials. 545
Psychologists may not conduct fraudulent research, plagiarize the work of others, or publish false data. During the past 35 years cases of scientific fraud or misconduct have been discovered in all of the sciences, including psychology. These acts have led to misunderstandings of important issues, taken scientific research in the wrong direction, and damaged public trust. Unfortunately, the impressions created by false findings may continue to influence the thinking of both the public and other scientists for years.
Psychologists must acknowledge their limitations with regard to patients who are disabled or whose gender, ethnicity, language, socioeconomic status, or sexual orientation differs from that of the therapist. This guideline often requires psychotherapists to obtain additional training or supervision, consult with more knowledgeable colleagues, or refer clients to more appropriate professionals.
Psychologists who make evaluations and testify in legal cases must base their assessments on sufficient information and substantiate their findings appropriately. If an adequate examination of the individual in question is not possible, psychologists must make clear the limited nature of their testimony.
Psychologists may not take advantage of clients and students, sexually or otherwise. This guideline relates to the social problem of sexual harassment, as well as the problem of therapists who take sexual advantage of clients in therapy. The code specifically forbids a sexual relationship with a present or former therapy client for at least two years after the end of treatment—
and even then such a relationship is permitted only in “the most unusual circumstances.” Furthermore, psychologists may not accept as clients people with whom they have previously had a sexual relationship. Research has clarified that clients may suffer great emotional damage from sexual involvement with their therapists (Pope & Vasquez, 2016, 2011; Pope & Wedding, 2014). How many therapists actually have a sexual relationship with a client? On the basis of various surveys, reviewers have estimated that 4 to 5 percent of today’s therapists engage in some form of sexual misconduct with patients, down from 10 percent more than a decade ago.
Although the vast majority of therapists do not engage in sexual behavior of any kind with clients, their ability to control private feelings is apparently another matter. In surveys, more than 80 percent of therapists reported having been sexually attracted to a client, at least on occasion (Pope & Vasquez, 2016, 2011; Pope & Wedding, 2014). Although few of these therapists acted on their feelings, most of them felt guilty, anxious, or concerned about the attraction. Given such issues, it is not surprising that sexual ethics training is given high priority in many of today’s clinical training programs.
confidentiality The principle that certain professionals will not divulge the information they obtain from a client.
Psychologists must follow the principle of confidentiality. All of the state and federal courts have upheld laws protecting therapist confidentiality (Fisher, 2013; Nagy, 2011). For peace of mind and to ensure effective therapy, clients must be able to trust that their private exchanges with a therapist will not be repeated to others. There are times, however, when the principle of confidentiality must be compromised (Pope & Vasquez, 2016, 2011). A therapist in training, for example, must discuss cases on a regular basis with a supervisor, and clients must be informed that such discussions are taking place.

546
A second exception arises in cases of outpatients who are clearly dangerous. The 1976 case of Tarasoff v. Regents of the University of California, one of the most important cases to affect client–
Should confidentiality have been broken in this case? The therapist, in fact, felt that it should. Campus police were notified, but the patient was released after some questioning. In their suit against the hospital and therapist, the victim’s parents argued that the therapist should have also warned them and their daughter that the patient intended to harm Ms. Tarasoff. The California Supreme Court agreed: “The protective privilege ends where the public peril begins.”
duty to protect The principle that therapists must break confidentiality in order to protect a person who may be the intended victim of a client.
The current code of ethics for psychologists thus declares that therapists have a duty to protect—a responsibility to break confidentiality, even without the client’s consent, when it is necessary “to protect the client or others from harm.” Since the Tarasoff ruling, most states have passed “duty to protect” bills that clarify the rules of confidentiality for therapists and protect them from certain civil suits (Knoll, 2015).