INTRODUCTION: Understanding Psychological Disorders
KEY THEME
Understanding psychological disorders includes considerations of their origins, symptoms, and development, as well as how behavior relates to cultural and social norms.
KEY QUESTIONS
What is a psychological disorder, and what differentiates abnormal behavior from normal behavior?
What is DSM-
5, and how was it developed? How prevalent are psychological disorders?
Does the cartoon on the right make you smile? The cartoon is humorous, but it’s actually intended to make some serious points. It reflects several common misconceptions about psychological disorders that we hope to dispel in this chapter.
First, there’s the belief that “crazy” behavior is very different from “normal” behavior. Granted, sometimes it is, like Elyn’s bizarre pronouncements from the roof in front of her classmates. But as you’ll see throughout this chapter, the line that divides “normal” and “crazy” behavior is often not as sharply defined as most people think. In many instances, the difference between normal and abnormal behavior is a matter of degree. For example, as you leave your apartment or house, it’s normal to check or even double-
535
The dividing line between normal and abnormal behavior is also often determined by the social or cultural context in which a particular behavior occurs. For example, among traditional Hindus in India, certain dietary restrictions are followed as part of the mourning process. It would be a serious breach of social norms if an Indian widow ate fish, meat, onions, garlic, or any other “hot” foods within six months of her husband’s death. A Catholic widow in the United States would consider such restrictions absurd.
Second, when we encounter people whose behavior strikes us as weird, unpredictable, or baffling, it’s easy to simply dismiss them as “crazy,” as in the cartoon. Although convenient, such a response is too simplistic, not to mention unkind. It could also be wrong. Sometimes, unconventional people are labeled as crazy when they’re actually just creatively challenging the conventional wisdom with new ideas.

Even if a person’s behavior is seriously disturbed, labeling that person as “crazy” tells us nothing meaningful. What are the person’s specific symptoms? What might be the cause of the symptoms? How did they develop? How long can they be expected to last? And how might the person be helped? The area of psychology and medicine that focuses on these questions is called psychopathology—the scientific study of the origins, symptoms, and development of psychological disorders. In this chapter and the next, we’ll take a closer look at psychological disorders and their treatment.
Finally, there is still a strong social stigma attached to suffering from a psychological disorder (Ben-
What Is a Psychological Disorder?
What exactly are we talking about when we say that someone has a psychological or mental disorder? A psychological disorder or mental disorder can be defined as a pattern of behavioral or psychological symptoms that causes significant personal distress, impairs the ability to function in one or more important areas of life, or both (DSM-
What determines whether a given pattern of symptoms or behaviors qualifies as a psychological disorder? Throughout this chapter, you’ll notice numerous references to DSM-
536
DSM-
The first edition of the Diagnostic and Statistical Manual was published in 1952. With each new edition, the number of distinct disorders has progressively increased—
CRITICAL THINKING
Are People with a Mental Illness as Violent as the Media Portray Them?
Are people with a psychological disorder more violent than other people? When a heinous crime occurs, such as a mass shooting in a public place, people tend to react by assuming that the perpetrator “must be crazy.” Such statements may reflect the belief that mental illness and violent crime are closely linked. As Mary Camp and her colleagues (2010) write, “those categorized as mad are expected to be violent, unpredictable, or antisocial.”
In some cases, such as the 2012 shootings in an elementary school in Newtown, Connecticut, or the 2014 shootings near the University of California, Santa Barbara, the killers do have symptoms of mental disturbance. Yet the vast majority of violent crimes, even heinous ones, are committed by people who are not mentally ill. And another study found that symptoms of mental illness were not a strong predictor of criminal behavior (Peterson & others, 2014).
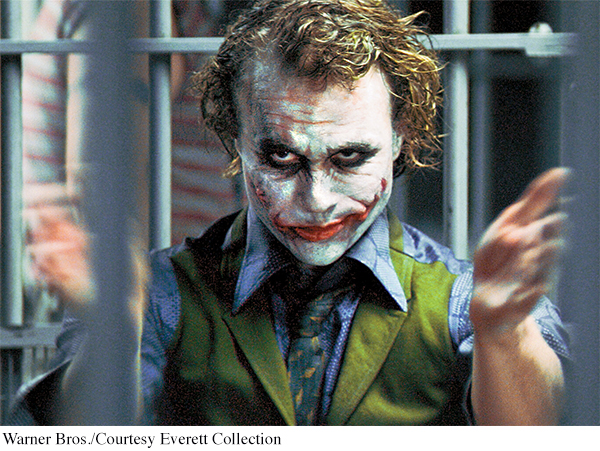
Multiple studies have found that people with a major mental illness belong to the most stigmatized group in modern society (Hinshaw & Stier, 2008; Schomerus & others, 2012). Substantial progress has been made in the understanding and treatment of psychological disorders. However, in much of the popular media, people with psychological disorders are still portrayed in highly negative, stereotyped ways (Klin & Lemish, 2008; Nairn & others, 2011). One stereotype is that of the mentally disturbed person as a helpless victim. The other stereotype is that of the mentally disordered person as an evil villain who is unpredictable, dangerous, and violent (Camp & others, 2010). For example, many of the criminals in the Batman series, including the Joker and the Riddler, end up imprisoned in the fictional Arkham Asylum for the Criminally Insane after they are captured (Daniels, 2008).
One comprehensive survey found that although 5 percent of “normal” television characters are murderers, 20 percent of “mentally ill” characters are killers (Gerbner, 1998). The same survey found that about 40 percent of “normal” characters were violent, but 70 percent of characters labeled as mentally ill were violent. This trend is also apparent in stories about real people. A study of Canadian news stories in 20 major newspapers over five years found that 40 percent of articles that discussed mental illness put it in the context of “danger, violence, or criminality” (Whitley & Berry, 2013). These media stereotypes reflect and reinforce the widespread belief among Americans that most people with mental illness are violent and threatening (Diefenbach & West, 2007).
This public perception that people with a mental illness are dangerous contributes to the stigma of mental illness (Fazel & others, 2009; Torrey, 2011). But let’s look at the evidence. Are people with mental disorders more violent than other people?
One groundbreaking study by psychologist Henry Steadman and his colleagues (1998) monitored the behavior of more than 1,000 former mental patients in the year after they were discharged from psychiatric facilities. For their control group, they also monitored a matched group of people who were not former mental patients but were living in the same neighborhood.
The researchers found that, overall, the former mental patients did not have a higher rate of violence than the comparison group. Former mental patients who demonstrated symptoms of substance use disorder were the most likely to engage in violent behavior. However, the same was also true of the control group. In other words, substance use disorder was associated with more violent behavior in all participants, whether they had a history of mental illness or not. The study also found that the violent behavior that did occur was most frequently aimed at friends and family members, not at strangers.
MYTH SCIENCE
Is it true that most people with a psychological disorder are violent?
Recent meta-
Canadian psychologist Kevin Douglas and his colleagues (2009) emphasize that the overall size of the association between psychosis and violence is relatively small. As they point out, “Most violent individuals are not psychotic, and most psychotic individuals are not violent.”
Clearly, the incidence of violent behavior among current or former mental patients is exaggerated in media portrayals. In turn, the exaggerated fear of violence from people with a psychological disorder contributes to the stigma of mental illness (Fazel & others, 2009). As psychologists Stephen Hinshaw and Andrea Stier (2008) emphasize, “Media depictions that routinely and inevitably link all forms of mental disorder with physical violence are stereotypic and inaccurate. Indeed, empirical data reveal that people with mental illness are far more likely to be victims of violent crime than are other individuals, and far more likely to be victims than to be perpetrators of violence.”
CRITICAL THINKING QUESTIONS
Can you think of any reasons why people with psychological disorders are more likely to be depicted as villains than members of other social groups?
Can you think of any television shows or movies in which characters with a severe psychological disorder were shown in a sympathetic light? If so, are such depictions more or less common than depictions of people with a mental illness as dangerous or violent?
What evidence could you cite to challenge the notion that people with psychological disorders are dangerous?
537
It’s important to understand that DSM-
Despite these efforts, DSM-
inclusion of some conditions that are too “normal” to be considered disorders, such as extreme sadness related to bereavement (Maj, 2012; Wakefield, 2013b; G. Watts, 2012)
use of arbitrary cutoffs to draw the line between people with and without a particular disorder, and even between different diagnoses (Caspi & others, 2014; J. Cohen & others, 2011; Insel, 2013; Laceulle & others, 2015)
gender bias (Marecek & Gavey, 2013; Yonkers & Clarke, 2011)
possible bias resulting from the financial ties of many DSM-
5 authors to the pharmaceutical industry, which might benefit from the expansion of mental illness categories or loosening of criteria for diagnoses (Cosgrove & Krimsky, 2012)
538
Finally, many critics believe that DSM-
Despite its flaws, DSM-
The Prevalence of Psychological Disorders
A 50–
MYTH SCIENCE
Is it true that psychological disorders are rare?
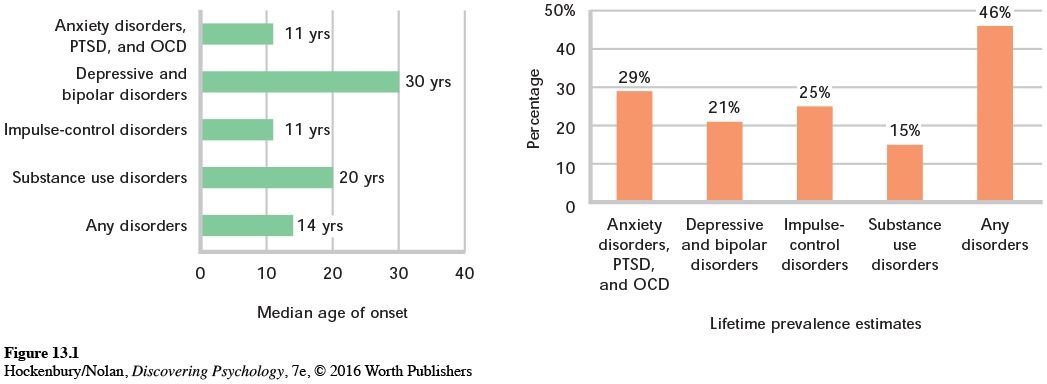
Just how common are psychological disorders? To investigate that question, researcher Ronald C. Kessler and his colleagues (2005a, 2005b) conducted a nationally representative survey of more than 9,000 Americans, ages 18 and older. Called the National Comorbidity Survey Replication (NCS-

The NCS-
Figure 13.1 shows the typical age of onset for some of the common mental disorders reported by the NCS-
Rates of mental illness are high not just in the United States, but also globally. In a large-
Although it might initially seem disturbing to think that one-
539
It wouldn’t surprise anyone if I said that 99.9% of the population had been physically ill at some time in their life. Why, then, should it surprise anyone that 50% of the population has been mentally ill at some time in their life? The reason, of course, is that we invest the term “mentally ill” with excess meaning. A number of common mental illnesses, like adjustment disorders and brief episodes of depression, are usually mild and self-
The NCS-

Think Like a SCIENTIST
Tracking the incidence of mental health problems is challenging. Can Internet searches reveal trends? Go to LaunchPad: Resources to Think Like a Scientist about Tracking Mental Illness Online.

It seems clear that many people who could benefit from mental health treatment don’t receive it. Several factors contribute to this unmet need, including lack of insurance, low income, and lack of access to mental health care, such as in developing countries or rural areas of developed countries (Santiago & others, 2013; Wang & others, 2011). Some people lack awareness about psychological disorders or shun treatment for fear of being stigmatized for seeking help with troubling psychological symptoms.
On the other hand, it also seems clear that most people manage to weather psychological symptoms without becoming completely debilitated and needing professional intervention (Mojtabai & others, 2011). One explanation for this is that people use a variety of coping strategies—
But it’s important to remember that even ineffective strategies can appear to be effective. Why? Because the symptoms of many psychological disorders, especially those involving mild to moderate symptoms, diminish with the simple passage of time or with improvements in the person’s overall situation. Nevertheless, there are many effective treatments available for psychological disorders that can produce improvements that occur much more quickly and endure longer. We’ll look at the different types of therapies used to treat psychological disorders in the next chapter.
540
For the remainder of this chapter, we’ll focus on psychological disorders in six DSM-
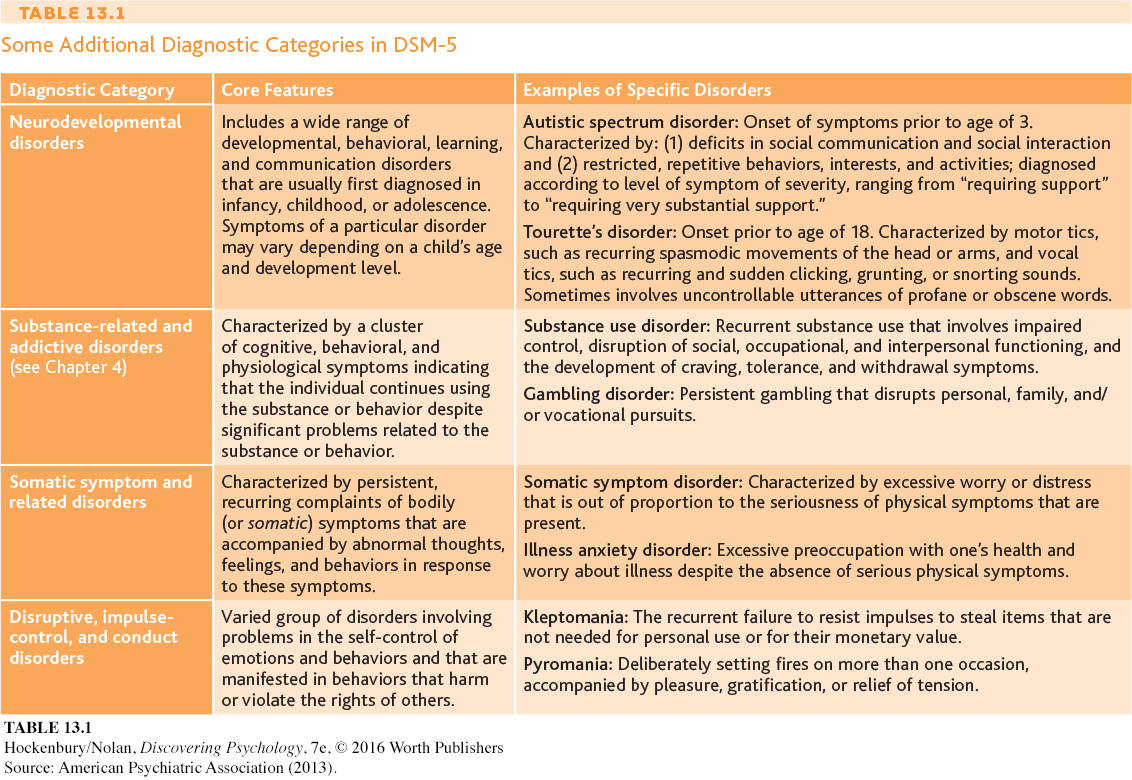
Table 13.1 describes other categories of mental disorders contained in the DSM-
Test your understanding of Understanding Psychological Disorders with  .
.